Abstract
Background
Nicotine dependence is difficult to treat, and the biological mechanisms that are involved are not entirely clear. There is an urgent need to develop better drugs and more effective treatments for clinical practice. A critical step towards accelerating progress in medication development is to understand the neurobehavioral effects of pharmacotherapies on clinical characteristics associated with nicotine dependence.
Objectives
This review sought to summarize the functional magnetic resonance imaging (fMRI) literature on smoking cessation with the aim to better understand the neural processes underlying the effects of nicotinic and non-nicotinic pharmacological smoking cessation treatments on specific symptoms of nicotine dependence and withdrawal.
Data Sources
We conducted a search in Pubmed, Web of Science and PsycINFO databases with the keywords ‘fMRI’ or ‘functional magnetic resonance imaging’ and ‘tobacco’ or ‘nicotine’ or ‘smok*’. The date of the most recent search was May 2012.
Study Eligibility Criteria, Participants and Interventions
The original studies that were included were those of smokers or nicotine-dependent individuals, published in the English language, with pharmacological treatment for nicotine dependence and use of fMRI with blood oxygen level-dependent (BOLD) imaging or continuous arterial spin labelling (CASL). No date limit was applied.
Study Appraisal and Synthesis Methods
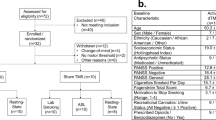
Two of the authors read the abstracts of all studies found in the search (n = 1,260). The inclusion and exclusion criteria were applied, and 1,224 articles were excluded. In a second step, the same authors read the remaining 36 studies. Nineteen of the 36 articles were excluded. The results were tabulated by the number of individuals and their mean age, the main sample characteristics, smoking status, study type and methodology, and the main fMRI findings.
Results
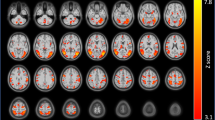
Seventeen original fMRI studies involving pharmacological treatment of smokers were selected. The anterior and posterior cingulate cortex, medial and lateral orbitofrontal cortex, ventral striatum, amygdala, thalamus and insula are heavily involved in the maintenance of smoking and nicotine withdrawal. The effects of varenicline and bupropion in alleviating withdrawal symptoms and decreasing smoking correlated with modulation of the activities of these areas. Nicotine replacement therapy seems to improve cognitive symptoms related to withdrawal especially by modulating activities of the default-network regions; however, nicotine replacement does not necessarily alter the activities of neural circuits, such as the cingulate cortices, that are associated with nicotine addiction.
Limitations
The risk of bias in individual studies, and across studies, was not assessed, and no method of handling data and combining results of studies was carried out. Most importantly, positron emission tomography (PET) studies were not included in this review.
Conclusions and Implication of Key Findings
fMRI studies delineate brain systems that contribute to cognitive deficits and reactivity to stimuli that generate the desire to smoke. Nicotinic and non-nicotinic pharmacotherapy may reduce smoking via distinct neural mechanisms of action. These findings should contribute to the development of new medications and discovery of early markers of the therapeutic response of cigarette smokers.



Similar content being viewed by others
References
Royal College of Physicians. Harm reduction in nicotine addiction: helping people who can’t quit. A report by the Tobacco Advisory Group of the Royal College of Physicians. London: RCP; 2007.
Hughes JR, Peters EN, Naud S. Relapse to smoking after 1 year of abstinence: a meta-analysis. Addict Behav. 2008;33:1516–20.
Lerman C, LeSage MG, Perkins KA, O’Malley SS, Siegel SJ, Benowitz NL, Corrigall WA. Translational research in medication development for nicotine dependence. Nat Rev Drug Discov. 2007;6:746–62.
Henningfield JE, Shiffman S, Ferguson SG, Gritz ER. Tobacco dependence and withdrawal: science base, challenges and opportunities for pharmacotherapy. Pharmacol Ther. 2009;123(1):1–16.
Watkins SS, Koob GF, Markou A. Neural mechanisms underlying nicotine addiction: acute positive reinforcement and withdrawal. Nicotine Tob Res. 2000;2:19–37.
Hughes JR. Effects of abstinence from tobacco: valid symptoms and time course. Nicotine Tob Res. 2007;9:315–27.
Grieder TE, George O, Tan H, George SR, Le Foll B, Laviolette SR, van der Kooy D. Phasic D1 and tonic D2 dopamine receptor signaling double dissociate the motivational effects of acute nicotine and chronic nicotine withdrawal. Proc Natl Acad Sci USA. 2012;109(8):3101–6.
Hyman SE, Fenton WS. Medicine: what are the right targets for psychopharmacology? Science. 2003;299:350–1.
Conn PJ, Roth BL. Opportunities and challenges of psychiatric drug discovery: roles for scientists in academic, industry, and government settings. Neuropsychopharmacology. 2008;33:2048–60.
Moher D, Liberati A, Tetzlaff J, Altan DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009;6(6):e1000097.
Franklin T, Wang Z, Suh JJ, Hazan R, Cruz J, Li Y, Goldman M, Detre JA, O’Brien CP, Childress AR. Effects of varenicline on smoking cue-triggered neural and craving responses. Arch Gen Psychiatry. 2011;68(5):516–26.
Loughead J, Ray R, Wileyto EP, Ruparel K, Sanborn P, Siegel S, Gur RC, Lerman C. Effects of the alpha4beta2 partial agonist varenicline on brain activity and working memory in abstinent smokers. Biol Psychiatry. 2010;67(8):715–21.
Loughead J, Ray R, Wileyto EP, Ruparel K, O'Donnell GP, Senecal N, Siegel S, Gur RC, Lerman C. Brain activity and emotional processing in smokers treated with varenicline. Addict Biol. 2013;18(4):732–8.
Shiffman SM, Jarvik ME. Smoking withdrawal symptoms in 2 weeks of abstinence. Psychopharmacology. 1976;50(1):35–9.
Culbertson CS, Bramen J, Cohen MS, London ED, Olmstead RE, Gan JJ, Costello MR, Shulenberger S, Mandelkern MA, Brody AL. Effect of bupropion treatment on brain activation induced by cigarette-related cues in smokers. Arch Gen Psychiatry. 2011;68(5):505–15.
Franklin TR, Wang Z, Sciortino N, Harper D, Li Y, Hakun J, Kildea S, Kampman K, Ehrman R, Detre JA, O’Brien CP, Childress AR. Modulation of resting brain cerebral blood flow by the GABA B agonist, baclofen: a longitudinal perfusion fMRI study. Drug Alcohol Depend. 2011;117(2–3):176–83.
Franklin TR, Shin J, Jagannathan K, Suh JJ, Detre JA, O’Brien CP, Childress AR. Acute baclofen diminishes resting baseline blood flow to limbic structures: a perfusion fMRI study. Drug Alcohol Depend. 2012;125(1–2):60–6.
Cole DM, Beckmann CF, Long CJ, Matthews PM, Durcan MJ, Beaver JD. Nicotine replacement in abstinent smokers improves cognitive withdrawal symptoms with modulation of resting brain network dynamics. Neuroimage. 2010;52(2):590–9.
Hahn B, Ross TJ, Wolkenberg FA, Shakleya DM, Huestis MA, Stein EA. Performance effects of nicotine during selective attention, divided attention, and simple stimulus detection: an fMRI study. Cereb Cortex. 2009;19(9):1990–2000.
Hahn B, Ross TJ, Yang Y, Kim I, Huestis MA, Stein EA. Nicotine enhances visuospatial attention by deactivating areas of the resting brain default network. J Neurosci. 2007;27(13):3477–89.
Hong LE, Gu H, Yang Y, Ross TJ, Salmeron BJ, Buchholz B, Thaker GK, Stein EA. Association of nicotine addiction and nicotine’s actions with separate cingulate cortex functional circuits. Arch Gen Psychiatry. 2009;66(4):431–41.
Janes AC, Frederick B, Richardt S, Burbridge C, Merlo-Pich E, Renshaw PF, Evins AE, Fava M, Kaufman MJ. Brain fMRI reactivity to smoking-related images before and during extended smoking abstinence. Exp Clin Psychopharmacol 2009;17(6):365–73. (Erratum in: Exp Clin Psychopharmacol 2010;18(3):296).
Lawrence NS, Ross TJ, Stein EA. Cognitive mechanisms of nicotine on visual attention. Neuron. 2002;36(3):539–48.
McClernon FJ, Hiott FB, Liu J, Salley AN, Behm FM, Rose JE. Selectively reduced responses to smoking cues in amygdala following extinction-based smoking cessation: results of a preliminary functional magnetic resonance imaging study. Addict Biol. 2007;12(3–4):503–12.
Rose JE, Ross TJ, Kurup PK, Stein EA. Nicotine modulation of information processing is not limited to input (attention) but extends to output (intention). Psychopharmacology. 2010;209(4):291–302.
Rose JE, Ross TJ, Salmeron BJ, Lee M, Shakleya DM, Huestis M, Stein EA. Chronic exposure to nicotine is associated with reduced reward-related activity in the striatum but not the midbrain. Biol Psychiatry. 2012;71(3):206–13.
Sutherland MT, Ross TJ, Shakleya DM, Huestis MA, Stein EA. Chronic smoking, but not acute nicotine administration, modulates neural correlates of working memory. Psychopharmacology. 2011;213(1):29–42.
Sweet LH, Mulligan RC, Finnerty CE, Jerskey BA, David SP, Cohen RA, Niaura RS. Effects of nicotine withdrawal on verbal working memory and associated brain response. Psychiatry Res. 2010;183(1):69–74.
Staley JK, Krishnan-Sarin S, Cosgrove KP, Krantzler E, Frohlich E, Perry E, Dubin JA, Estok K, Brenner E, Baldwin RM, Tamagnan GD, Seibyl JP, Jatlow P, Picciotto MR, London ED, O’Malley S, van Dyck CH. Human tobacco smokers in early abstinence have higher levels of beta2* nicotinic acetylcholine receptors than nonsmokers. J Neurosci. 2006;26:8707–14.
Patterson F, Jepson C, Strasser AA, Loughead J, Perkins KA, Gur RC, Frey JM, Siegel S, Lerman C. Varenicline improves mood and cognition during smoking abstinence. Biol Psychiatry. 2009;65:144–9.
Franklin TR, Wang Z, Wang J, Sciortino N, Harper D, Li Y, Ehrman R, Kampman K, O’Brien CP, Detre JA, Childress AR. Limbic activation to cigarette smoking cues independent of nicotine withdrawal: a perfusion fMRI study. Neuropsychopharmacology. 2007;32(11):2301–9.
Cardinal RN, Parkinson JA, Hall J, Everitt BJ. Emotion and motivation: the role of the amygdala, ventral striatum, and prefrontal cortex. Neurosci Biobehav Rev. 2002;26(3):321–52.
Kringelbach ML. The human orbitofrontal cortex: linking reward to hedonic experience. Nat Rev Neurosci. 2005;6(9):691–702.
Elliott R, Dolan RJ, Frith CD. Dissociable functions in the medial and lateral orbitofrontal cortex: evidence from human neuroimaging studies. Cereb Cortex. 2000;10(3):308–17.
Jacobsen LK, Krystal JH, Mencl WE, Westerveld M, Frost SJ, Pugh KR. Effects of smoking and smoking abstinence on cognition in adolescent tobacco smokers. Biol Psychiatry. 2005;57:56–66.
Mendrek A, Monterosso J, Simon SL, Jarvik M, Brody A, Olmstead R, Domier CP, Cohen MS, Ernst M, London ED. Working memory in cigarette smokers: comparison to nonsmokers and effects of abstinence. Addict Behav. 2006;31:833–44.
Procyk E, Goldman-Rakic PS. Modulation of dorsolateral prefrontal delay activity during self-organized behavior. J Neurosci. 2006;26:11313–23.
Carter CS, Van Veen V. Anterior cingulate cortex and conflict detection: an update of theory and data. Cogn Affect Behav Neurosci. 2007;7:367–79.
Behrens TEJ, Johansen-Berg H, Woolrich MW, Smith SM, Wheeler-Kingshott CAM, Boulby PA, Barker GJ, Sillery EL, Sheehan K, Ciccarelli O, Thompson AJ, Brady JM, Matthews PM. Non-invasive mapping of connections between human thalamus and cortex using diffusion imaging. Nat Neurosci. 2003;6:750–7.
Hayashi T, Ko JH, Strafella AP, Dagher A. Dorsolateral prefrontal and orbitofrontal cortex interactions during self-control of cigarette craving. Proc Natl Acad Sci USA. 2013;110(11):4422–7.
Raw M, Regan S, Rigotti NA, McNeill A. A survey of tobacco dependence treatment guidelines in 31 countries. Addiction. 2009;104(7):1243–50.
Strong DR, Kahler CW, Leventhal AM, Abrantes AM, Lloyd-Richardson E, Niaura R, Brown RA. Impact of bupropion and cognitive-behavioral treatment for depression on positive affect, negative affect, and urges to smoke during cessation treatment. Nicotine Tob Res. 2009;11(10):1142–53.
Bush G, Luu P, Posner MI. Cognitive and emotional influences in anterior cingulate cortex. Trends Cogn Sci. 2000;4(6):215–22.
Pastor A, Jones DM, Currie J. High-dose baclofen for treatment-resistant alcohol dependence. J Clin Psychopharmacol. 2012;32(2):266–8.
Muzyk AJ, Rivelli SK, Gagliardi JP. Defining the role of baclofen for the treatment of alcohol dependence: a systematic review of the evidence. CNS Drugs. 2012;26(1):69–78.
Addolorato G, Leggio L. Safety and efficacy of baclofen in the treatment of alcohol-dependent patients. Curr Pharm Des. 2010;16(19):2113–7.
Addolorato G, Leggio L, Ferrulli A, Cardone S, Bedogni G, Caputo F, Gasbarrini G, Landolfi R. Dose-response effect of baclofen in reducing daily alcohol intake in alcohol dependence: secondary analysis of a randomized, double-blind, placebo-controlled trial. Alcohol Alcohol. 2011;46(3):312–7.
Garbutt JC, Kampov-Polevoy AB, Gallop R, Kalka-Juhl L, Flannery BA. Efficacy and safety of baclofen for alcohol dependence: a randomized, double-blind, placebo-controlled trial. Alcohol Clin Exp Res. 2010;34(11):1849–57.
Franklin TR, Harper D, Kampman K, Kildea-McCrea S, Jens W, Lynch KG, O’Brien CP, Childress AR. The GABA B agonist baclofen reduces cigarette consumption in a preliminary double-blind placebo-controlled smoking reduction study. Drug Alcohol Depend. 2009;103:30–6.
See RE, Fuchs RA, Ledford CC, McLaughlin J. Drug addiction, relapse, and the amygdala. Ann NY Acad Sci. 2003;985:294–307.
Naqvi NH, Rudrauf D, Damasio H, Bechara A. Damage to the insula disrupts addiction to cigarette smoking. Science. 2007;315:531–4.
Craig AD. How do you feel—now? The anterior insula and human awareness. Nat Rev Neurosci. 2009;10:59–70.
Jarraya B, Brugières P, Tani N, Hodel J, Grandjacques B, Fénelon G, Decq P, Palfi S. Disruption of cigarette smoking addiction after posterior cingulate damage. J Neurosurg. 2010;113(6):1219–21.
Stead LF, Perera R, Bullen C, Mant D, Lancaster T. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev 2008;23(1):CD000146.
Stead LF, Perera R, Bullen C, Mant D, Hartmann-Boyce J, Cahill K, Lancaster T. Nicotine replacement therapy for smokng cessation. Cochrane Database Syst Rev 2012;11:CD000146.
Evans DE, Drobes DJ. Nicotine self-medication of cognitive-attentional processing. Addict Biol. 2009;14:32–42.
Heishman SJ, Kleykamp BA, Singleton EG. Meta-analysis of the acute effects of nicotine and smoking on human performance. Psychopharmacology. 2010;210(4):453–69.
Gusnard DA, Akbudak E, Shulman GL, Raichle ME. Medial prefrontal cortex and self-referential mental activity: relation to a default mode of brain function. Proc Natl Acad Sci USA. 2001;98:4259–64.
Shulman GL, Fiez JA, Corbetta M, Buckner RL, Miezin FM, Raichle ME, Petersen SE. Common blood flow changes across visual tasks: II. Decreases in cerebral cortex. J Cogn Neurosci. 1997;9:648–63.
McKiernan KA, Kaufman JN, Kucera-Thompson J, Binder JR. A parametric manipulation of factors affecting task-induced deactivation in functional neuroimaging. J Cogn Neurosci. 2003;15:394–408.
Caggiula AR, Donny EC, Chaudhri N, Perkins KA, Evans-Martin FF, Sved AF. Importance of nonpharmacological factors in nicotine self-administration. Physiol Behav. 2002;77:683–7.
Rose JE, Behm FM, Westman EC, Bates JE, Salley A. Pharmacologic and sensorimotor components of satiation in cigarette smoking. Pharmacol Biochem Behav. 2003;76:243–50.
Rose JE, Behm FM, Westman EC, Kukovich P. Precessation treatment with nicotine skin patch facilitates smoking cessation. Nicotine Tob Res. 2006;8:89–101.
Due D, Huettel SA, Hall WG, Rubin DC. Activation in mesolimbic and visuospatial neural circuits elicited by smoking cues: evidence from functional magnetic resonance imaging. Am J Psychiatry. 2002;159:954–60.
George MS, Anton RF, Bloomer C, Teneback C, Drobes DJ, Lorberbaum JP, Nahas Z, Vincent DJ. Activation of prefrontal cortex and anterior thalamus in alcoholic subjects on exposure to alcohol-specific cues. Arch Gen Psychiatry. 2001;58:345–52.
Rose JE, Behm FM, Salley AN, Bates JE, Coleman RE, Hawk TC, Turkington TG. Regional brain activity correlates of nicotine dependence. Neuropsychopharmacology. 2007;32(12):2441–52.
Atzori G, Lemmonds CA, Kotler ML, Durcan MJ, Boyle J. Efficacy of a nicotine (4 mg)-containing lozenge on the cognitive impairment of nicotine withdrawal. J Clin Psychopharmacol. 2008;28(6):667–74.
Moore CM, Wardrop M, deB Frederick B, Renshaw PF. Topiramate raises anterior cingulate cortex glutamine levels in healthy men; a 4.0 T magnetic resonance spectroscopy study. Psychopharmacology. 2006;188(2):236–43.
Langleben DD, Ruparel K, Elman I, Loughead JW, Busch EL, Cornish J, Lynch KG, Nuwayser ES, Childress AR, O’Brien CP. Extended-release naltrexone modulates brain response to drug cues in abstinent heroin-dependent patients. Addict Biol 2012 [Epub ahead of print].
Rasetti R, Mattay VS, Stankevich B, Skjei K, Blasi G, Sambataro F, Arrillaga-Romany IC, Goldberg TE, Callicott JH, Apud JA, Weinberger DR. Modulatory effects of modafinil on neural circuits regulating emotion and cognition. Neuropsychopharmacology. 2010;35(10):2101–9.
Schnoll RA, Wileyto EP, Pinto A, Leone F, Gariti P, Siegel S, Perkins KA, Dackis C, Heitjan DF, Berrettini W, Lerman C. A placebo-controlled trial of modafinil for nicotine dependence. Drug Alcohol Depend. 2008;98(1–2):86–93.
Moeller SJ, Honorio J, Tomasi D, Parvaz MA, Woicik PA, Volkow ND, Goldstein RZ. Methylphenidate enhances executive function and optimizes prefrontal function in both health and cocaine addiction. Cereb Cortex 2012 [Epub ahead of print].
Bush G, Holmes J, Shin LM, Surman C, Makris N, Mick E, Seidman LJ, Biederman J. Atomoxetine increases fronto-parietal functional MRI activation in attention-deficit/hyperactivity disorder: a pilot study. Psychiatry Res. 2013;211(1):88–91.
Minzenberg MJ, Yoon JH, Carter CS. Modafinil modulation of the default mode network. Psychopharmacology. 2011;215(1):23–31.
Marquand AF, De Simoni S, O’Daly OG, Williams SC, Mourão-Miranda J, Mehta MA. Pattern classification of working memory networks reveals differential effects of methylphenidate, atomoxetine, and placebo in healthy volunteers. Neuropsychopharmacology. 2011;36(6):1237–47.
Acknowledgments
None.
Conflict of interest
Drs. Menossi, Goudriaan, Périco, Nicastri, Andrade, D’Elia, Li, and Castaldelli-Maia have no conflicts of interest related to the content of this review.
Sources of funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Menossi, H.S., Goudriaan, A.E., de Azevedo-Marques Périco, C. et al. Neural Bases of Pharmacological Treatment of Nicotine Dependence - Insights from Functional Brain Imaging: A Systematic Review. CNS Drugs 27, 921–941 (2013). https://doi.org/10.1007/s40263-013-0092-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-013-0092-8