Abstract
The aim of the study was to compare the diagnostic performance of endoscopic ultrasonography (EUS), computed tomography (CT), and 18F-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) in staging of oesophageal cancer. PubMed was searched to identify English-language articles published before January 2006 and reporting on diagnostic performance of EUS, CT, and/or FDG-PET in oesophageal cancer patients. Articles were included if absolute numbers of true-positive, false-negative, false-positive, and true-negative test results were available or derivable for regional, celiac, and abdominal lymph node metastases and/or distant metastases. Sensitivities and specificities were pooled using a random effects model. Summary receiver operating characteristic analysis was performed to study potential effects of study and patient characteristics. Random effects pooled sensitivities of EUS, CT, and FDG-PET for regional lymph node metastases were 0.80 (95% confidence interval 0.75–0.84), 0.50 (0.41–0.60), and 0.57 (0.43–0.70), respectively, and specificities were 0.70 (0.65–0.75), 0.83 (0.77–0.89), and 0.85 (0.76–0.95), respectively. Diagnostic performance did not differ significantly across these tests. For detection of celiac lymph node metastases by EUS, sensitivity and specificity were 0.85 (0.72–0.99) and 0.96 (0.92–1.00), respectively. For abdominal lymph node metastases by CT, these values were 0.42 (0.29–0.54) and 0.93 (0.86–1.00), respectively. For distant metastases, sensitivity and specificity were 0.71 (0.62–0.79) and 0.93 (0.89–0.97) for FDG-PET and 0.52 (0.33–0.71) and 0.91 (0.86–0.96) for CT, respectively. Diagnostic performance of FDG-PET for distant metastases was significantly higher than that of CT, which was not significantly affected by study and patient characteristics. The results suggest that EUS, CT, and FDG-PET each play a distinctive role in the detection of metastases in oesophageal cancer patients. For the detection of regional lymph node metastases, EUS is most sensitive, whereas CT and FDG-PET are more specific tests. For the evaluation of distant metastases, FDG-PET has probably a higher sensitivity than CT. Its combined use could however be of clinical value, with FDG-PET detecting possible metastases and CT confirming or excluding their presence and precisely determining the location(s).
Similar content being viewed by others
Main
To optimise the selection of patients with oesophageal cancer for a curative or palliative treatment option, it is important to determine the depth of infiltration of the tumour into the oesophageal wall (T stage), and the presence of malignant regional lymph nodes (N stage) and distant metastases (M stage). For N stage, N0 and N1 indicate the absence or presence of regional lymph node metastases, respectively. Similarly, M0 indicates the absence and M1 the presence of distant metastases (Fleming et al, 1997). Whether a malignant lymph node is defined as N1 or M1 depends on the location of the primary tumour. For example, malignant celiac lymph nodes are staged as M1a if the primary tumour is located in the distal part of the oesophagus, but as stage M1b if the tumour is located in the more proximal part of the oesophagus and as N1 if the tumour is located in the gastric cardia (Thompson, 1997). Distant metastases from oesophageal cancer are most frequently detected in celiac and supraclavicular lymph nodes, liver, lung, and adrenal glands (Quint et al, 1995).
Endoscopic ultrasonography (EUS) is often used to determine the depth of tumour invasion and the presence of malignant regional and celiac lymph nodes in patients with oesophageal cancer. Both computed tomography (CT) and 18F-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) are commonly applied to determine whether malignant lymph nodes or distant metastases are present.
It is known that EUS, CT, and FDG-PET each have certain limitations. For example, only lymph nodes in the proximity of the oesophageal and gastric wall can be visualised with EUS, as it has a limited penetration depth of approximately 5 cm. As a consequence, metastases in distant lymph nodes or organs can often not be detected by EUS (Kienle et al, 2002). Computed tomography is not able to detect metastases in normal-sized lymph nodes. Furthermore, an enlarged lymph node may contain metastases, but can also be enlarged as a consequence of inflammation (Halvorsen and Thompson, 1984; Finch et al, 1997; Choi et al, 2000). The same is true for abnormal findings in the liver or adrenal glands, for which it is not always clear whether these are metastases or not. Detection of metastases by FDG-PET is based on an altered tissue glucose metabolism. Biochemical changes are known to appear earlier in time than structural changes and also they are more specific (Block et al, 1997; Flanagan et al, 1997). Nevertheless, lesions less than 1 cm in diameter can be missed by FDG-PET (Lerut et al, 2000).
In this study, we evaluated the diagnostic performance of EUS, CT, and FDG-PET as has been reported in the literature. In addition, we determined whether only one or a combination of these investigations should be used in the staging of oesophageal cancer. The focus in this meta-analysis was on the application of EUS for the detection of malignant regional and celiac lymph nodes, the use of CT for the detection of malignant regional and abdominal lymph nodes and distant metastases, and the use of FDG-PET for the detection of malignant regional lymph nodes and distant metastases.
Materials and methods
Literature search and data extraction
A PubMed literature search was performed identifying all articles related to the diagnostic use of EUS, CT, and FDG-PET in patients with oesophageal cancer. Search terms that were used to identify such articles were combinations of ‘esophagus’, ‘oesophagus’, ‘cancer’, ‘neoplasm’, ‘carcinoma’, ‘endoscopic ultrasonography’, ‘endosonography’ ‘EUS’, ‘computed tomography’, ‘CT’, ‘positron emission tomography’, and ‘PET’. Abstracts obtained from these searches were evaluated. Articles containing information on the results of EUS, CT, and/or FDG-PET for N and/or M stage of oesophageal cancer and published in the English literature before January 2006 were reviewed. Articles were included if the absolute numbers of true-positive (TP), false-negative (FN), false-positive (FP), and true-negative (TN) test results were available or derivable from the article, which allowed us to construct 2 × 2 contingency tables. The references of articles and reviews, found in the literature search, were also examined to find additional articles that met the inclusion criteria. Studies with potentially overlapping study populations were excluded. For this, we included only the study with the largest patient population and published latest in time, whereas the previous study, with often a smaller subgroup of patients, was excluded. Also excluded were articles published in abstract form only, case reports, editorials, and reviews. In addition, articles containing the results of patients who had undergone prior radiation and/or chemotherapy were excluded if the result of the reference standard could have been influenced by the administration of this treatment. The reference standard was resection, result of fine-needle aspiration (FNA), follow-up with radiographic techniques, and/or clinical follow-up in the article.
Two independent readers (EV, PS) extracted the data from the included articles. The absolute numbers of TP, FN, FP, and TN test results were retrieved or calculated from the published data. Other characteristics that were extracted from each study were origin and publication year of an article, mean age of patients, proportion of males (as percentage of total number of patients), tumour histology, retrospective or prospective set-up of the study, whether or not the patients were consecutively included, whether or not the test results were blindly interpreted, and the reference standard that was used in the study. For articles containing EUS results, the type of EUS probe, whether or not FNA was performed for suspicious lymph nodes, and whether or not dilation was performed in patients with a stenotic tumour were also recorded. From articles containing CT results, information on the type of CT scanner and use of a contrast agent was obtained. From articles containing FDG-PET results, the type of PET scanner was recorded. Inconsistent findings between the two readers were discussed and agreed upon by consensus.
Statistical analysis
To determine whether publication bias, that is, the selective reporting of manuscripts with more positive results, was present, funnel plots were constructed. A funnel plot is an epidemiologic method for assessing the presence of publication bias. For this, the measure of study size is plotted against the measure of interest. In this study, the measure of study size was the number of patients included in the study, whereas the measure of interest was the natural logarithm of the diagnostic odds ratio (D). The idea is that studies with the largest study size will estimate D most accurately, whereas studies with a smaller study size will have a more variable result, with both lower and higher values of D compared to the larger studies. If this is the case, the plot will have a symmetric, inverted funnel shape. If publication bias is present, the left base of the plot will disappear and the plot is asymmetric and skewed (Terrin et al, 2005). Symmetry and shape of the funnel plots were determined by means of visual inspection. To allow assessment of the presence of publication bias by visual inspection, the number of included articles had to be more than 10.
Sensitivities and specificities of EUS, CT, and FDG-PET were pooled using a random effects model. With this method, the variability between studies is taken into account. To estimate the relationship between sensitivities and specificities of each investigation, a random effects summary receiver operating characteristic (SROC) analysis was performed. In an SROC analysis, the logits (log odds) of sensitivity and 1−specificity are subtracted to calculate D (D=ln(sensitivity/(1−sensitivity))−ln((1−specificity)/specificity)). D is the log of the diagnostic odds ratio, which represents a summary measure of the diagnostic performance or discriminatory power of an investigation. D ranges from zero to infinity. A value close to zero or far from 1 represents an investigation with good diagnostic performance. The logits are summed to calculate S (S=ln(sensitivity/(1−sensitivity))+ln((1−specificity)/specificity)), which is a proxy for the positivity criterion of the diagnostic test. When institutions use different thresholds for scoring a test result as positive, different positivity criteria will exist among studies. Subsequently, a linear regression model D=a+bS was estimated, weighted by the inverse of the variance of D. We have chosen to perform a weighted regression, as the unweighted regression may not highlight larger studies.
Additional covariates (such as publication year, number of patients, mean age, proportion of males, whether or not the study was performed prospectively, whether or not the patients were included consecutively, and whether or not the test results were interpreted in a blinded fashion) were added to the model to adjust for differences in study and patient characteristics. The effect of a covariate was expressed in the relative diagnostic odds ratio (a value >1, 1, or <1 means superior, equal, or inferior diagnostic performance, respectively) and was considered statistically significant if P<0.05. The meta and metareg commands of STATA 8.0 were used to perform the meta-analysis.
Results
Literature search and data extraction
The PubMed literature search for the identification of articles relating to the diagnostic use of EUS in oesophageal cancer patients resulted in 573 hits on the search terms. In total, 31 articles on EUS for regional lymph node metastases (Tio et al, 1990; Botet et al, 1991; Rice et al, 1991; Ziegler et al, 1991; Dittler and Siewert, 1993; Grimm et al, 1993; Greenberg et al, 1994; Yoshikane et al, 1994; Binmoeller et al, 1995; Hasegawa et al, 1996; Hunerbein et al, 1996; Natsugoe et al, 1996; Pham et al, 1998; Vickers, 1998; Bowrey et al, 1999; Catalano et al, 1999; Nishimaki et al, 1999; Salminen et al, 1999; Choi et al, 2000; Nesje et al, 2000; Richards et al, 2000; Shinkai et al, 2000; Vazquez-Sequeiros et al, 2001, 2003; Rasanen et al, 2003; Wu et al, 2003; Heeren et al, 2004; Sihvo et al, 2004; DeWitt et al, 2005; Lowe et al, 2005; Pedrazzani et al, 2005) and five articles on EUS for celiac lymph node metastases were included (Binmoeller et al, 1995; Catalano et al, 1999; Eloubeidi et al, 2001; Vazquez-Sequeiros et al, 2001; Parmar et al, 2002) (Table 1). For CT, the literature search gave 1091 hits. Seventeen articles on CT for regional lymph node metastases met the inclusion criteria (Quint et al, 1985; Botet et al, 1991; Ziegler et al, 1991; Sondenaa et al, 1992; Greenberg et al, 1994; Yoshikane et al, 1994; Flanagan et al, 1997; Nishimaki et al, 1999; Choi et al, 2000; Wren et al, 2002; Rasanen et al, 2003; Vazquez-Sequeiros et al, 2003; Wu et al, 2003; Yoon et al, 2003; Heeren et al, 2004; Sihvo et al, 2004; Lowe et al, 2005). As some articles containing the results of CT not only reported on celiac lymph node metastases, but also on other abdominal lymph node metastases, we decided to include all articles (five in total) with these results (Quint et al, 1985; Becker et al, 1986; Watt et al, 1989; Van Overhagen et al, 1993; Parmar et al, 2002). In addition, seven articles on CT for distant metastases were included (Van Overhagen et al, 1993; Flamen et al, 2000; Wren et al, 2002; Rasanen et al, 2003; Yoon et al, 2003; Sihvo et al, 2004; Lowe et al, 2005) (Table 2). Our literature search for FDG-PET gave 163 hits. We included 10 articles on FDG-PET for regional lymph node metastases (Flanagan et al, 1997; Luketich et al, 1997; Choi et al, 2000; Lerut et al, 2000; Wren et al, 2002; Rasanen et al, 2003; Yoon et al, 2003; Heeren et al, 2004; Sihvo et al, 2004; Lowe et al, 2005). Nine articles were included on FDG-PET for distant metastases (Luketich et al, 1997; Flamen et al, 2000; Lerut et al, 2000; Wren et al, 2002; Rasanen et al, 2003; Yoon et al, 2003; Heeren et al, 2004; Sihvo et al, 2004; Lowe et al, 2005) (Table 3). We found that the interobserver agreement for the data extraction was excellent (κ>0.80).
Regional lymph node metastases
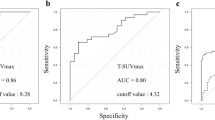
Random effects pooled sensitivity and specificity of EUS for N stage were 0.80 (95% confidence interval (CI) 0.75–0.84) and 0.70 (95% CI 0.65–0.75), respectively, and the pooled log odds ratio was 1.94 (95% CI 1.71–2.17) (Table 4). Visual inspection of the funnel plot revealed that the plot was symmetric (Figure 1), which implies that the presence of publication bias was unlikely. In the present study, no statistically significant differences were found between EUS and EUS-FNA for N stage.
Random effects pooled sensitivity and specificity of CT for regional lymph node metastases were 0.50 (95% CI 0.41–0.60) and 0.83 (95% CI 0.77–0.89), respectively. The pooled log odds ratio was 1.40 (95% CI 1.08–1.72) (Table 4). No evidence for publication bias was found (Figure 2).
Random effects pooled sensitivity and specificity of FDG-PET for regional lymph node metastases were 0.57 (95% CI 0.43–0.70) and 0.85 (95% CI 0.76–0.95), respectively. The pooled log odds ratio was 1.71 (95% CI 1.22–2.20) (Table 4). It was not possible to assess whether publication bias was present, as the number of articles was too small (n=10).
The estimated SROC curves are shown in Figure 3. The differences between the curves of EUS, CT, and FDG-PET for N staging were not statistically significant. The relative diagnostic odds ratio of CT vs EUS was 0.76 (95% CI 0.48–1.21; P=0.25) and of FDG-PET vs EUS 0.95 (95% CI 0.54–1.67; P=0.86). Thus, taking into account the inverse relationship between sensitivity and specificity and different test thresholds across different studies, there were no significant differences in diagnostic performance across these tests for the detection of regional lymph node metastases. Study and patient characteristics also did not show any significant effect on the diagnostic performance of the tests. Nevertheless, comparing the pooled sensitivities and pooled specificities across the tests, statistically significant differences were present, that is, the 95% CI did not always overlap. Sensitivities of CT and FDG-PET for N stage were significantly lower than that of EUS, whereas specificities were significantly higher. This implies that these investigations work at different points on the SROC curve, that is, with EUS being more sensitive and less specific than CT and FDG-PET for regional lymph node metastases, but overall having a similar diagnostic performance (Table 4).
Celiac and abdominal lymph node metastases
Random effects pooled sensitivity and specificity of EUS for celiac lymph node metastases were 0.85 (95% CI 0.72–0.99) and 0.96 (95% CI 0.92–1.00), respectively, and the pooled log odds ratio was 3.89 (95% CI 2.67–5.11) (Table 4). As the number of articles was only five, assessment of publication bias was not possible.
Random effects pooled sensitivity and specificity of CT for malignant abdominal lymph nodes were 0.42 (95% CI 0.29–0.54) and 0.93 (95% CI 0.86–1.00), respectively. The pooled log odds ratio measured 1.74 (95% CI 0.45–3.04) (Table 4). It was not possible to assess whether publication bias was present.
We have not included an SROC curve for EUS (celiac lymph node metastases) and CT (abdominal lymph node metastases) as we think that these curves could not be fairly compared with each other.
Distant metastases
Random effects pooled sensitivity and specificity of CT for distant metastases were 0.52 (95% CI 0.33–0.71) and 0.91 (95% CI 0.86–0.96), respectively. The pooled log odds ratio was 2.10 (95% CI 1.59–2.62) (Table 4). The number of articles was too low to assess publication bias.
Random effects pooled sensitivity and specificity of FDG-PET for the detection of distant metastases were 0.71 (95% CI 0.62–0.79) and 0.93 (95% CI 0.89–0.97), respectively. The pooled log odds ratio was 2.93 (95% CI 2.41–3.45) (Table 4). Assessment of publication bias was not possible.
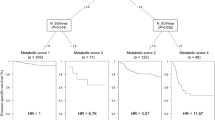
If the pooled sensitivities, specificities, and log odds ratios across tests were compared separately, we found higher values of FDG-PET for the detection of distant metastases compared to CT, although not statistically significant. Nevertheless, the SROC analysis showed that the diagnostic performance of FDG-PET was significantly higher than the diagnostic performance of CT (relative diagnostic odds ratio=2.26 (95% CI 1.09–4.71), P<0.03), taking into account the inverse relationship between sensitivity and specificity and different test thresholds across the studies (Figure 4).
To adjust for differences in study characteristics, various covariates were added in the SROC analysis. This showed that the covariates were not statistically significant (P>0.05), and there was significant difference between the diagnostic performance of CT and FDG-PET for the detection of distant metastases.
Discussion
We performed a meta-analysis to determine the value of EUS, CT, and FDG-PET in the staging of oesophageal cancer patients. We found that EUS was significantly more sensitive but less specific than CT and FDG-PET for the detection of regional lymph node metastases. The overall diagnostic performance of the three tests, however, was similar. Furthermore, we found that the diagnostic performance of FDG-PET was significantly higher than that of CT for distant metastases.
Based on these results, EUS was shown to be particularly useful for the exclusion of regional lymph node metastases. The low number of false-negative results for EUS meant that a negative EUS result will be in most patients a truly negative one. The sensitivities of CT and FDG-PET for the detection of regional lymph node metastases were lower. It is already known that lymph nodes adjacent to the primary oesophageal cancer are difficult to discriminate from the primary tumour with FDG-PET (McAteer et al, 1999), which is due to the intense activity in the primary cancer (Flanagan et al, 1997) and the limited spatial resolution of PET (Luketich et al, 1997; Rankin et al, 1998). Low sensitivity of CT for regional lymph node can at least partly be explained by the fact that CT is not able to detect metastases in normal-sized lymph nodes (Choi et al, 2000).
Computed tomography and/or FDG-PET can be used to confirm that an enlarged regional lymph node is indeed metastatic, as the number of false-positive results was found to be relatively low for both investigations. However, a better option nowadays is to perform EUS-guided FNA to confirm metastatic disease. This is in line with recommendations in the literature, in which EUS-FNA, CT, and/or FDG-PET are advocated for the exclusion of the presence of regional lymph node metastases in oesophageal cancer patients, particularly if this will affect a treatment decision in these patients. In several studies, it has been demonstrated that the results of EUS-FNA were better than those of EUS alone for determining N stage (Eloubeidi et al, 2001; Vazquez-Sequeiros et al, 2001; Parmar et al, 2002; van Vliet et al, 2006), because EUS combined with FNA allowed a cytological differentiation between reactive (non-malignant) and malignant lymph nodes (van Vliet et al, 2006).
The presence or absence of regional lymph node metastases has little direct consequences for the treatment decision. For example, patients with a T1–3 tumour without distant metastases and who are fit enough will receive a resection, which is mostly irrespective of the presence of regional lymph node metastases. Nonetheless, it is important to know whether regional lymph node metastases are present if an endoscopic treatment option is considered in patients with early-stage oesophageal cancer. In addition, the presence of regional lymph node metastases plays a role in the comparison of treatment modalities of oesophageal cancer, for example if comparing neoadjuvant therapy plus surgery vs surgery alone, and has consequences for the prognosis of patients. Therefore, we think that it is important to analyse whether detected lymph nodes are indeed metastatic (by using FNA), particularly if this will affect a treatment decision in patients.
It is also of clinical relevance to determine whether celiac and/or other abdominal lymph node metastases are present. If present, these are considered to be distant metastases (M1b), depending on the localisation of the primary tumour, which could change a treatment decision from a curative to a palliative option. As several articles on CT for staging oesophageal cancer reported not only on celiac lymph nodes, but also on other abdominal lymph nodes, the pooled results of EUS for the detection of celiac lymph node metastases and the pooled results of CT for the detection of abdominal lymph node metastases could not be fairly compared. Nevertheless, as the results of EUS and CT were clearly different, with EUS results being obviously better, it seems likely that EUS is the preferred investigation to determine whether or not celiac lymph node metastases are present in patients with oesophageal cancer. It is important to realise, however, that not all abdominal lymph nodes can be determined with EUS, as the EUS probe has a limited penetration depth of approximately 5 cm. Although no data are available in the literature, we recommend combining EUS with CT to investigate whether, apart from celiac lymph node metastases, other abdominal lymph node metastases are present.
The staging results of EUS for celiac lymph node metastases were even better than those for regional lymph node metastases. An explanation for this could be that only a few studies have reported on the use of EUS for the detection of malignant celiac lymph nodes, which were likely performed in high-volume EUS centres. In contrast, studies that reported EUS results for regional lymph node metastases were performed not only in high-volume centres, but also in low-volume centres. We recently reported that the results of EUS performed in a centre where <50 EUS procedures per endoscopist per year (low-volume centres) are performed were inferior to those from high-volume EUS centres (>50 EUS procedures per endoscopist per year) (van Vliet et al, 2006).
Both CT and FDG-PET can be used to detect distant metastases, which determines whether a patient is suitable for a curative treatment option. The reported results of the investigations varied widely (Table 2 and 3) and it is currently difficult to determine how these investigations should be used during staging of patients with oesophageal cancer. The pooled sensitivity of CT for the detection of distant metastases was lower than that of FDG-PET, whereas specificity was equivalent. The results for FDG-PET were comparable to the results found in a previous meta-analysis on FDG-PET for this indication (van Westreenen et al, 2004). In our SROC analysis, we found that the diagnostic performance of FDG-PET was significantly better than that of CT (Figure 4). This method takes both sensitivity and specificity into account and adjusts for potential differences in test thresholds across studies. Two studies in which FDG-PET was directly compared with CT for the detection of distant metastases (Luketich et al, 1999; Flamen et al, 2000) demonstrated that both sensitivity and specificity of FDG-PET for distant metastases were higher compared to those of CT. In contrast, other studies comparing FDG-PET with CT found similar accuracies for both investigations for the detection of distant metastases (Wren et al, 2002; Kneist et al, 2003, 2004; Rasanen et al, 2003; Sihvo et al, 2004).
Several publications have reported on the additional value of FDG-PET for the detection of distant metastases, and it has been demonstrated that distant metastases were detected with FDG-PET in 0–20% of patients with oesophageal cancer, which were not found with other investigations. In patients in whom distant metastases were detected with FDG-PET, the treatment plan was corrected from a curative to a palliative option and unnecessary surgery was precluded (Block et al, 1997; Flanagan et al, 1997; Kole et al, 1998; Rankin et al, 1998; Luketich et al, 1999; Flamen et al, 2000; Lerut et al, 2000; Wren et al, 2002; Imdahl et al, 2004; van Westreenen et al, 2005). Disadvantages of FDG-PET include the high costs and the fact that it mostly needs to be combined with CT to localise a lesion that is visualised by FDG-PET. It remains to be established whether the costs of FDG-PET are compensated for by the cost reduction of resections that are prevented due to the finding of additional metastases with FDG-PET. In the early days of FDG-PET, it was unclear whether FDG-PET should be the initial investigation to detect metastases in oesophageal cancer, or, alternatively, whether FDG-PET should be performed if EUS and CT have already been performed. The performance of FDG-PET alone does not seem to be the ideal method for the detection of distant metastases, but the combined use of FDG-PET and CT could well be of significance. This is already on the horizon, as integrated FDG-PET/CT machines are increasingly becoming available. Unfortunately, the value of PET-CT could not be clearly determined by our meta-analysis, as there were not enough well-performed studies available.
Our meta-analysis has some limitations. First, abstracts were assessed to identify articles reporting on the results of EUS, CT, and FDG-PET. There is a small risk that some articles of which the abstract revealed that it was highly unlikely that the article contained information on the results of EUS, CT, and/or FDG-PET were excluded from evaluation. It is also possible that articles with results on EUS, CT, and FDG-PET did not match the search terms. To correct for this, references of included articles and reviews were examined for additional articles that met the inclusion criteria.
Second, only studies with the results of EUS, CT, and/or FDG-PET for the detection of lymph node or distant metastases from which absolute numbers of TP, FN, FP, and TN test results were available or derivable were included, which is advocated in the STARD guidelines (Bossuyt et al, 2003). Several studies did not report these absolute numbers precluding thorough statistical evaluation. In addition, some of our analyses were based on limited numbers of publications and it could therefore be that some differences in this meta-analysis were not statistically significant due to these limited sample sizes.
Third, it seems likely that verification bias played a role in all articles included in our meta-analysis, because the results of staging investigations performed in patients with oesophageal cancer were used to decide whether or not FNA should be performed and whether or not patients could undergo a resection. Funnel plots, as shown in Figure 1 and 2, revealed that publication bias was probably not present in the meta-analysis regarding EUS and CT for the detection of regional lymph node metastases. Nevertheless, for the other analyses, the number of included studies was too small to evaluate publication bias.
Fourth, the time period in which the evaluated articles were published might also be a factor to consider. The initial reported results of a new investigation are often more favorable than those published later in time if the procedure is used in a less selected study population. We accounted for this potential effect by including the year of publication as a covariate in our analysis. The results showed that the publication year was not a significant predictor of diagnostic performance in our study.
Fifth, the methodological quality of some studies included in this meta-analysis was limited. For example, several studies that are shown in Table 1, 2, 3 were retrospectively performed and in some studies the test results were not blindly interpreted. In addition, missing values were present for some covariates, particularly for the covariates inclusion (consecutive or not) and interpretation (blinded or not).
Sixth, only a few articles on CT and EUS reported nodal cutoff sizes for positivity. For this reason, we could not perform a sub-analysis to determine which nodal cutoff size was most accurate. In addition, only a few articles reported on the location of the tumour and, therefore, it was not possible to determine whether the results of EUS differed for the various locations of the tumours, that is, cervical, upper 1/3 thoracic, central 1/3 thoracic, lower 1/3 thoracic, and gastrooesophageal junction. In addition, it would have been clinically interesting if the localisation of the primary tumour could have been combined with nodal status. The same was true for the location of distant metastases, which was also not reported in the majority of studies and, if reported, results were not given per location. Therefore, it was not possible to calculate results for the different metastatic locations in our meta-analysis.
Finally, it is known that experience is an important factor in performing EUS. Nevertheless, in the majority of articles, it was not reported how experienced endoscopists were and, therefore, we could not determine whether EUS results varied for different levels of experience. Moreover, no information was given on the number of patients with squamous cell carcinoma or adenocarcinoma in several studies and, if reported, results were mostly not reported per tumour histology.
In conclusion, the presence of malignant regional lymph nodes can be determined with EUS, CT, and FDG-PET. Of these, EUS has the highest sensitivity but also the lowest specificity for regional lymph node metastases. To exclude the presence of regional lymph node metastases, EUS should be used, whereas detected lesions should be confirmed with FNA, or, alternatively, with CT and/or FDG-PET, particularly if this will affect a treatment decision in patients. Both EUS and CT should probably be performed to determine whether abdominal lymph node metastases are present, with EUS being highly sensitive for celiac lymph node metastases and CT being performed to detect other abdominal lymph node metastases. Both CT and FDG-PET can be used to detect the presence of distant metastases; however, the results suggest that FDG-PET has a higher diagnostic performance than CT. Nonetheless, it seems likely that its combined use could be of clinical value, with FDG-PET detecting possible metastases and CT confirming or excluding their presence and precisely determining the location(s). Nowadays, integrated FDG-PET/CT machines are increasingly being available and their use has become more common.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Becker CD, Barbier P, Porcellini B (1986) CT evaluation of patients undergoing transhiatal esophagectomy for cancer. J Comput Assist Tomogr 10: 607–611
Binmoeller KF, Seifert H, Seitz U, Izbicki JR, Kida M, Soehendra N (1995) Ultrasonic esophagoprobe for TNM staging of highly stenosing esophageal carcinoma. Gastrointest Endosc 41: 547–552
Block MI, Patterson GA, Sundaresan RS, Bailey MS, Flanagan FL, Dehdashti F, Siegel BA, Cooper JD (1997) Improvement in staging of esophageal cancer with the addition of positron emission tomography. Ann Thorac Surg 64: 770–776; discussion 776, 777
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, Lijmer JG, Moher D, Rennie D, de Vet HC (2003) Towards complete and accurate reporting of studies of diagnostic accuracy: The STARD Initiative. Radiology 226: 24–28
Botet JF, Lightdale CJ, Zauber AG, Gerdes H, Winawer SJ, Urmacher C, Brennan MF (1991) Preoperative staging of esophageal cancer: comparison of endoscopic US and dynamic CT. Radiology 181: 419–425
Bowrey DJ, Clark GW, Roberts SA, Maughan TS, Hawthorne AB, Williams GT, Carey PD (1999) Endosonographic staging of 100 consecutive patients with esophageal carcinoma: introduction of the 8-mm esophagoprobe. Dis Esophagus 12: 258–263
Catalano MF, Alcocer E, Chak A, Nguyen CC, Raijman I, Geenen JE, Lahoti S, Sivak Jr MV (1999) Evaluation of metastatic celiac axis lymph nodes in patients with esophageal carcinoma: accuracy of EUS. Gastrointest Endosc 50: 352–356
Choi JY, Lee KH, Shim YM, Lee KS, Kim JJ, Kim SE, Kim BT (2000) Improved detection of individual nodal involvement in squamous cell carcinoma of the esophagus by FDG PET. J Nucl Med 41: 808–815
DeWitt J, Kesler K, Brooks JA, LeBlanc J, McHenry L, McGreevy K, Sherman S (2005) Endoscopic ultrasound for esophageal and gastroesophageal junction cancer: impact of increased use of primary neoadjuvant therapy on preoperative locoregional staging accuracy. Dis Esophagus 18: 21–27
Dittler HJ, Siewert JR (1993) Role of endoscopic ultrasonography in esophageal carcinoma. Endoscopy 25: 156–161
Eloubeidi MA, Wallace MB, Reed CE, Hadzijahic N, Lewin DN, Van Velse A, Leveen MB, Etemad B, Matsuda K, Patel RS, Hawes RH, Hoffman BJ (2001) The utility of EUS and EUS-guided fine needle aspiration in detecting celiac lymph node metastasis in patients with esophageal cancer: a single-center experience. Gastrointest Endosc 54: 714–719
Finch MD, John TG, Garden OJ, Allan PL, Paterson-Brown S (1997) Laparoscopic ultrasonography for staging gastroesophageal cancer. Surgery 121: 10–17
Flamen P, Lerut A, Van Cutsem E, De Wever W, Peeters M, Stroobants S, Dupont P, Bormans G, Hiele M, De Leyn P, Van Raemdonck D, Coosemans W, Ectors N, Haustermans K, Mortelmans L (2000) Utility of positron emission tomography for the staging of patients with potentially operable esophageal carcinoma. J Clin Oncol 18: 3202–3210
Flanagan FL, Dehdashti F, Siegel BA, Trask DD, Sundaresan SR, Patterson GA, Cooper JD (1997) Staging of esophageal cancer with 18F-fluorodeoxyglucose positron emission tomography. AJR Am J Roentgenol 168: 417–424
Fleming ID, Cooper JS, Henson DE (1997) AJCC Cancer Staging Manual. Philadelphia: Lippincott-Raven Publishers
Greenberg J, Durkin M, Van Drunen M, Aranha GV (1994) Computed tomography or endoscopic ultrasonography in preoperative staging of gastric and esophageal tumors. Surgery 116: 696–701; discussion 701, 702
Grimm H, Binmoeller KF, Hamper K, Koch J, Henne-Bruns D, Soehendra N (1993) Endosonography for preoperative locoregional staging of esophageal and gastric cancer. Endoscopy 25: 224–230
Halvorsen RA, Thompson WM (1984) Computed tomographic evaluation of esophageal carcinoma. Semin Oncol 11: 113–126
Hasegawa N, Niwa Y, Arisawa T, Hase S, Goto H, Hayakawa T (1996) Preoperative staging of superficial esophageal carcinoma: comparison of an ultrasound probe and standard endoscopic ultrasonography. Gastrointest Endosc 44: 388–393
Heeren PA, Jager PL, Bongaerts F, van Dullemen H, Sluiter W, Plukker JT (2004) Detection of distant metastases in esophageal cancer with (18)F-FDG PET. J Nucl Med 45: 980–987
Hunerbein M, Dohmoto M, Rau B, Schlag PM (1996) Endosonography and endosonography-guided biopsy of upper-GI-tract tumors using a curved-array echoendoscope. Surg Endosc 10: 1205–1209
Imdahl A, Hentschel M, Kleimaier M, Hopt UT, Brink I (2004) Impact of FDG-PET for staging of oesophageal cancer. Langenbecks Arch Surg 389: 283–288
Kienle P, Buhl K, Kuntz C, Dux M, Hartmann C, Axel B, Herfarth C, Lehnert T (2002) Prospective comparison of endoscopy, endosonography and computed tomography for staging of tumours of the oesophagus and gastric cardia. Digestion 66: 230–236
Kneist W, Schreckenberger M, Bartenstein P, Grunwald F, Oberholzer K, Junginger T (2003) Positron emission tomography for staging esophageal cancer: does it lead to a different therapeutic approach? World J Surg 27: 1105–1112
Kneist W, Schreckenberger M, Bartenstein P, Menzel C, Oberholzer K, Junginger T (2004) Prospective evaluation of positron emission tomography in the preoperative staging of esophageal carcinoma. Arch Surg 139: 1043–1049
Kole AC, Plukker JT, Nieweg OE, Vaalburg W (1998) Positron emission tomography for staging of oesophageal and gastroesophageal malignancy. Br J Cancer 78: 521–527
Lerut T, Flamen P, Ectors N, Van Cutsem E, Peeters M, Hiele M, De Wever W, Coosemans W, Decker G, De Leyn P, Deneffe G, Van Raemdonck D, Mortelmans L (2000) Histopathologic validation of lymph node staging with FDG-PET scan in cancer of the esophagus and gastroesophageal junction: a prospective study based on primary surgery with extensive lymphadenectomy. Ann Surg 232: 743–752
Lowe VJ, Booya F, Fletcher JG, Nathan M, Jensen E, Mullan B, Rohren E, Wiersema MJ, Vazquez-Sequeiros E, Murray JA, Allen MS, Levy MJ, Clain JE (2005) Comparison of positron emission tomography, computed tomography, and endoscopic ultrasound in the initial staging of patients with esophageal cancer. Mol Imaging Biol 7: 422–430
Luketich JD, Friedman DM, Weigel TL, Meehan MA, Keenan RJ, Townsend DW, Meltzer CC (1999) Evaluation of distant metastases in esophageal cancer: 100 consecutive positron emission tomography scans. Ann Thorac Surg 68: 1133–1136; discussion 1136, 1137
Luketich JD, Schauer PR, Meltzer CC, Landreneau RJ, Urso GK, Townsend DW, Ferson PF, Keenan RJ, Belani CP (1997) Role of positron emission tomography in staging esophageal cancer. Ann Thorac Surg 64: 765–769
McAteer D, Wallis F, Couper G, Norton M, Welch A, Bruce D, Park K, Nicolson M, Gilbert FJ, Sharp P (1999) Evaluation of 18F-FDG positron emission tomography in gastric and oesophageal carcinoma. Br J Radiol 72: 525–529
Natsugoe S, Yoshinaka H, Morinaga T, Shimada M, Baba M, Fukumoto T, Stein HJ, Aikou T (1996) Ultrasonographic detection of lymph-node metastases in superficial carcinoma of the esophagus. Endoscopy 28: 674–679
Nesje LB, Svanes K, Viste A, Laerum OD, Odegaard S (2000) Comparison of a linear miniature ultrasound probe and a radial-scanning echoendoscope in TN staging of esophageal cancer. Scand J Gastroenterol 35: 997–1002
Nishimaki T, Tanaka O, Ando N, Ide H, Watanabe H, Shinoda M, Takiyama W, Yamana H, Ishida K, Isono K, Endo M, Ikeuchi T, Mitomi T, Koizumi H, Imamura M, Iizuka T (1999) Evaluation of the accuracy of preoperative staging in thoracic esophageal cancer. Ann Thorac Surg 68: 2059–2064
Parmar KS, Zwischenberger JB, Reeves AL, Waxman I (2002) Clinical impact of endoscopic ultrasound-guided fine needle aspiration of celiac axis lymph nodes (M1a disease) in esophageal cancer. Ann Thorac Surg 73: 916–920; discussion 920, 921
Pedrazzani C, Bernini M, Giacopuzzi S, Pugliese R, Catalano F, Festini M, Rodella L, de Manzoni G (2005) Evaluation of Siewert classification in gastro-esophageal junction adenocarcinoma: what is the role of endoscopic ultrasonography? J Surg Oncol 91: 226–231
Pham T, Roach E, Falk GL, Chu J, Ngu MC, Jones DB (1998) Staging of oesophageal carcinoma by endoscopic ultrasound: preliminary experience. Aust NZ J Surg 68: 209–212
Quint LE, Glazer GM, Orringer MB, Gross BH (1985) Esophageal carcinoma: CT findings. Radiology 155: 171–175
Quint LE, Hepburn LM, Francis IR, Whyte RI, Orringer MB (1995) Incidence and distribution of distant metastases from newly diagnosed esophageal carcinoma. Cancer 76: 1120–1125
Rankin SC, Taylor H, Cook GJ, Mason R (1998) Computed tomography and positron emission tomography in the pre-operative staging of oesophageal carcinoma. Clin Radiol 53: 659–665
Rasanen JV, Sihvo EI, Knuuti MJ, Minn HR, Luostarinen ME, Laippala P, Viljanen T, Salo JA (2003) Prospective analysis of accuracy of positron emission tomography, computed tomography, and endoscopic ultrasonography in staging of adenocarcinoma of the esophagus and the esophagogastric junction. Ann Surg Oncol 10: 954–960
Rice TW, Boyce GA, Sivak MV (1991) Esophageal ultrasound and the preoperative staging of carcinoma of the esophagus. J Thorac Cardiovasc Surg 101: 536–543
Richards DG, Brown TH, Manson JM (2000) Endoscopic ultrasound in the staging of tumours of the oesophagus and gastro-oesophageal junction. Ann R Coll Surg Engl 82: 311–317
Salminen JT, Farkkila MA, Ramo OJ, Toikkanen V, Simpanen J, Nuutinen H, Salo JA (1999) Endoscopic ultrasonography in the preoperative staging of adenocarcinoma of the distal oesophagus and oesophagogastric junction. Scand J Gastroenterol 34: 1178–1182
Shinkai M, Niwa Y, Arisawa T, Ohmiya N, Goto H, Hayakawa T (2000) Evaluation of prognosis of squamous cell carcinoma of the oesophagus by endoscopic ultrasonography. Gut 47: 120–125
Sihvo EI, Rasanen JV, Knuuti MJ, Minn HR, Luostarinen ME, Viljanen T, Farkkila MA, Salo JA (2004) Adenocarcinoma of the esophagus and the esophagogastric junction: positron emission tomography improves staging and prediction of survival in distant but not in locoregional disease. J Gastrointest Surg 8: 988–996
Sondenaa K, Skaane P, Nygaard K, Skjennald A (1992) Value of computed tomography in preoperative evaluation of resectability and staging in oesophageal carcinoma. Eur J Surg 158: 537–540
Terrin N, Schmid CH, Lau J (2005) In an empirical evaluation of the funnel plot, researchers could not visually identify publication bias. J Clin Epidemiol 58: 894–901
Thompson WM (1997) Esophageal carcinoma. Abdom Imaging 22: 138–142
Tio TL, Coene PP, den Hartog Jager FC, Tytgat GN (1990) Preoperative TNM classification of esophageal carcinoma by endosonography. Hepatogastroenterology 37: 376–381
Van Overhagen H, Lameris JS, Berger MY, Tilanus HW, Van Pel R, Klooswijk AI, Schutte HE (1993) Improved assessment of supraclavicular and abdominal metastases in oesophageal and gastro-oesophageal junction carcinoma with the combination of ultrasound and computed tomography. Br J Radiol 66: 203–208
van Vliet EP, Eijkemans MJ, Poley JW, Steyerberg EW, Kuipers EJ, Siersema PD (2006) Staging of esophageal carcinoma in a low-volume EUS center compared with reported results from high-volume centers. Gastrointest Endosc 63: 938–947
van Westreenen HL, Heeren PA, van Dullemen HM, van der Jagt EJ, Jager PL, Groen H, Plukker JT (2005) Positron emission tomography with F-18-fluorodeoxyglucose in a combined staging strategy of esophageal cancer prevents unnecessary surgical explorations. J Gastrointest Surg 9: 54–61
van Westreenen HL, Westerterp M, Bossuyt PM, Pruim J, Sloof GW, van Lanschot JJ, Groen H, Plukker JT (2004) Systematic review of the staging performance of 18F-fluorodeoxyglucose positron emission tomography in esophageal cancer. J Clin Oncol 22: 3805–3812
Vazquez-Sequeiros E, Norton ID, Clain JE, Wang KK, Affi A, Allen M, Deschamps C, Miller D, Salomao D, Wiersema MJ (2001) Impact of EUS-guided fine-needle aspiration on lymph node staging in patients with esophageal carcinoma. Gastrointest Endosc 53: 751–757
Vazquez-Sequeiros E, Wiersema MJ, Clain JE, Norton ID, Levy MJ, Romero Y, Salomao D, Dierkhising R, Zinsmeister AR (2003) Impact of lymph node staging on therapy of esophageal carcinoma. Gastroenterology 125: 1626–1635
Vickers J (1998) Role of endoscopic ultrasound in the preoperative assessment of patients with oesophageal cancer. Ann R Coll Surg Engl 80: 233–239
Watt I, Stewart I, Anderson D, Bell G, Anderson JR (1989) Laparoscopy, ultrasound and computed tomography in cancer of the oesophagus and gastric cardia: a prospective comparison for detecting intra-abdominal metastases. Br J Surg 76: 1036–1039
Wren SM, Stijns P, Srinivas S (2002) Positron emission tomography in the initial staging of esophageal cancer. Arch Surg 137: 1001–1006; discussion 1006, 1007
Wu LF, Wang BZ, Feng JL, Cheng WR, Liu GR, Xu XH, Zheng ZC (2003) Preoperative TN staging of esophageal cancer: comparison of miniprobe ultrasonography, spiral CT and MRI. World J Gastroenterol 9: 219–224
Yoon YC, Lee KS, Shim YM, Kim BT, Kim K, Kim TS (2003) Metastasis to regional lymph nodes in patients with esophageal squamous cell carcinoma: CT vs FDG PET for presurgical detection prospective study. Radiology 227: 764–770
Yoshikane H, Tsukamoto Y, Niwa Y, Goto H, Hase S, Shimodaira M, Maruta S, Miyata A, Yoshida M (1994) Superficial esophageal carcinoma: evaluation by endoscopic ultrasonography. Am J Gastroenterol 89: 702–707
Ziegler K, Sanft C, Zeitz M, Friedrich M, Stein H, Haring R, Riecken EO (1991) Evaluation of endosonography in TN staging of oesophageal cancer. Gut 32: 16–20
Acknowledgements
The first author of this article was funded by a grant from the ‘Doelmatigheidsonderzoek’ fund of the Erasmus MC – University Medical Center Rotterdam, The Netherlands.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
van Vliet, E., Heijenbrok-Kal, M., Hunink, M. et al. Staging investigations for oesophageal cancer: a meta-analysis. Br J Cancer 98, 547–557 (2008). https://doi.org/10.1038/sj.bjc.6604200
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604200
Keywords
This article is cited by
-
McKeown esophagectomy for a thoracic esophageal carcinoma patient who has a history of definitive chemoradiotherapy for esophageal carcinoma and total pharyngolaryngectomy for hypopharyngeal cancer
World Journal of Surgical Oncology (2023)
-
18F-FDG-PET/CT to Detect Pathological Complete Response After Neoadjuvant Treatment in Patients with Cancer of the Esophagus or Gastroesophageal Junction: Accuracy and Long-Term Implications
Journal of Gastrointestinal Cancer (2023)
-
Approach to Localized Squamous Cell Cancer of the Esophagus
Current Treatment Options in Oncology (2022)
-
Pentixafor PET/CT for imaging of chemokine receptor 4 expression in esophageal cancer – a first clinical approach
Cancer Imaging (2021)
-
A DNA-damage immune response assay combined with PET biomarkers predicts response to neo-adjuvant chemotherapy and survival in oesophageal adenocarcinoma
Scientific Reports (2021)