Abstract
Background
The indications for surgery in primary hyperparathyroidism (1HPT) are the same for patients with and without localization on imaging. However, patients with negative imaging may not be referred for surgery or the surgeon may be reluctant to operate. We compare outcomes in patients with negative imaging to those with localization.
Methods
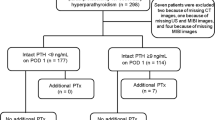
A review of patients who underwent primary operation for 1HPT with a preoperative Tc99 sestamibi I-123 (MIBI) scan was conducted. Imaging, laboratory, operative findings, pathologic findings, and outcomes were used to compare patients with negative scans to those with localization.
Results
A total of 2,681 patients had an operation for 1HPT with preoperative MIBI. MIBI imaging was negative in 136 (5.7 %). The negative MIBI group had a lower calcium (10.9 vs. 11.0 mg/ml, P = 0.02), phosphorus (2.9 vs. 3.1 mg/dl, P < 0.001), and urinary calcium (251 vs. 287 mg/ml, P = 0.02) and no difference in parathyroid hormone, 25-OH vitamin D, or bone loss. Multigland resection was higher with a negative scan (32 vs. 13 %, P < 0.001). A curative operation was performed in 90.4 % with a negative MIBI compared to 97.5 % with localization (P < 0.001). Patients who underwent successful surgery despite a negative MIBI scan had lower calcium (10.8 vs. 11.1 mg/ml, P = 0.04) and parathyroid hormone (98 vs. 196 pg/ml, P = 0.03) than those not cured. Patients with both a negative ultrasound result and negative MIBI had a cure rate of 89 %.
Conclusions
A curative operation is performed at an acceptably lower rate with negative MIBI imaging. A decision for surgery with a negative MIBI finding should consider lower cure rates and symptom severity.


Similar content being viewed by others
References
Irvin GL III, Carneiro DM, Solorzano CC. Progress in the operative management of sporadic primary hyperparathyroidism over 34 years. Ann Surg. 2004;239:704–11.
Van Heerden JA, Grant CS. Surgical treatment of primary hyperparathyroidism: an institutional perspective. World J Surg. 1991;15:688–92.
Van Heerden JA, Bearhrs OH, Wollner LB. The pathology and surgical management of primary hyperparathyroidism. Surg Clin North Am. 1977;57:557–63.
Rubin MR, Bilezikian JP, McMahon DJ, et al. The natural history of primary hyperparathyroidism with or without parathyroid surgery after 15 years. J Clin Endocrinol Metab. 2008;93:3462–70.
Coakley AJ, Ketlle AG, Wells CP, et al. 99Tcm-sestamibi—a new agent for parathyroid imaging. Nucl Med Commun. 1989;10:791–4.
Civelek AC, Ozalp E, Donovan P, et al. Prospective evaluation of delayed technetium-99 m sestamibi SPECT scintigraphy for preoperative localization of primary hyperparathyroidism. Surgery. 2002;131:149–57.
Sharma J, Mazzaglia P, Milas M, et al. Radionuclide imaging for hyperparathyroidism (HPT): which is the best technetium-99 m sestamibi modality? Surgery. 2006;140:856–63.
Norton KS, Johnson LW, Griffen FD, et al. The sestamibi scan as a preoperative screen tool. Am Surg. 2002;68:812–5.
Grant C, Thompson G, Farley D, Van Heerden J. Primary hyperparathyroidism surgical management since the introduction of minimally invasive parathyroidectomy. Arch Surg. 2005;140:472–8.
Arici C, Cheah WK, Ituarte PH, et al. Can localization studies be used to direct focused parathyroid operations? Surgery. 2001;129:720–9.
Wermers RA, Khosla S, Atkinson EJ, Achenbach SJ, Oberg AL, Grant CS. Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993–2001: an update on the changing epidemiology of the disease. J Bone Miner Res. 2006;21:171–7.
Proceedings of the NIDDK Workshop program. Asymptomatic primary hyperparathyroidism: a perspective for the 21st century. Bethesda, April 8–9, 2002. J Bone Miner Res. 2002;17(Suppl):N1–162.
AACE/AAES Task Force on Primary Hyperparathyroidism. American Association of Clinical Endocrinologists and the American Association of Endocrine Surgeons position statement on the diagnosis and management of primary hyperparathyroidism. Endocr Pract. 2005;11:49–54.
Bilezikian JP, Potts JT, Fuleihan Gel-H, et al. Summary statement from a workshop on asymptomatic primary hyperparathyroidism: a perspective for the 21st century. J Clin Endocrinol Metab. 2002;87:5353–61.
Lew JI, Rivera M, Irvin GL 3rd, Solorzano CC. Operative failure in the era of focused parathyroidectomy. Arch Surg. 2010;145:628–33.
Siperstein A, Berber E, Barbosa GF, et al. Predicting the success of limited exploration for primary hyperparathyroidism using ultrasound, sestamibi, and intraoperative parathyroid hormone: analysis of 1158 cases. Ann Surg. 2008;248:420–8.
Solorzano CC, Lee TM, Ramirez MC, et al. Surgeon performed ultrasound improves localization of abnormal parathyroid glands. Am Surg. 2005;71:557–62.
Kebapci M, Entok E, Kebapci N, et al. Preoperative evaluation of parathyroid lesions in patients with concomitant thyroid disease: role of high resolution ultrasonography and dual phase technetium 99 m sestamibi scintigraphy. J Endocrinol Invest. 2004;27:24–30.
Bergenfelz AO, Wallin G, Jansson S, et al. Results of surgery for sporadic primary hyperparathyroidism in patients with preoperatively negative sestamibi scintigraphy and ultrasound. Langenbecks Arch Surg. 2011;396:83–90.
Rodgers SE, Hunter GJ, Hamberg LM, et al. Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery. 2006;140:932–4.
Starker LF, Mahajan A, Björklund P, Sze G, Udelsman R, Carling T. 4D parathyroid CT as the initial localization study for patients with de novo primary hyperparathyroidism. Ann Surg Oncol. 2011;18:1723–8.
Silverberg SJ, Shane E, Jacobs TP, Siris E, Bilezikian JP. A 10-year prospective study of primary hyperparathyroidism with or without parathyroid surgery. N Engl J Med. 1999;341:1249–55.
Conflict of interest
All authors have no conflict interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dy, B.M., Richards, M.L., Vazquez, B.J. et al. Primary Hyperparathyroidism and Negative Tc99 Sestamibi Imaging: To Operate or Not?. Ann Surg Oncol 19, 2272–2278 (2012). https://doi.org/10.1245/s10434-012-2325-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-012-2325-3