Abstract
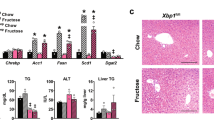
Production of bile by the liver is crucial for the absorption of lipophilic nutrients. Dysregulation of bile acid homeostasis can lead to cholestatic liver disease and endoplasmic reticulum (ER) stress. We show by global location analysis ('ChIP-on-chip') and cell type–specific gene ablation that the winged helix transcription factor Foxa2 is required for normal bile acid homeostasis. As suggested by the location analysis, deletion of Foxa2 in hepatocytes in mice using the Cre-lox system leads to decreased transcription of genes encoding bile acid transporters on both the basolateral and canalicular membranes, resulting in intrahepatic cholestasis. Foxa2-deficient mice are strikingly sensitive to a diet containing cholic acid, which results in toxic accumulation of hepatic bile salts, ER stress and liver injury. In addition, we show that expression of FOXA2 is markedly decreased in liver samples from individuals with different cholestatic syndromes, suggesting that reduced FOXA2 abundance could exacerbate the injury.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Accession codes
References
Kaestner, K.H. The hepatocyte nuclear factor 3 (HNF3 or FOXA) family in metabolism. Trends Endocrinol. Metab. 11, 281–285 (2000).
Costa, R.H., Grayson, D.R. & Darnell, J.E., Jr. Multiple hepatocyte-enriched nuclear factors function in the regulation of transthyretin and α1-antitrypsin genes. Mol. Cell. Biol. 9, 1415–1425 (1989).
Ang, S.L. et al. The formation and maintenance of the definitive endoderm lineage in the mouse: involvement of HNF3/forkhead proteins. Development 119, 1301–1315 (1993).
Monaghan, A.P., Kaestner, K.H., Grau, E. & Schutz, G. Postimplantation expression patterns indicate a role for the mouse forkhead/HNF-3 α, β and γ genes in determination of the definitive endoderm, chordamesoderm and neuroectoderm. Development 119, 567–578 (1993).
Lee, C.S., Friedman, J.R., Fulmer, J.T. & Kaestner, K.H. The initiation of liver development is dependent on Foxa transcription factors. Nature 435, 944–947 (2005).
Zhang, L., Rubins, N.E., Ahima, R.S., Greenbaum, L.E. & Kaestner, K.H. Foxa2 integrates the transcriptional response of the hepatocyte to fasting. Cell Metab. 2, 141–148 (2005).
Suzuki, K. et al. Epididymis-specific promoter–driven gene targeting: a transcription factor which regulates epididymis-specific gene expression. Mol. Cell. Endocrinol. 250, 184–189 (2006).
Carroll, J.S. et al. Chromosome-wide mapping of estrogen receptor binding reveals long-range regulation requiring the forkhead protein FoxA1. Cell 122, 33–43 (2005).
Laganiere, J. et al. From the Cover: Location analysis of estrogen receptor α target promoters reveals that FOXA1 defines a domain of the estrogen response. Proc. Natl. Acad. Sci. USA 102, 11651–11656 (2005).
Wolfrum, C., Asilmaz, E., Luca, E., Friedman, J.M. & Stoffel, M. Foxa2 regulates lipid metabolism and ketogenesis in the liver during fasting and in diabetes. Nature 432, 1027–1032 (2004).
Lantz, K.A. et al. Foxa2 regulates multiple pathways of insulin secretion. J. Clin. Invest. 114, 512–520 (2004).
Rausa, F.M. et al. Elevated levels of hepatocyte nuclear factor 3β in mouse hepatocytes influence expression of genes involved in bile acid and glucose homeostasis. Mol. Cell. Biol. 20, 8264–8282 (2000).
Goodwin, B. et al. A regulatory cascade of the nuclear receptors FXR, SHP-1 and LRH-1 represses bile acid biosynthesis. Mol. Cell 6, 517–526 (2000).
Lu, T.T. et al. Molecular basis for feedback regulation of bile acid synthesis by nuclear receptors. Mol. Cell 6, 507–515 (2000).
Sinal, C.J. et al. Targeted disruption of the nuclear receptor FXR/BAR impairs bile acid and lipid homeostasis. Cell 102, 731–744 (2000).
Wang, L. et al. Redundant pathways for negative feedback regulation of bile acid production. Dev. Cell 2, 721–731 (2002).
Fischer, S., Beuers, U., Spengler, U., Zwiebel, F.M. & Koebe, H.G. Hepatic levels of bile acids in end-stage chronic cholestatic liver disease. Clin. Chim. Acta 251, 173–186 (1996).
Zollner, G. et al. Role of nuclear receptors and hepatocyte-enriched transcription factors for Ntcp repression in biliary obstruction in mouse liver. Am. J. Physiol. Gastrointest. Liver Physiol. 289, G798–G805 (2005).
Kullak-Ublick, G.A., Stieger, B. & Meier, P.J. Enterohepatic bile salt transporters in normal physiology and liver disease. Gastroenterology 126, 322–342 (2004).
Eloranta, J.J. & Kullak-Ublick, G.A. Coordinate transcriptional regulation of bile acid homeostasis and drug metabolism. Arch. Biochem. Biophys. 433, 397–412 (2005).
Mennone, A. et al. Mrp4−/− mice have an impaired cytoprotective response in obstructive cholestasis. Hepatology 43, 1013–1021 (2006).
Hagenbuch, B. & Meier, P.J. The superfamily of organic anion transporting polypeptides. Biochim. Biophys. Acta 1609, 1–18 (2003).
Lam, P., Wang, R. & Ling, V. Bile acid transport in sister of P-glycoprotein (ABCB11) knockout mice. Biochemistry 44, 12598–12605 (2005).
Fernandez-Checa, J.C., Takikawa, H., Horie, T., Ookhtens, M. & Kaplowitz, N. Canalicular transport of reduced glutathione in normal and mutant Eisai hyperbilirubinemic rats. J. Biol. Chem. 267, 1667–1673 (1992).
Geier, A. et al. Characterization of organic anion transporter regulation, glutathione metabolism and bile formation in the obese Zucker rat. J. Hepatol. 43, 1021–1030 (2005).
Ruiz, M.L. et al. Beneficial effect of spironolactone administration on ethynylestradiol-induced cholestasis in the rat: involvement of up-regulation of multidrug resistance–associated protein 2. Drug Metab. Dispos. 35, 2060–2066 (2007).
Ballatori, N. & Truong, A.T. Glutathione as a primary osmotic driving force in hepatic bile formation. Am. J. Physiol. 263, G617–G624 (1992).
Zollner, G. et al. Hepatobiliary transporter expression in percutaneous liver biopsies of patients with cholestatic liver diseases. Hepatology 33, 633–646 (2001).
Oswald, M., Kullak-Ublick, G.A., Paumgartner, G. & Beuers, U. Expression of hepatic transporters OATP-C and MRP2 in primary sclerosing cholangitis. Liver 21, 247–253 (2001).
Zhang, Y., Kast-Woelbern, H.R. & Edwards, P.A. Natural structural variants of the nuclear receptor farnesoid X receptor affect transcriptional activation. J. Biol. Chem. 278, 104–110 (2003).
Guo, G.L. et al. Complementary roles of farnesoid X receptor, pregnane X receptor and constitutive androstane receptor in protection against bile acid toxicity. J. Biol. Chem. 278, 45062–45071 (2003).
Shih, D.Q. et al. Hepatocyte nuclear factor-1α is an essential regulator of bile acid and plasma cholesterol metabolism. Nat. Genet. 27, 375–382 (2001).
Coffinier, C. et al. Bile system morphogenesis defects and liver dysfunction upon targeted deletion of HNF1β. Development 129, 1829–1838 (2002).
Inoue, Y., Yu, A.M., Inoue, J. & Gonzalez, F.J. Hepatocyte nuclear factor 4α is a central regulator of bile acid conjugation. J. Biol. Chem. 279, 2480–2489 (2004).
Hubbard, B. et al. Mice deleted for fatty acid transport protein 5 have defective bile acid conjugation and are protected from obesity. Gastroenterology 130, 1259–1269 (2006).
Bernstein, H. et al. Activation of the promoters of genes associated with DNA damage, oxidative stress, ER stress and protein malfolding by the bile salt, deoxycholate. Toxicol. Lett. 108, 37–46 (1999).
Riggs, A.C. et al. Mice conditionally lacking the Wolfram gene in pancreatic islet β cells exhibit diabetes as a result of enhanced endoplasmic reticulum stress and apoptosis. Diabetologia 48, 2313–2321 (2005).
Menendez-Benito, V., Verhoef, L.G., Masucci, M.G. & Dantuma, N.P. Endoplasmic reticulum stress compromises the ubiquitin-proteasome system. Hum. Mol. Genet. 14, 2787–2799 (2005).
Zhao, L., Longo-Guess, C., Harris, B.S., Lee, J.W. & Ackerman, S.L. Protein accumulation and neurodegeneration in the woozy mutant mouse is caused by disruption of SIL1, a cochaperone of BiP. Nat. Genet. 37, 974–979 (2005).
Vendemiale, G., Grattagliano, I., Lupo, L., Memeo, V. & Altomare, E. Hepatic oxidative alterations in patients with extra-hepatic cholestasis. Effect of surgical drainage. J. Hepatol. 37, 601–605 (2002).
Zollner, G., Marschall, H.U., Wagner, M. & Trauner, M. Role of nuclear receptors in the adaptive response to bile acids and cholestasis: pathogenetic and therapeutic considerations. Mol. Pharm. 3, 231–251 (2006).
Xie, W. et al. An essential role for nuclear receptors SXR/PXR in detoxification of cholestatic bile acids. Proc. Natl. Acad. Sci. USA 98, 3375–3380 (2001).
Staudinger, J.L. et al. The nuclear receptor PXR is a lithocholic acid sensor that protects against liver toxicity. Proc. Natl. Acad. Sci. USA 98, 3369–3374 (2001).
Bombail, V., Taylor, K., Gibson, G.G. & Plant, N. Role of Sp1, C/EBP α, HNF3, and PXR in the basal- and xenobiotic-mediated regulation of the CYP3A4 gene. Drug Metab. Dispos. 32, 525–535 (2004).
Sund, N.J. et al. Hepatocyte nuclear factor 3β (Foxa2) is dispensable for maintaining the differentiated state of the adult hepatocyte. Mol. Cell. Biol. 20, 5175–5183 (2000).
Denson, L.A. et al. The orphan nuclear receptor, Shp, mediates bile acid–induced inhibition of the rat bile acid transporter, Ntcp. Gastroenterology 121, 140–147 (2001).
Zollner, G. et al. Induction of short heterodimer partner 1 precedes downregulation of Ntcp in bile duct–ligated mice. Am. J. Physiol. Gastrointest. Liver Physiol. 282, G184–G191 (2002).
Lai, E., Prezioso, V.R., Tao, W.F., Chen, W.S. & Darnell, J.E., Jr. Hepatocyte nuclear factor 3 α belongs to a gene family in mammals that is homologous to the Drosophila homeotic gene fork head. Genes Dev. 5, 416–427 (1991).
Wang, R. et al. Targeted inactivation of sister of P-glycoprotein gene (Spgp) in mice results in nonprogressive but persistent intrahepatic cholestasis. Proc. Natl. Acad. Sci. USA 98, 2011–2016 (2001).
Wang, R. et al. Severe cholestasis induced by cholic acid feeding in knockout mice of sister of P-glycoprotein. Hepatology 38, 1489–1499 (2003).
Pauli-Magnus, C. et al. BSEP and MDR3 haplotype structure in healthy Caucasians, primary biliary cirrhosis and primary sclerosing cholangitis. Hepatology 39, 779–791 (2004).
Besnard, V., Wert, S.E., Hull, W.M. & Whitsett, J.A. Immunohistochemical localization of Foxa1 and Foxa2 in mouse embryos and adult tissues. Gene Expr. Patterns 5, 193–208 (2004).
Rubins, N.E. et al. Transcriptional networks in the liver: hepatocyte nuclear factor 6 function is largely independent of Foxa2. Mol. Cell. Biol. 25, 7069–7077 (2005).
Tusher, V.G., Tibshirani, R. & Chu, G. Significance analysis of microarrays applied to the ionizing radiation response. Proc. Natl. Acad. Sci. USA 98, 5116–5121 (2001).
Acknowledgements
We thank D.D. Moore for advice on the cholic acid diet; J.A. Whittsett (Cincinnati Children's Hospital Medical Center and The University of Cincinnati College of Medicine) for providing rabbit polyclonal antibodies to Foxa2; K. Ma and L.E. Greenbaum for critical reading of the manuscript; D. Ye, A. Arsenlis, G. Tuteja and N. Gao for contributions to this project; and E. Rand, and the Fred and Suzanne Biesecker Pediatric Liver Center for providing pediatric liver samples. We are grateful to S. Hammani and E. Helmbrecht for care of the mice. Our studies were assisted by the University of Pennsylvania Diabetes Center (P30DK19525). This work was supported by grants DK-049210 and DK-056947 to K.H.K. I.M.B. was supported by training grant T32-HG000046 and a Penn Genomics Institute Graduate Fellowship.
Author information
Authors and Affiliations
Contributions
I.M.B. developed the project, performed most of the experiments and data analysis and wrote the draft of the manuscript. N.E.R. and P.W. performed some of the experiments and data analysis. E.E.F. and J.R.F. contributed to the human tissue studies. K.H.K. directed the project and reviewed and edited the manuscript.
Corresponding author
Supplementary information
Supplementary Text and Figures
Supplementary Fig. 1, Supplementary Tables 1–3 and Supplementary Methods (PDF 106 kb)
Rights and permissions
About this article
Cite this article
Bochkis, I., Rubins, N., White, P. et al. Hepatocyte-specific ablation of Foxa2 alters bile acid homeostasis and results in endoplasmic reticulum stress. Nat Med 14, 828–836 (2008). https://doi.org/10.1038/nm.1853
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.1853
This article is cited by
-
miR-195b is required for proper cellular homeostasis in the elderly
Scientific Reports (2024)
-
Time-of-day defines NAD+ efficacy to treat diet-induced metabolic disease by synchronizing the hepatic clock in mice
Nature Communications (2023)
-
The bromodomain inhibitor JQ1 up-regulates the long non-coding RNA MALAT1 in cultured human hepatic carcinoma cells
Scientific Reports (2022)
-
Loss of FOXA2 induces ER stress and hepatic steatosis and alters developmental gene expression in human iPSC-derived hepatocytes
Cell Death & Disease (2022)
-
Endoplasmic reticulum stress-mediated cell death in liver injury
Cell Death & Disease (2022)