Abstract
Interferon (IFN)-α is a cytokine of the innate immune response that is well known for inducing behavioral alterations and has been used to study effects of cytokines on the nervous system. Limited data, however, are available on the sites of action of IFN-α within the brain and their relationship with specific IFN-α-induced symptoms. Using a longitudinal design, whole-brain metabolic activity as assessed by fluorine-18-labeled fluorodeoxyglucose uptake and positron emission tomography was examined before and 4 weeks after IFN-α administration in patients with malignant melanoma. Changes in metabolic activity in relevant brain regions were then correlated with IFN-α-induced behavioral changes. IFN-α administration was associated with widespread bilateral increases in glucose metabolism in subcortical regions including the basal ganglia and cerebellum. Decreases in dorsal prefrontal cortex glucose metabolism were also observed. Prominent IFN-α-induced behavioral changes included lassitude, inability to feel, and fatigue. Correlational analyses revealed that self-reported fatigue (specifically as assessed by the ‘energy’ subscale of the Visual Analog Scale of Fatigue) was associated with increased glucose metabolism in the left nucleus accumbens and putamen. These data indicate that IFN-α as well as other cytokines of the innate immune response may target basal ganglia nuclei, thereby contributing to fatigue-related symptoms in medically ill patients.
Similar content being viewed by others
INTRODUCTION
Recent data suggest that behavioral changes in medically ill patients with chronically activated innate immunity arise in part through effects of peripheral inflammatory processes on the brain (Dantzer, 2001; Lee et al, 2004; Raison et al, 2006). Indeed, tissue damage and destruction (as occurs in a variety of medical disorders and their treatment) activate innate/inflammatory immune responses and lead to the release of cytokines, including interferon (IFN)-α, interleukin (IL)-1, IL-6, and tumor necrosis factor (TNF)-α. All of these cytokines can access the brain and have profound effects on neurotransmitter metabolism, neuroendocrine function, synaptic plasticity, and behavior (Konsman et al, 2002; Raison et al, 2006). To further elucidate nervous system pathways that may be implicated in cytokine-induced effects on the brain in humans, specifically the anatomical loci involved, our group and others have studied patients undergoing treatment with IFN-α (Capuron and Miller, 2004).
IFN-α is currently used for the treatment of certain viral illnesses and cancers, including chronic hepatitis C and malignant melanoma. Although a successful antiviral and antineoplastic strategy, IFN-α causes a host of neuropsychiatric symptoms, including depression, cognitive dysfunction, and fatigue in a large proportion of patients (Capuron et al, 2002a; Capuron and Miller, 2004; Musselman et al, 2001; Pavol et al, 1995). Thus, IFN-α provides a unique opportunity to study the effects of cytokines on the brain. Previous studies have found that neuropsychiatric symptoms that develop during IFN-α therapy for malignant melanoma appear to represent at least two distinct behavioral syndromes with distinct phenomenology and responsiveness to antidepressants: a mood/cognitive syndrome, including depressed mood, anxiety, and attentional and memory alterations, and a neurovegetative syndrome, including fatigue (the most common IFN-α-induced symptom), anorexia, psychomotor slowing, and sleep disturbances (Capuron et al, 2002a; Maddock et al, 2005). The neurovegetative syndrome typically occurs within the first 4 weeks of therapy, persists into later stages of treatment, and has been minimally responsive to the antidepressant paroxetine (Capuron et al, 2002a; Maddock et al, 2005). In contrast, the mood/cognitive syndrome, which develops in a smaller proportion of patients and occurs at later stages of IFN-α treatment, has been shown to be highly responsive to paroxetine administration (Capuron et al, 2002a; Capuron and Miller, 2004; Musselman et al, 2001). These data suggest that different pathophysiological mechanisms mediate neurovegetative vs mood/cognitive effects of IFN-α.
Studies by our group and others have indicated that hyperactivity of stress-responsive neuroendocrine pathways and disturbances in serotonin metabolism may participate in the development of the mood/cognitive syndrome during IFN-α therapy (Bonaccorso et al, 2002; Capuron and Miller, 2004; Capuron et al, 2002b, 2003a, 2003b). In addition, using functional magnetic resonance imaging, we recently reported that IFN-α-induced alterations in information processing as reflected by increased activation in the dorsal anterior cingulate cortex during a task of visuo-spatial attention may also contribute to mood and anxiety symptoms (Capuron et al, 2005). Finally, previous work demonstrated a relationship between decreased prefrontal cortex glucose metabolism and depression scores in patients receiving 12 weeks of IFN-α for treatment of hepatitis C (Juengling et al, 2000). Little is known, however, about the neurobiological mechanisms and anatomical loci underlying IFN-α-induced neurovegetative symptoms, including fatigue.
Recent data suggest that IFN-α's effects on the development of fatigue and other neurovegetative symptoms may be related to alterations in the activity of subcortical brain regions, notably the basal ganglia, and dopaminergic transmission (Capuron and Miller, 2004). Indeed, Parkinson-like symptoms observed in patients receiving IFN-α for chronic hepatitis C (Horikawa et al, 1999) were reversed by intravenous administration of levodopa (Sunami et al, 2000). In addition, a positron emission tomography (PET) study with fluorine-18-labeled fluorodeoxyglucose (18F-FDG) in patients with chronic hepatitis C revealed that treatment with IFN-α was associated with glucose hypermetabolism in the putamen, a basal ganglia structure (Juengling et al, 2000), although the relationship of these changes with specific behavioral symptoms was not examined. Finally, experimental data in mice have shown that chronic treatment with IFN-α is associated with depletion of central nervous system dopamine concentrations in whole brain homogenates (Shuto et al, 1997).
To further evaluate the specific sites of action of IFN-α in the brain and examine the relationship between changes in regional brain activity and specific symptoms associated with IFN-α therapy, especially fatigue, we conducted a PET study assessing resting state cerebral glucose metabolism in patients with malignant melanoma devoid of metastatic disease and pre-existing behavioral alterations. PET scanning was performed at baseline (before IFN-α treatment) and again after 4 weeks of IFN-α therapy. Four weeks was chosen because it is a time point at which neurovegetative symptoms including fatigue are more prominent relative to other (eg mood/cognitive) symptoms. Neuropsychiatric symptoms were quantified using the Montgomery Asberg Depression Rating Scale (MADRS) (Montgomery and Asberg, 1979) and the Visual Analogue Scale of Fatigue (VAS-F) (Lee et al, 1991).
METHODS AND MATERIALS
Subjects
Using a longitudinal design, two PET scans (before and after 4 weeks of IFN-α therapy) were performed in a total of 12 right-handed patients [nine men, three women, mean age 49 (SD 9) years] diagnosed with stage II–IV malignant melanoma with a 50% or greater risk of recurrence. All patients had been surgically rendered clinically free of disease and were eligible to receive high-dose IFN-α therapy. Patients were recruited from the Winship Cancer Institute at Emory University. Medical exclusion criteria included diabetes; unstable cardiovascular, endocrine, hematological, hepatic, or renal disease; brain damage and/or neoplastic involvement; neurological disease; and severe or uncontrolled visual disturbances. Patients with a diagnosis of schizophrenia, bipolar disorder, or current major depression as determined by Structured Clinical Interview for DSM-IV Axis I disorders (Association, 1994); a Mini Mental State Exam ⩽24 (Folstein et al, 1983); or active treatment with antipsychotics, antidepressants, or benzodiazepines were also excluded. All patients were offered antidepressant treatment to prevent depression during IFN-α administration, and all declined. IFN-α2b (IntronA, Schering-Plough) was administered intravenously at a dose of 20 million units per square meter of body-surface area 5 days/week for 4 weeks. Concomitant medications for fever and nausea due to IFN-α administration were allowed during the study, but psychotropic medications, including antipsychotics, antidepressants, and benzodiazepines, were not.
All patients were adults and provided written informed consent before enrollment. The study was approved by the Institutional Review Board of the Emory University School of Medicine.
Behavioral Assessments
Behavioral assessments were performed at baseline (before the initiation of IFN-α therapy) and after 4 weeks of IFN-α treatment. Assessments included the observer-rated MADRS (Montgomery and Asberg, 1979), a 10-item scale assessing the severity of depressive symptoms, including sadness, inner tension, concentration difficulties, inability to feel (defined as reduced interest in surroundings and usually pleasurable activities and/or reduced emotional responsivity), pessimistic thoughts, suicidal thoughts, reduced sleep, reduced appetite, and lassitude (defined as difficulty getting started or slowness initiating and performing everyday activities). Based on previous work indicating that fatigue is the most prominent IFN-α-induced symptom (Capuron et al, 2002a), subjects were also administered the self-report VAS-F, an 18-item 100-mm visual analogue scale, which assesses fatigue using two series of inverse items: a ‘fatigue’ series (13 items including ‘tired’, ‘sleepy’, ‘drowsy’, ‘fatigued’, ‘worn out’, ‘bushed’, ‘exhausted’, difficulty ‘keeping eyes open’, difficulty ‘moving my body’, difficulty ‘concentrating’, difficulty ‘carrying on a conversation’, ‘desire to close my eyes’, ‘desire to lie down’) and an ‘energy’ series (five items including ‘energetic’, ‘active’, ‘vigorous’, ‘efficient’, ‘lively’), which together represent ‘fatigue’ and ‘energy’ subscales (Lee et al, 1991). The VAS-F has been shown to possess good overall psychometric properties (Lee et al, 1991; Meek et al, 2000; Miaskowski and Lee, 1999), although in a comparison of multiple fatigue instruments and their subscales (see below), the energy subscale of the VAS-F was found to exhibit the highest reliability in measuring fatigue-related symptoms in cancer patients (Meek et al, 2000).
Changes in behavioral scores between baseline and week 4 of IFN-α therapy were assessed using paired t-tests with Bonferroni correction for multiple comparisons.
Acquisition of PET Data
Patients underwent two PET scans, one before the initiation of IFN-α therapy (baseline assessment) and one at the end of the fourth week of IFN-α therapy. All patients were asked to fast for at least 4 h before each scan.
PET measures of regional cerebral glucose metabolism (rCMRGlc) were acquired in the rest condition (patients were asked to lie quietly with eyes closed) following the intravenous injection of 9–10 mCi of fluorine-18-labeled fluorodeoxyglucose ([18]FDG) via a catheter inserted in an arm vein.
Forty-five minutes after tracer injection, brain images were acquired as a single 25-min frame study in two-dimensional acquisition mode using an ECAT 951 tomograph (Siemens, Knoxville, TN), with a voxel size of 2.574 × 2.574 × 3.375 mm.
PET Data Analysis
For each patient, the PET image obtained at 4 weeks of IFN-α therapy was spatially registered to the image acquired at baseline. Images were then spatially transformed to a FDG brain template conforming to the Montreal Neurological Institute (MNI) reference brain, resampled at a 2 × 2 × 2 mm voxel size, and subsequently smoothed with an isotropic Gaussian kernel of 12 mm FWHM. An MNI probabilistic map of brain tissue (included in the SPM2 software distribution, Wellcome Department of Cognitive Neurology, University College, London, UK) was thresholded at p=0.4 to generate a mask excluding voxels outside the brain. The smoothed FDG images were then multiplied by the latter mask and intensity-normalized to an average reference value of 100 across in-brain voxels, in order to correct for global difference intensity across images.
Whole-Brain Analysis
A whole-brain analysis, using a voxel-wise paired t-test, was performed to assess relative changes in rCMRGlc across the brain between baseline and 4 weeks of IFN-α therapy. Analysis was performed with the software package AFNI (Cox, 1996). The specified experiment-wise (ie corrected for multiple comparisons) alpha level <0.05 was reached by the combination of the single-voxel threshold of p=0.0001 and a cluster size threshold of 78 voxels, as determined by a Monte Carlo simulation performed with the AFNI routine AlphaSim (Forman et al, 1995).
Regions of Interest Analysis
Because of previous data implicating subcortical structures in IFN-α-induced behavioral symptoms, notably the basal ganglia, the change in rCMRGlc evidenced by whole-brain analysis was further investigated by partitioning the whole-brain activation clusters according to their location within specific basal ganglia nuclei: left and right putamen, left and right globus pallidus, and left and right nucleus accumbens (no activation cluster was present in the region of the caudate nucleus). These regions of interest were anatomically defined according to the digital version of the Talairach atlas included in the software package AFNI (Cox, 1996).
Analysis of PET and Behavioral Data
Correlational analyses were performed to characterize the relationship between the change in glucose metabolism in neuroanatomical locations significantly altered during IFN-α therapy (according to the whole-brain analysis) and the behavioral symptoms that were significantly changed during IFN-α treatment. To protect against Type I errors, only statistically significant (p<0.05, two-sided) correlation coefficients reflecting a large effect size (r⩾0.50) were considered meaningful (Cohen, 1988). Where indicated, age and sex were entered into the analyses as covariates.
RESULTS
Changes in Brain Glucose Metabolism during IFN-α Therapy: Whole-Brain Analysis
Significant and widespread increases in resting state rCMRGlc were measured after 4 weeks of IFN-α therapy in one extended subcortical cluster, which included the bilateral putamen, globus pallidus, nucleus accumbens, pulvinar, and the left amygdala (Figure 1 and Table 1). Distinct increases in rCMRGlc were also noted in the right putamen and in a large portion of the cerebellum. Small regions of decreased rCMGLc were observed in the left and right dorsal prefrontal cortex.
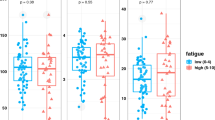
Changes in regional brain glucose metabolism during IFN-α therapy. Whole-brain metabolic activity was assessed using positron emission tomography before and 4 weeks after IFN-α administration in 12 patients with malignant melanoma devoid of metastatic disease or pre-existing behavioral alterations. Whole-brain glucose metabolism was estimated by fluorine-18-labeled fluorodeoxyglucose uptake while subjects were at rest. Statistical threshold was set up at an experiment-wise alpha<0.05, with psingle−voxel=0.0001 and cluster size=78 voxels. Images are displayed as coronal brain sections with blue regions representing decreases in metabolic activity and yellow representing increases. L (left) and R (right) orientation of the images are indicated as are relevant Broadman areas (BA) in the prefrontal cortex. Correlations between changes (delta) in regional cerebral glucose metabolism (rCMRGLc) in the left putamen and left nucleus accumbens (relative to baseline) and changes (delta) in ‘energy’ subscale scores as measured by the Visual Analogue Scale of Fatigue (VAS-F) during IFN-α therapy (R=−0.622, p=0.03 and R=−0.669, p=0.02, respectively) are also depicted. Increased metabolic activity in these basal ganglia nuclei were associated with decreases in energy subscale scores during IFN-α therapy.
Symptom Development during IFN-α Therapy
IFN-α therapy for 4 weeks was associated with significant changes in scores on the MADRS and VAS-F (Table 2). Whereas total scores on the MADRS and VAS-F subscale of fatigue significantly increased, VAS-F energy subscale scores significantly decreased. Consistent with data on the VAS-F, MADRS items exhibiting statistically significant change during IFN-α treatment included inability to feel and lassitude, both of which are associated with the symptom dimensions of fatigue/decreased energy. Given the overlap of the constructs of fatigue as measured by the VAS-F with the single items of inability to feel and lassitude on the MADRS, we chose the more nuanced VAS-F subscales for subsequent correlations with brain metabolism.
Changes in Brain Metabolic Activity during IFN-α Therapy: Relationship of Behavioral Changes with Specific Anatomical Locations
As shown in Table 3 and Figure 1, increased activity in basal ganglia nuclei at 4 weeks of IFN-α therapy (relative to baseline) correlated with VAS-F energy subscale scores. More specifically, VAS-F energy subscale scores during IFN-α therapy were negatively correlated with glucose metabolic activity in the left putamen and left nucleus accumbens (R=−0.622, p=0.03 and R=−0.669, p=0.02, respectively) (Figure 1). Entry of age and sex as covariates in these analyses did not appreciably change the significance of the results for either the putamen (p=0.04) or the accumbens (p=0.03). VAS-F subscale scores of fatigue did not correlate with any specific basal ganglia region identified in the study. Moreover, no significant correlations were observed between VAS-F subscale scores and any other brain region that was significantly altered by IFN-α administration (all p>0.05 and r<0.50) (Table 3). Correlational analyses also failed to reveal significant correlations between brain regions with IFN-α-induced alterations in metabolic activity and total MADRS scores (data not shown).
DISCUSSION
The present findings indicate that a 4-week course of IFN-α administration is associated with marked and extensive increases in glucose metabolism in subcortical brain regions, notably the basal ganglia, as well as the cerebellum. Smaller areas of decreased regional glucose metabolism were noted in the dorsal prefrontal cortex. In addition, IFN-α administration was associated with significant increases in behavioral symptoms that included lassitude, inability to feel, and fatigue. Correlational analyses indicated that increased glucose metabolism in the basal ganglia, specifically the left putamen and nucleus accumbens, significantly correlated with the development of IFN-α-induced fatigue symptoms, specifically as assessed by the energy subscale of VAS-F.
As previously mentioned, data from clinical and laboratory animal research have provided considerable evidence that IFN-α, as well as other cytokines, may alter the function of basal ganglia circuits (Horikawa et al, 1999; Kamata et al, 2000; Kumai et al, 2000; Shuto et al, 1997; Sunami et al, 2000). Our results are consistent with these observations and suggest that increased basal ganglia resting state glucose metabolism in IFN-α-treated patients may be indicative of altered dopaminergic activity, as is seen in patients with Parkinson's disease (PD). Increased glucose metabolism in the basal ganglia (as seen following IFN-α administration) has been repeatedly demonstrated in PD patients (Eidelberg et al, 1994; Mentis et al, 2002; Spetsieris et al, 1995), where it is believed to reflect the degeneration of inhibitory neurocircuits related to the loss of dopaminergic neurons in the substantia nigra pars compacta (Wichmann and DeLong, 2003). Disinhibition of dopaminergic inhibitory neurocircuits in turn leads to increased oscillatory burst activity in relevant basal ganglia nuclei (and thus increased metabolic activity) (Wichmann and DeLong, 1999). Relevant to the role of diminished dopamine availability in basal ganglia hyperactivity, levodopa infusion has been shown to reduce glucose metabolism in the basal ganglia, notably in the putamen, and is associated with clinical improvement in PD patients (Feigin et al, 2001). Given the role of dopamine pathways in activating frontal cortex neurons (Alexander et al, 1986), altered basal ganglia and dopamine function may also contribute to the reduced metabolic activity observed in the frontal cortex following IFN-α administration. Such decreases in frontal cortex activity also have been found in PD patients, especially in those with depression (Mayberg et al, 1990).
Additional support regarding IFN-α's effects on the basal ganglia and dopamine pathways is provided by the strong implication of basal ganglia function in pathological fatigue (Chaudhuri and Behan, 2000). Fatigue represents a fundamental behavioral characteristic of diseases that affect the basal ganglia, including PD, multiple sclerosis, cortical stroke, and HIV/AIDS (Chaudhuri and Behan, 2000; Gray et al, 2001; Lou et al, 2001) Moreover, it has been suggested that reduced nucleus accumbens dopamine may contribute to symptoms of fatigue in patients with depression (Salamone et al, 2003, 2005). Treatment with levodopa or other pharmacologic agents that increase dopamine release (eg stimulants) has been shown to improve fatigue in patients with basal ganglia disorders as well as in IFN-α-treated patients with malignant melanoma (Lou et al, 2003; Schwartz et al, 2002). Taken together, these findings suggest that changes in basal ganglia activity during IFN-α therapy may be related to altered dopamine neurotransmission and in turn play a role in the pathophysiology of IFN-α-induced fatigue-related symptoms.
Patients with immune-based disorders, including cancer and viral infections, commonly report symptoms of fatigue. Recent data suggest that cytokines released during activation of innate immunity may participate in the development of fatigue-related symptoms in these medically ill patients (Bower et al, 2002; Cleeland et al, 2003; Lee et al, 2004; Meyers et al, 2005). Our findings with IFN-α are consistent with these notions and extend the potential mechanisms to include cytokine effects on the basal ganglia. The basal ganglia have been particularly vulnerable to immune activation. Indeed, several infectious diseases, including HIV/AIDS, have been associated with basal ganglia alterations and fatigue (Berger and Arendt, 2000; von Giesen et al, 2005). Interestingly, in these diseases both basal ganglia hypermetabolism and hypometabolism have been observed, possibly related to the duration of pathogen exposure and/or the chronicity of the disease. For example, in HIV/AIDS, data have suggested that early stages of neurologic involvement are characterized by basal ganglia hypermetabolism followed by basal ganglia hypometabolism, possibly reflective of neurodegeneration (von Giesen et al, 2000). Such data suggest that, while 4 weeks of IFN-α administration was associated with basal ganglia hypermetabolism, more chronic exposure to this or other cytokines may lead to degeneration of basal ganglia neurons and basal ganglia hypometabolism. Studies examining more long-term consequences of IFN-α are needed to address these possibilities as well as the reversibility of the effects.
Further supporting the involvement of innate immune cytokines in basal ganglia pathology, diseases involving the basal ganglia, notably PD, have exhibited increased expression of proinflammatory cytokines in basal ganglia circuitry, and the development of PD in animal models using N-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine is in part dependent on expression of the proinflammatory cytokine, TNF-α (Leng et al, 2005; Nagatsu and Sawada, 2005). Of note, relevant receptors for proinflammatory cytokines are expressed in abundance in the basal ganglia (Gray et al, 2001; Haas and Schauenstein, 1997), and chronic infusion of lipopolysaccharide, a potent inducer of the proinflammatory cytokine cascade, into the rat brain has been shown to induce a progressive and selective degeneration of nigral dopaminergic neurons through microglial activation (Gao et al, 2002). More specifically related to IFN-α, IFN-α receptors have been identified throughout the brain especially in microglia (Yamada and Yamanaka, 1995). IFN-α-induced activation of microglia may in turn lead to the release of proinflammatory cytokines, such as TNF-α, which, as noted above, may contribute to alterations in basal ganglia function through local inflammation and neuronal damage. In addition, previous studies have shown that IFN-α can bind to opioid receptors (Wang et al, 2006), which are richly expressed in brain regions that exhibited increased metabolic activity in the current study, including the basal ganglia (Baumgartner et al, 2006). Moreover, opioids have been shown to influence dopamine release in the ventral striatum through a calcium-dependent mechanism (McGinty, 1999). Taken together, the data suggest that the basal ganglia may be a relevant and specific target for the effects of cytokines on the brain, inducing behavioral changes that include fatigue-related symptoms.
Another finding in the current study was the profound IFN-α-induced increase in glucose metabolic activity in the cerebellum. This finding has not been previously described and may relate to a specific targeting of the cerebellum by IFN-α or a preferential increase in cerebellar blood–brain-barrier (BBB) permeability as a function of chronic IFN-α exposure. In studies of transgenic mice with CNS hyper-expression of IFN-α, the brain regions exhibiting the most dramatic neuropathological changes were the cerebellum and basal ganglia (Campbell et al, 1999). In addition, compared with the cerebral cortex, the cerebellum exhibited a significantly greater loss of BBB integrity as well as up-regulation of relevant adhesion molecules during a non-pathogenic CNS viral infection, suggesting that regional differences in BBB permeability may occur in the context of exposure to certain viruses or antiviral cytokines, such as IFN-α (Phares et al, 2006). Regarding the functional implications of IFN-α effects on the cerebellum, there is increasing evidence for a role of the human cerebellum in processing speed and accuracy for tasks that have already become automated (Ramnani, 2006). These more cognitive aspects of cerebellar function appear to involve a closed cortico-pontine-cerebellar loop from Brodmann areas 9 and 46 in the prefrontal cortex, to the pons, to the ventral dentate nucleus in the cerebellum, and back to the prefrontal cortex via the thalamus. This circuit, especially aspects involving cerebellar and cortical (Brodmann areas 9 and 46) components, appears to be well represented in our data. An intriguing possibility is that a dysfunction of this loop (as may occur during IFN-α administration) could result in a mismatch between expected and actual consequences of actions, which would require constant (if subtle) corrective readjustments even for automated everyday tasks, a situation that could contribute to an increase in synaptic activity and the experience of fatigue (or lack of energy). Nevertheless, as indicated above, it is important to consider the equal or more likely possibility that the increased glucose metabolism in the cerebellum (as well as other relevant brain regions) may be directly related to inflammatory processes (manifested by increased glycolysis) (Bakheet and Powe, 1998), a situation that could also cause an inflammation-induced increase in regional blood flow, probably best detected using H215O-PET imaging. This notion is especially relevant in view of the evidence of a specific vulnerability of the cerebellum to IFN-α administration as discussed above.
In contrast to the results of a previous study, we did not observe a relationship between IFN-α-induced changes in prefrontal cortex glucose metabolism and symptoms of depression, despite a similar number of subjects (Juengling et al, 2000). This finding may relate to our study design, which, as noted previously, purposely sampled subjects after 4 weeks of IFN-α therapy, when neurovegetative symptoms including fatigue are prominent. Based on our previous data (Capuron et al, 2002a; Raison et al, 2005), longer periods of IFN-α treatment are required to allow the full emergence of mood and cognitive symptoms, which may in turn be correlated with changes in metabolic activity in other brain regions including the prefrontal cortex. Moreover, in a study by Capuron et al, psychomotor slowing—a behavioral sign that often accompanies altered basal ganglia function—was predictive of subsequent depressive symptoms, suggesting that IFN-α-induced effects on the basal ganglia may precede changes in prefrontal cortical function and their effects on behavior (Capuron et al, 2001).
Finally, at least two limitations in the study methodology should be considered. First, the study included a relatively small number of subjects, which possibly contributed to the inability to detect a significant relationship between basal ganglia activity and VAS-F fatigue subscale scores as well as other potential brain–behavior relationships during IFN-α administration. Nevertheless, as noted above, compared to the VAS-F energy subscale, the VAS-F fatigue subscale has been found to exhibit reduced stability and effect size compared with the energy subscale in a recent study focused on validating psychometric instruments for fatigue-related symptoms in cancer patients (Meek et al, 2000). Indeed, in this study, among all the instruments (and their subscales) examined, including the Profile of Mood States short-form fatigue subscale, Multidimensional Assessment of Fatigue, the Multidimensional Fatigue Inventory, and the VAS-F scale, the VAS-F energy subscale was one of only two subscales that met satisfactory levels of test–retest reliability in cancer patients. Nevertheless, future studies with a larger population of subjects assessed at several time points may be required to observe more subtle relationships between alterations in metabolic activity in specific brain regions and IFN-α-induced behavioral changes, which have been found to evolve over time. Second, there was no control group that underwent FDG-PET scanning and symptom assessments in parallel with the IFN-α-treated subjects. Nevertheless, measures of regional cerebral glucose metabolism during rest exhibit a reasonable degree of reproducibility (Bartlett et al, 1988; Maquet et al, 1990), and thus the rCMRGlc differences observed during IFN-α treatment are unlikely to be secondary to a systematic test–retest effect. Despite the limitations, few studies have addressed the relationship between regional brain changes and cytokine administration in humans, and the study therefore serves as an important first step in addressing potential neural circuits as targets for further research and symptom management in these individuals. In addition, although the data reported herein derive from patients undergoing IFN-α treatment for malignant melanoma, the results of the study may extend to other populations of patients or individuals in whom chronic activation of innate immune cytokines and their signaling pathways may alter basal ganglia circuitry as well as dopamine neurotransmission to induce fatigue-related symptoms.
References
Alexander GE, DeLong MR, Strick PL (1986). Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annu Rev Neurosci 9: 357–381.
Association AP (1994). Diagnostic and Statistical Manual of Mental Disorders, 4th edn. American Psychiatric Association: Washington, DC.
Bakheet SM, Powe J (1998). Benign causes of 18-FDG uptake on whole body imaging. Semin Nucl Med 28: 352–358.
Bartlett EJ, Brodie JD, Wolf AP, Christman DR, Laska E, Meissner M (1988). Reproducibility of cerebral glucose metabolic measurements in resting human subjects. J Cereb Blood Flow Metab 8: 502–512.
Baumgartner U, Buchholz HG, Bellosevich A, Magerl W, Siessmeier T, Rolke R et al (2006). High opiate receptor binding potential in the human lateral pain system. Neuroimage 30: 692–699.
Berger JR, Arendt G (2000). HIV dementia: the role of the basal ganglia and dopaminergic systems. J Psychopharmacol 14: 214–221.
Bonaccorso S, Marino V, Puzella A, Pasquini M, Biondi M, Artini M et al (2002). Increased depressive ratings in patients with hepatitis C receiving interferon-alpha-based immunotherapy are related to interferon-alpha-induced changes in the serotonergic system. J Clin Psychopharmacol 22: 86–90.
Bower JE, Ganz PA, Aziz N, Fahey JL (2002). Fatigue and proinflammatory cytokine activity in breast cancer survivors. Psychosom Med 64: 604–611.
Campbell IL, Krucker T, Steffensen S, Akwa Y, Powell HC, Lane T et al (1999). Structural and functional neuropathology in transgenic mice with CNS expression of IFN-alpha. Brain Res 835: 46–61.
Capuron L, Gumnick JF, Musselman DL, Lawson DH, Reemsnyder A, Nemeroff CB et al (2002a). Neurobehavioral effects of interferon-alpha in cancer patients: phenomenology and paroxetine responsiveness of symptom dimensions. Neuropsychopharmacology 26: 643–652.
Capuron L, Miller AH (2004). Cytokines and psychopathology: lessons from interferon-alpha. Biol Psychiatry 56: 819–824.
Capuron L, Neurauter G, Musselman DL, Lawson DH, Nemeroff CB, Fuchs D et al (2003a). Interferon-alpha-induced changes in tryptophan metabolism. Relationship to depression and paroxetine treatment. Biol Psychiatry 54: 906–914.
Capuron L, Pagnoni G, Demetrashvili M, Woolwine BJ, Nemeroff CB, Berns GS et al (2005). Anterior cingulate activation and error processing during interferon-alpha treatment. Biol Psychiatry 58: 190–196.
Capuron L, Raison CL, Musselman DL, Lawson DH, Nemeroff CB, Miller AH (2003b). Association of exaggerated HPA axis response to the initial injection of interferon-alpha with development of depression during interferon-alpha therapy. Am J Psychiatry 160: 1342–1345.
Capuron L, Ravaud A, Dantzer R (2001). Timing and specificity of the cognitive changes induced by interleukin-2 and interferon-alpha treatments in cancer patients. Psychosom Med 63: 376–386.
Capuron L, Ravaud A, Neveu PJ, Miller AH, Maes M, Dantzer R (2002b). Association between decreased serum tryptophan concentrations and depressive symptoms in cancer patients undergoing cytokine therapy. Mol Psychiatry 7: 468–473.
Chaudhuri A, Behan PO (2000). Fatigue and basal ganglia. J Neurol Sci 179: 34–42.
Cleeland CS, Bennett GJ, Dantzer R, Dougherty PM, Dunn AJ, Meyers CA et al (2003). Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism?. A cytokine-immunologic model of cancer symptoms. Cancer 97: 2919–2925.
Cohen JD (1988). Statistical Power Analysis for the Behavioral Sciences, 2nd edn. Lawrence Erlbaum Associates: Hillsdale, NJ.
Cox RW (1996). AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Comput Biomed Res 29: 162–173.
Dantzer R (2001). Cytokine-induced sickness behavior: mechanisms and implications. Ann NY Acad Sci 933: 222–234.
Eidelberg D, Moeller JR, Dhawan V, Spetsieris P, Takikawa S, Ishikawa T et al (1994). The metabolic topography of parkinsonism. J Cereb Blood Flow Metab 14: 783–801.
Feigin A, Fukuda M, Dhawan V, Przedborski S, Jackson-Lewis V, Mentis MJ et al (2001). Metabolic correlates of levodopa response in Parkinson's disease. Neurology 57: 2083–2088.
Folstein MF, Robins LN, Helzer JE (1983). The Mini-Mental State Examination. Arch Gen Psychiatry 40: 812.
Forman SD, Cohen JD, Fitzgerald M, Eddy WF, Mintun MA, Noll DC (1995). Improved assessment of significant activation in functional magnetic resonance imaging (fMRI): use of a cluster-size threshold. Magn Reson Med 33: 636–647.
Gao HM, Jiang J, Wilson B, Zhang W, Hong JS, Liu B (2002). Microglial activation-mediated delayed and progressive degeneration of rat nigral dopaminergic neurons: relevance to Parkinson's disease. J Neurochem 81: 1285–1297.
Gray F, Adle-Biassette H, Chretien F, Lorin de la Grandmaison G, Force G, Keohane C (2001). Neuropathology and neurodegeneration in human immunodeficiency virus infection. Pathogenesis of HIV-induced lesions of the brain, correlations with HIV-associated disorders and modifications according to treatments. Clin Neuropathol 20: 146–155.
Haas HS, Schauenstein K (1997). Neuroimmunomodulation via limbic structures—the neuroanatomy of psychoimmunology. Prog Neurobiol 51: 195–222.
Horikawa N, Yamazaki T, Sagawa M, Nagata T (1999). A case of akathisia during interferon-alpha therapy for chronic hepatitis type C. Gen Hosp Psychiatry 21: 134–135.
Juengling FD, Ebert D, Gut O, Engelbrecht MA, Rasenack J, Nitzsche EU et al (2000). Prefrontal cortical hypometabolism during low-dose interferon alpha treatment. Psychopharmacology (Berl) 152: 383–389.
Kamata M, Higuchi H, Yoshimoto M, Yoshida K, Shimizu T (2000). Effect of single intracerebroventricular injection of alpha-interferon on monoamine concentrations in the rat brain. Eur Neuropsychopharmacol 10: 129–132.
Konsman JP, Parnet P, Dantzer R (2002). Cytokine-induced sickness behaviour: mechanisms and implications. Trends Neurosci 25: 154–159.
Kumai T, Tateishi T, Tanaka M, Watanabe M, Shimizu H, Kobayashi S (2000). Effect of interferon-alpha on tyrosine hydroxylase and catecholamine levels in the brain of rats. Life Sci 67: 663–669.
Lee BN, Dantzer R, Langley KE, Bennett GJ, Dougherty PM, Dunn AJ et al (2004). A cytokine-based neuroimmunologic mechanism of cancer-related symptoms. Neuroimmunomodulation 11: 279–292.
Lee KA, Hicks G, Nino-Murcia G (1991). Validity and reliability of a scale to assess fatigue. Psychiatry Res 36: 291–298.
Leng A, Mura A, Feldon J, Ferger B (2005). Tumor necrosis factor-alpha receptor ablation in a chronic MPTP mouse model of Parkinson's disease. Neurosci Lett 375: 107–111.
Lou JS, Kearns G, Benice T, Oken B, Sexton G, Nutt J (2003). Levodopa improves physical fatigue in Parkinson's disease: a double-blind, placebo-controlled, crossover study. Mov Disord 18: 1108–1114.
Lou JS, Kearns G, Oken B, Sexton G, Nutt J (2001). Exacerbated physical fatigue and mental fatigue in Parkinson's disease. Mov Disord 16: 190–196.
Maddock C, Landau S, Barry K, Maulayah P, Hotopf M, Cleare AJ et al (2005). Psychopathological symptoms during interferon-alpha and ribavirin treatment: effects on virologic response. Mol Psychiatry 10: 332–333.
Maquet P, Dive D, Salmon E, von Frenckel R, Franck G (1990). Reproducibility of cerebral glucose utilization measured by PET and the [18F]-2-fluoro-2-deoxy-d-glucose method in resting, healthy human subjects. Eur J Nucl Med 16: 267–273.
Mayberg HS, Starkstein SE, Sadzot B, Preziosi T, Andrezejewski PL, Dannals RF et al (1990). Selective hypometabolism in the inferior frontal lobe in depressed patients with Parkinson's disease. Ann Neurol 28: 57–64.
McGinty JF (1999). Regulation of neurotransmitter interactions in the ventral striatum. Ann NY Acad Sci 877: 129–139.
Meek PM, Nail LM, Barsevick A, Schwartz AL, Stephen S, Whitmer K et al (2000). Psychometric testing of fatigue instruments for use with cancer patients. Nurs Res 49: 181–190.
Mentis MJ, McIntosh AR, Perrine K, Dhawan V, Berlin B, Feigin A et al (2002). Relationships among the metabolic patterns that correlate with mnemonic, visuospatial, and mood symptoms in Parkinson's disease. Am J Psychiatry 159: 746–754.
Meyers CA, Albitar M, Estey E (2005). Cognitive impairment, fatigue, and cytokine levels in patients with acute myelogenous leukemia or myelodysplastic syndrome. Cancer 104: 788–793.
Miaskowski C, Lee KA (1999). Pain, fatigue, and sleep disturbances in oncology outpatients receiving radiation therapy for bone metastasis: a pilot study. J Pain Symptom Manage 17: 320–332.
Montgomery SA, Asberg M (1979). A new depression scale designed to be sensitive to change. Br J Psychiatry 134: 382–389.
Musselman DL, Lawson DH, Gumnick JF, Manatunga AK, Penna S, Goodkin RS et al (2001). Paroxetine for the prevention of depression induced by high-dose interferon alpha. N Engl J Med 344: 961–966.
Nagatsu T, Sawada M (2005). Inflammatory process in Parkinson's disease: role for cytokines. Curr Pharm Des 11: 999–1016.
Pavol MA, Meyers CA, Rexer JL, Valentine AD, Mattis PJ, Talpaz M (1995). Pattern of neurobehavioral deficits associated with interferon alpha therapy for leukemia. Neurology 45: 947–950.
Phares TW, Kean RB, Mikheeva T, Hooper DC (2006). Regional differences in blood-brain barrier permeability changes and inflammation in the apathogenic clearance of virus from the central nervous system. J Immunol 176: 7666–7675.
Raison CL, Borisov AS, Broadwell SD, Capuron L, Woolwine BJ, Jacobson IM et al (2005). Depression during pegylated interferon-alpha plus ribavirin therapy: prevalence and prediction. J Clin Psychiatry 66: 41–48.
Raison CL, Capuron L, Miller AH (2006). Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol 27: 24–31.
Ramnani N (2006). The primate cortico-cerebellar system: anatomy and function. Nat Rev Neurosci 7: 511–522.
Salamone JD, Correa M, Mingote S, Weber SM (2003). Nucleus accumbens dopamine and the regulation of effort in food-seeking behavior: implications for studies of natural motivation, psychiatry, and drug abuse. J Pharmacol Exp Ther 305: 1–8.
Salamone JD, Correa M, Mingote SM, Weber SM (2005). Beyond the reward hypothesis: alternative functions of nucleus accumbens dopamine. Curr Opin Pharmacol 5: 34–41.
Schwartz AL, Thompson JA, Masood N (2002). Interferon-induced fatigue in patients with melanoma: a pilot study of exercise and methylphenidate. Oncol Nurs Forum 29: E85–E90.
Shuto H, Kataoka Y, Horikawa T, Fujihara N, Oishi R (1997). Repeated interferon-alpha administration inhibits dopaminergic neural activity in the mouse brain. Brain Res 747: 348–351.
Spetsieris PG, Moeller JR, Dhawan V, Ishikawa T, Eidelberg D (1995). Visualizing the evolution of abnormal metabolic networks in the brain using PET. Comput Med Imaging Graph 19: 295–306.
Sunami M, Nishikawa T, Yorogi A, Shimoda M (2000). Intravenous administration of levodopa ameliorated a refractory akathisia case induced by interferon-alpha. Clin Neuropharmacol 23: 59–61.
von Giesen HJ, Antke C, Hefter H, Wenserski F, Seitz RJ, Arendt G (2000). Potential time course of human immunodeficiency virus type 1-associated minor motor deficits: electrophysiologic and positron emission tomography findings. Arch Neurol 57: 1601–1607.
von Giesen HJ, Haslinger BA, Rohe S, Koller H, Arendt G (2005). HIV Dementia Scale and psychomotor slowing--the best methods in screening for neuro-AIDS. J Neuropsychiatry Clin Neurosci 17: 185–191.
Wang JY, Zeng XY, Fan GX, Yuan YK, Tang JS (2006). mu- but not delta- and kappa-opioid receptor mediates the nucleus submedius interferon-alpha-evoked antinociception in the rat. Neurosci Lett 397: 254–258.
Wichmann T, DeLong MR (1999). Oscillations in the basal ganglia. Nature 400: 621–622.
Wichmann T, DeLong MR (2003). Functional neuroanatomy of the basal ganglia in Parkinson's disease. Adv Neurol 91: 9–18.
Yamada T, Yamanaka I (1995). Microglial localization of alpha-interferon receptor in human brain tissues. Neurosci Lett 189: 73–76.
Acknowledgements
This research project was supported in part by the National Institute of Mental Health (MH067990 and MH069124), the Centers for Disease Control and Prevention, the National Institute of Biomedical Imaging and Bioengineering (EB002635), and the National Institute of Drug Abuse (DA00367). We thank John Votaw, PhD, for expert advice in image processing and analysis, and Delicia Votaw, CNMT, Margie Jones, CNMT, Clinton D Kilts, PhD, and the Emory Center for Positron Emission Tomography staff for assistance with image acquisition. The authors disclose the following contractual relationships: DHL: Speakers Bureau: Schering Plough Corporation and Chiron; CBN: Grants/Research Support: Abbott Laboratories; AFSP; AstraZeneca; Bristol-Myers-Squibb; Forest Laboratories; GlaxoSmithKline; Janssen Pharmaceutica; NARSAD; NIMH; Pfizer Pharmaceuticals; Stanley Foundation/NAMI; Wyeth-Ayerst; Consultant: Abbott Laboratories; Acadia Pharmaceuticals; AstraZeneca; Bristol-Myers-Squibb; Corcept; Cypress Biosciences; Cyberonics; Forest Laboratories; GlaxoSmithKline; Janssen Pharmaceutica; Ono Pharma; Otsuka; Pfizer Pharmaceuticals; Quintiles; Sanofi; Somerset; Wyeth-Ayerst; Speakers Bureau: Abbott Laboratories; AstraZeneca; GlaxoSmithKline; Janssen Pharmaceutica; Pfizer Pharmaceuticals; Stockholder: Corcept; Cypress Biosciences; Neurocrine Biosciences; Acadia Pharmaceuticals; Revaax; Board of Directors: American Foundation for Suicide Prevention (AFSP); American Psychiatric Institute for Research and Education (APIRE); George West Mental Health Foundation; Novadel Pharma; Patents: Method and devices for transdermal delivery of lithium (US 6,375,990 B1), Method to estimate serotonin and norepinephrine transporter occupancy after drug treatment using patient or animal serum (provisional filing April, 2001); AHM: Grants/Research Support: GlaxoSmithKline, Schering Plough Corporation, Janssen Pharmaceutica; Consultant: Schering Plough, Centocor.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Capuron, L., Pagnoni, G., Demetrashvili, M. et al. Basal Ganglia Hypermetabolism and Symptoms of Fatigue during Interferon-α Therapy. Neuropsychopharmacol 32, 2384–2392 (2007). https://doi.org/10.1038/sj.npp.1301362
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301362
Keywords
This article is cited by
-
Influences of dopaminergic system dysfunction on late-life depression
Molecular Psychiatry (2022)
-
Interferon and anti-TNF therapies differentially modulate amygdala reactivity which predicts associated bidirectional changes in depressive symptoms
Molecular Psychiatry (2021)
-
Inflammatory markers are associated with psychomotor slowing in patients with schizophrenia compared to healthy controls
npj Schizophrenia (2020)
-
Whole-blood expression of inflammasome- and glucocorticoid-related mRNAs correctly separates treatment-resistant depressed patients from drug-free and responsive patients in the BIODEP study
Translational Psychiatry (2020)
-
Neuroimaging in the Kleine-Levin Syndrome
Current Neurology and Neuroscience Reports (2018)