Abstract
Knowledge of estrogen receptor (ER), progesterone receptor (PgR) and human epidermal growth factor receptor-2 (HER2) status is necessary for determining the optimal treatment of breast cancer patients. At the same time, the discordance between marker profiles (ER/PR and HER2) of primary and metastatic breast cancer is well documented. Whether discordant cases are secondary to “clonal selection” in the face of targeted anti-estrogen or anti-HER2 therapy or whether they are a laboratory artifact is still debated; both scenarios are likely. This article outlines current modalities for ER, PR, and HER2 testing in primary breast carcinoma and its metastases and reviews prospective and retrospective studies that have addressed these issues, as well as recent advances in the field.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •Of importance, ••Of major importance
Beslija S,. Bonneterre J,. Burstein HJ, et al.: Third consensus on medical treatment of metastatic breast cancer. Ann Oncol 2009, 20:1771–1785.
Sorlie T, Perou CM, Tibshirani R, et al.: Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci U S A 2001, 98:10869–10874.
Early Breast Cancer Trialists' Collaborative Group (EBCTCG): Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005, 365:1687–1717.
Hudis CA: Trastuzumab—mechanism of action and use in clinical practice. N Engl J Med 2007, 357:39–51.
Wolff AC, Hammond MEH, Schwartz JN, et al.: American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol 2007, 25:118–145.
•• Hammond ME, Hayes DF, Dowsett M, et al.: American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer (unabridged version). Arch Pathol Lab Med 2010, 134:e48–e72. These are detailed recommended guidelines for ER and PgR testing.
Gancberg D, Di Leo A, Cardoso F, et al.: Comparison of HER-2 status between primary breast cancer and corresponding distant metastatic sites. Ann Oncol 2002, 13:1036–1043.
Gong Y, Booser DJ, Sneige N: Comparison of HER-2 status determined by fluorescence in situ hybridization in primary and metastatic breast carcinoma. Cancer 2005, 103:1763–1769.
Zidan J, Dashkovsky I, Stayerman C, et al.: Comparison of HER-2 overexpression in primary breast cancer and metastatic sites and its effect on biological targeting therapy of metastatic disease. Br J Cancer 2005, 93:552–556.
Amir E, Clemons M: Should a biopsy be recommended to confirm metastatic disease in women with breast cancer? Lancet Oncol 2009, 10:933–935.
Broom RJ, Tang PA, Simmons C, et al.: Changes in estrogen receptor, progesterone receptor and Her-2/neu status with time: discordance rates between primary and metastatic breast cancer. Anticancer Res 2009, 29:1557–1562.
Lindström L, Howell S, Âström G, et al.: Controversies in the management of metastatic breast cancer: biologic evaluation of breast cancer—Should metastases be biopsied? In American Society of Clinical Oncology 2010 Educational Book. Alexandria, VA: American Society of Clinical Oncology; 2010:e7–e12.
Kocjan G, Chandra A, Cross P, et al.: BSCC Code of Practice—fine needle aspiration cytology. Cytopathology 2009, 20:283–296.
Youngson BJ, Cranor M, Rosen PP: Epithelial displacement in surgical breast specimens following needling procedures. Am J Surg Pathol 1994, 18:896–903.
Liebens F, Carly B, Cusumano P, et al.: Breast cancer seeding associated with core needle biopsies: a systematic review. Maturitas 2009, 62:113–123.
Liedtke C, Broglio K, Moulder S, et al.: Prognostic impact of discordance between triple-receptor measurements in primary and recurrent breast cancer. Ann Oncol 2009, 20:1953–1958.
Murray MP, Liberman L, Nehhozina T, et al.: Negative estrogen receptor and HER2 assays at core biopsy of invasive cancers should be confirmed in the surgical specimens [poster 6008]. Presented at the 32nd Annual San Antonio Breast Cancer Symposium. San Antonio, TX; December 13, 2009.
Goldstein NS, Ferkowicz M, Odish E, et al.: Minimum formalin fixation time for consistent estrogen receptor immunohistochemical staining of invasive breast carcinoma. Am J Clin Pathol 2003, 120:86–92.
Khoury T, Sait S, Hwang H, et al.: Delay to formalin fixation effect on breast biomarkers. Mod Pathol 2009, 22:1457–1467.
Mullink H, Henzen-Logmans SC, Tadema TM, et al.: Influence of fixation and decalcification on the immunohistochemical staining of cell-specific markers in paraffin-embedded human bone biopsies. J Histochem Cytochem 1985, 33:1103–1109.
Hanley KZ, Birdsong GG, Cohen C, Siddiqui MT: Immunohistochemical detection of estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 expression in breast carcinomas: comparison on cell block, needle-core, and tissue block preparations. Cancer Cytopathol 2009, 117:279–288.
Wolff AC, Hammond ME, Schwartz JN, et al.: American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. Arch Pathol Lab Med 2007, 131:18–43.
Mann GB, Fahey VD, Feleppa F, Buchanan MR: Reliance on hormone receptor assays of surgical specimens may compromise outcome in patients with breast cancer. J Clin Oncol 2005, 23:5148–5154.
Ibarra JA, Rogers LW, Kyshtoobayeva A, Bloom K: Fixation time does not affect the expression of estrogen receptor. Am J Clin Pathol 2010, 133:747–755.
Price JA, Grunfeld E, Barnes PJ, et al.: Inter-institutional pathology consultations for breast cancer: impact on clinical oncology therapy recommendations. Curr Oncol 2010, 17:25–32.
Slamon DJ, Clark GM, Wong SG, et al.: Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 1987, 235:177–182.
Patil A, Nehhozina T, Akram M, et al.: Clinical, morphologic and immunophenotypic characteristics of breast carcinomas with lung metastasis [abstract 214]. Mod Pathol 2008, 21:49A.
• Sauter G, Lee J, Bartlett JM, et al.: Guidelines for human epidermal growth factor receptor 2 testing: biologic and methodologic considerations. J Clin Oncol 2009, 27:1323–1333. This paper addresses biologic and practical aspects related to HER2 testing.
Tapia C, Savic S, Wagner U, et al.: HER2 gene status in primary breast cancers and matched distant metastases. Breast Cancer Res 2007, 9:R31.
Lipton A, Leitzel K, Ali SM, et al.: Serum HER-2/neu conversion to positive at the time of disease progression in patients with breast carcinoma on hormone therapy. Cancer 2005, 104:257–263.
D’Alfonso T, Liu YF, Monni S, et al.: Accurately assessing her-2/neu status in needle core biopsies of breast cancer patients in the era of neoadjuvant therapy: emerging questions and considerations addressed. Am J Surg Pathol 2010, 34:575–581.
Mittendorf EA, Wu Y, Scaltriti M, et al.: Loss of HER2 amplification following trastuzumab-based neoadjuvant systemic therapy and survival outcomes. Clin Cancer Res 2009, 15:7381–7388.
Amir E, Clemons M, Freedman OC, et al.: Tissue confirmation of disease recurrence in patients with breast cancer: pooled analysis of two large prospective studies [abstract]. J Clin Oncol 2010 ASCO Annual Meeting Proceedings (Post-Meeting Edition) 2010, 28(May 20 Suppl):1007.
Simmons C, Miller N, Geddie W, et al.: Does confirmatory tumor biopsy alter the management of breast cancer patients with distant metastases? Ann Oncol 2009, 20:1499–1504.
Karlsson E, Lindstrom LS, Wilking U, et al.: Discordance in hormone receptor status in breast cancer during tumor progression [abstract]. J Clin Oncol 2010 ASCO Annual Meeting Proceedings (Post-Meeting Edition) 2010, 28(May 20 Suppl):1009.
Locatelli M A, Curigliano G, Fumagalli L, et al.: Should liver metastases of breast cancer be biopsied to improve treatment choice? [abstract]. J Clin Oncol 2010 ASCO Annual Meeting Proceedings (Post-Meeting Edition) 2010, 28(June 20 Suppl):CRA1008.
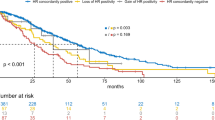
Kuukasjarvi T, Kononen J, Helin H, et al.: Loss of estrogen receptor in recurrent breast cancer is associated with poor response to endocrine therapy. J Clin Oncol 1996, 14:2584–2589.
Arnedos M, Nerurkar A, Osin P, et al.: Discordance between core needle biopsy (CNB) and excisional biopsy (EB) for estrogen receptor (ER), progesterone receptor (PgR) and HER2 status in early breast cancer (EBC). Ann Oncol 2009, 20:1948–1952.
Sharma A, Crook T, Thompson A, Palmieri C: Surgical oncology: why biopsying metastatic breast cancer should be routine. Nat Rev Clin Oncol 2010, 7:72–74.
Kalikaki A, Koutsopoulos A, Trypaki M, et al.: Comparison of EGFR and K-RAS gene status between primary tumours and corresponding metastases in NSCLC. Br J Cancer 2008, 99:923–929.
Navin N, Krasnitz A, Rodgers L, et al.: Inferring tumor progression from genomic heterogeneity. Genome Res 2010, 20:68–80.
• Kim MY, Oskarsson T, Acharyya S, et al.: Tumor self-seeding by circulating cancer cells. Cell 2009, 139:1315–1326. This interesting basic science paper shows that circulating tumor cells can also colonize their tumors of origin (“tumor self-seeding”).
Monaco SE, Nikiforova MN, Cieply K, et al.: A comparison of EGFR and KRAS status in primary lung carcinoma and matched metastases. Hum Pathol 2010, 41:94–102.
Tortola S, Steinert R, Hantschick M, et al.: Discordance between K-ras mutations in bone marrow micrometastases and the primary tumor in colorectal cancer. J Clin Oncol 2001, 19:2837–2843.
Goeze A, Schluns K, Wolf G, et al.: Chromosomal imbalances of primary and metastatic lung adenocarcinomas. J Pathol 2002, 196:8–16.
Nassar A, Radhakrishnan A, Cabrero IA, et al.: Intratumoral heterogeneity of immunohistochemical marker expression in breast carcinoma: a tissue microarray-based study. Appl Immunohistochem Mol Morphol 2010, 18:441–443.
• Barry WT, Kernagis DN, Dressman HK, et al.: Intratumor heterogeneity and precision of microarray-based predictors of breast cancer biology and clinical outcome. J Clin Oncol 2010, 28:2198–2206. This paper discusses intratumoral heterogeneity and microarray-based predictions of tumor behavior or clinical outcome.
Weigelt B, Hu Z, He X, et al.: Molecular portraits and 70-gene prognosis signature are preserved throughout the metastatic process of breast cancer. Cancer Res 2005, 65:9155–9158.
Nahta R, Shabaya S, Ozbay T, Rowe DL: Personalizing HER2-targeted therapy in metastatic breast cancer beyond HER2 status: what we have learned from clinical specimens. Curr Pharmacogenomics Person Med 2009, 7:263–274.
Di Cosimo S, Baselga J: Management of breast cancer with targeted agents: importance of heterogeneity [corrected]. Nat Rev Clin Oncol 2010, 7:139–147.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khasraw, M., Brogi, E. & Seidman, A.D. The Need to Examine Metastatic Tissue at the Time of Progression of Breast Cancer: Is Re-biopsy a Necessity or a Luxury?. Curr Oncol Rep 13, 17–25 (2011). https://doi.org/10.1007/s11912-010-0137-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-010-0137-9