Abstract
Purpose
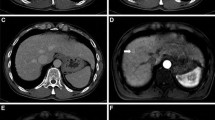
We prospectively compared gadoliniumenhanced magnetic resonance imaging (dynamic MRI), superparamagnetic iron oxide (SPIO) (ferucarbotran) MRI and multidetector-row computed tomography (MDCT) and the combination of dynamic MRI plus MDCT vs. dynamic MRI plus SPIO-MRI (double-contrast MRI: DC-MRI) forthe detection of small (≤3 cm) hepatocellular carcinomas (HCCs).
Materials and Methods
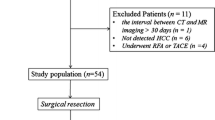
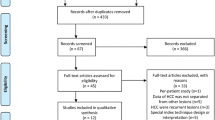
Sixty-three patients with liver cirrhosis and suspicious nodules detected during ultrasound (US) surveillance underwent DC-MRI in the same imaging session and MDCT within 15 days. The final diagnosis was established at pathology on the explanted liver (n=10), resection (n=6) and biopsy (n=38) specimens or at 2-years’ follow-up (n=9).
Results
One hundred and twenty-three nodules were detected: 87 were confirmed HCCs in 54 patients. The accuracy of SPIO-MRI and dynamic MRI were similar, both being superior to MDCT. Dynamic MRI demonstrated the highest sensitivity (83.9%; p<0.001). especially for lesions <1 cm (90.6%) - coupled with a lower specificity (36.1%) than SPIO-MRI, particularly in subcentimeter lesions (28.6%). SPIO-MRI demonstrated the highest sensitivity for nodules >1 cm and the highest specificity (83.3%) superior to dynamic MRI (p<0.0001). In the per-lesion analysis, SPIO-MRI demonstrated a positive predictive value higher than dynamic MRI (p=0.0059) and than both the combinations dynamic MRI/MDCT and DC-MRI (p=0.0021 and p=0.0087, respectively). DC-MRI showed the highest sensitivity (97.7%) and accuracy (78.9%), detecting hypovascular and atypical HCCs >1 cm. Furthermore its per-patient negative predictive value was the highest (100%), and significantly higher than all the other methods.
Conclusions
DC-MRI is the most sensitive and accurate method and can be confidently used as a single-step procedure for the detection of small HCCs, with the exception of lesions <1 cm.
Riassunto
Obiettivo
Abbiamo condotto uno studio prospettico per la diagnosi del piccolo epatocarcinoma (HCC) (<3 cm) comparando la risonanza magnetica (RM) dinamica dopo iniezione di Gd-DTPA (RM-dinamica), RM dopo mezzo di contrasto superparamagnetico-Resovist (RM-SPIO) e tomografia computerizzata (TC) spirale multidetettore (TCMD) e le combinazioni di RM-dinamica/TCMD e di RM-dinamica/RM-SPIO (eseguendo una RM a doppio contrasto, RM-DC).
Materiali e metodi
Sessantatre pazienti cirrotici con noduli sospetti individuati durante la sorveglianza ecografica (US) hanno eseguito una RM-dinamica ed una RM-SPIO nella stessa seduta ed una TCMD entro 15 giorni. La diagnosi definitiva viene fornita dal reperto anatomo-patologico — su fegato espiantato (n=10), resezione (n=6) e biopsia (n=38) — o da follow-up di 2 anni (n=9).
Risultati
Sono stati individuati 123 noduli, di cui 87 HCC in 54 pazienti. RM-SPIO e RM-dinamica hanno mostrato accuratezza simile, superiore alla TCMD. La RMdinamica ha dimostrato la maggiore sensibilità (83,9%; p<0,001), specie per lesioni<1 cm (90,6%), associata a minore specificità (36,1%) rispetto alla RM-SPIO, specie in lesioni subcentimetriche (28,6%). La RM-SPIO ha dimostrato la massima sensibilità per i noduli>1 cm e una specificità (83,3%) più elevata della RM-dinamica (p<0,0001). Nell’analisi per lesione la RM-SPIO ha dimostrato un valore predittivo positivo superiore alla RM-dinamica (p=0,0059) ed alla combinazione RMdinamica/TCMD e RM-DC (rispettivamente p=0,0021 e p=0,0087). La RM-DC ha dimostrato la più alta sensibilità (97,7%) ed accuratezza (78,9%), individuando gli HCC>1 cm ipovascolari ed atipici; inoltre il suo valore predittivo negativo per paziente è massimale (100%) e significativamente superiore a tutte le altre metodiche.
Conclusioni
La RM-DC si è rivelata la metodica più sensibile e accurata e può essere adottata con sicurezza come singola metodica per l’individuazione dei piccoli HCC, pur presentando alcuni limiti nelle lesioni<1 cm.
Similar content being viewed by others
References/Bibliografia
Bruix J, Sherman M, Llovet JM et al (2001) EASL Panel of Experts on HCC. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol 35:421–430
Bruix J, Sherman M (2005) Practice Guidelines Committee, American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma. Hepatology 42:1208–1236
Willatt JM, Hussain HK, Adsumilly S et al (2008) MR imaging carcinoma in the cirrhotic liver: challenges and controversies. Radiology 247:311–328
Colli A, Fraquelli M, Casazza G et al (2006) Accuracy of ultrasonography, spiral CT, magnetic resonance, and alpha-fetoprotein in diagnosing hepatocellular carcinoma: a systematic review. Am J Gastroenterol 101:513–523
Forner A, Vilana R, Ayuso C et al (2008) Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma. Hepatology 47:97–104
Hecht EM, Holland AE, Israel GM et al (2006) Hepatocellular carcinoma in the cirrhotic liver: gadolinium-enhanced 3D T1-weighted MR imaging as a stand-alone sequence for diagnosis. Radiology 239:438–447
Rode A, Bancel B, Douek P et al (2001) Small nodule detection in cirrhotic livers: evaluation with US, spiral CT, and MRI and correlation with pathologic examination of explanted liver. J Comput Assist Tomogr 25:327–336
Burrel M, Llovet JM, Ayuso C et al (2003) Barcelona Clinic Liver Cancer Group. MRI angiography is superior to helical CT for detection of HCC prior to liver transplantation: an explant correlation. Hepatology 38:1034–1042
Lencioni R, Della Pina C, Bruix J et al (2005) Clinical management of hepatic malignancies: ferucarbotran-enhanced magnetic resonance imaging versus contrast-enhanced spiral computed tomography. Dig Dis Sci 50:533–537
Bluemke DA, Paulson EK, Choti MA et al (2000) Detection of hepatic lesions in candidates for surgery: comparison of ferumoxides-enhanced MR imaging and dual-phase helical CT. AJR Am J Roentgenol 175:1653–1658
Kang BK, Lim JH, Kim SH et al (2003) Preoperative depiction of hepatocellular carcinoma: ferumoxides-enhanced MR imaging versus triple-phase helical CT. Radiology 226:79–85
Kim SH, Choi D, Kim SH et al (2005) Ferucarbotran-enhanced MRI versus triple-phase MDCT for the preoperative detection of hepatocellular carcinoma. AJR Am J Roentgenol 184:1069–1076
Kim YK, Kwak HS, Kim CS et al (2006) Hepatocellular carcinoma in patients with chronic liver disease: comparison of SPIO enhanced MR imaging and 16-detector row CT. Radiology 238: 531–541
Vogl TJ, Schwarz W, Blume S et al (2003) Preoperative evaluation of malignant liver tumors: comparison of unenhanced and SPIO (Resovist)-enhanced MR imaging with biphasic CTAP and intraoperative US. Eur Radiol 13: 262–272
Choi D, Kim SH, Lim JH et al (2001) Preoperative detection of hepatocellular carcinoma: ferumoxides-enhanced MR imaging versus combined CT during arterial portography and CT hepatic arteriography. AJR Am J Roentgenol 176: 475–482
Kim MJ, Kim JH, Chung JJ et al (2003) Focal hepatic lesions: detection and characterization with combination gadolinium- and superparamagnetic iron oxide-enhanced MR imaging. Radiology 228: 719–726
Ward J, Guthrie JA, Scott DJ et al (2000) Hepatocellular carcinoma in the cirrhotic liver: double-contrast MR imaging for diagnosis. Radiology 216: 154–162
Bhartia B, Ward J, Guthrie JA et al (2003) Hepatocellular carcinoma in cirrhotic livers: double-contrast thinsection MR imaging with pathologic correlation of explanted tissue. AJR Am J Roentgenol 180: 577–584
Hanna RF, Kased N, Kwan SW et al (2008) Double-contrast MRI for accurate staging of hepatocellular carcinoma in patients with cirrhosis. AJR Am J Roentgenol 190: 47–57
Hanna RF, Aguirre DA, Kased N et al (2008) Cirrhosis associated Hepatocellular Nodules: Correlation of Histopathologic and MR Imaging Features. Radiographics 28: 747–769
de Ledinghen V, Laharie D, Lecesne R et al (2002) Detection of nodules in liver cirrhosis: spiral computed tomography or magnetic resonance imaging? A prospective study of 88 nodules in 34 patients. Eur J Gastroenterol Hepatol 14: 159–165
Nakamura H, Ito N, Kotake F et al (2000) Tumor-detecting capacity and clinical usefulness of SPIO-MRI in patients with hepatocellular carcinoma. J Gastroenterol 35: 849–855
Kwak HS, Lee JM, Kim YK et al (2005) Detection of hepatocellular carcinoma: comparison of ferumoxidesenhanced and gadolinium-enhanced dynamic three-dimensional volume interpolated breath-hold MR imaging. Eur Radiol 15: 140–147
Pauleit D, Textor J, Bachmann R et al (2002) Hepatocellular carcinoma: detection with gadolinium- and ferumoxides-enhanced MR imaging of the liver. Radiology 222: 73–80
Tang Y, Yamashita Y, Arakawa A et al (1999). Detection of hepatocellular carcinoma arising in cirrhotic livers: comparison of gadolinium- and ferumoxides-enhanced MR imaging. AJR Am J Roentgenol 172: 1547–1554
Tanimoto A, Kuribayashi S (2006) Application of superparamagnetic iron oxide to imaging of hepatocellular carcinoma. Eur J Radiol 58: 200–216
Simon G, Link TM, Wortler K et al (2005) Detection of hepatocellular carcinoma: comparison of Gd-DTPAand ferumoxides-enhanced MR imaging. Eur Radiol 15: 895–903
Jeong YY, Mitchell DG, Kamashima T (2002) Small (< 20 mm) enhancing hepatic nodules seen on arterial phase MR imaging of the cirrhotic liver: clinical implications. AJR Am J Roentgenol 178: 1327–1334
Shimizu A, Ito K, Koike S et al (2003). Cirrhosis or chronic hepatitis: evaluation of small (< 2 cm) earlyenhancing hepatic lesions with serial contrast-enhanced dynamic MR imaging. Radiology 226: 550–555
Holland AE, Hecht EM, Hahn WY et al (2005) Importance of small (< or =20- mm) enhancing lesions with whole explanted liver seen only during the hepatic arterial phase at MR imaging of the cirrhotic liver: evaluation and comparison with whole esplanted liver. Radiology 237: 938–944
Oudkerk M, van den Heuvel AG, Wielopolski PA et al (1997) Hepatic lesions: detection with ferumoxideenhanced T1-weighted MR imaging. Radiology 203: 449–456
Bolondi L, Gaiani S, Celli N et al (2005) Characterization of small nodules in cirrhosis by assessment of vascularity: the problem of hypovascular hepatocellular carcinoma. Hepatology 42: 27–34
Bartolozzi C, Crocetti L, Lencioni R et al (2007) Biliary and reticuloendothelial impairment in hepatocarcinogenesis: the diagnostic role of tissue-specific MR contrast media. Eur Radiol 17: 2519–2530
Kojiro M (2004) Focus on dysplastic nodules and early hepatocellular carcinoma: an Eastern point of view. Liver Transpl 10: S3–S8
Imai Y, Murakami T, Yoshida S et al (2000) Superparamagnetic iron oxideenhanced magnetic resonance images of hepatocellular carcinoma: correlation with histological grading. Hepatology 32: 205–212
Lim JH, Choi D, Cho SK et al (2001) Conspicuity of hepatocellular nodular lesions in cirrhotic livers at ferumoxides-enhanced MR imaging: importance of Kupffer cell number. Radiology 220: 669–676
Qayyum, A, Thoeni RF, Coakley FV et al (2006) Detection of hepatocellular carcinoma by ferumoxides-enhanced MR imaging in cirrhosis: incremental value of dynamic gadoliniumenhancement. J Magn Reson Imaging 23: 17–22
Mori K, Scheidler J, Helmberger T et al (2002) Detection of malignant hepatic lesions before orthotopic liver transplantation: accuracy of ferumoxides-enhanced MR imaging. AJR Am J Roentgenol 179: 1045–1051
Krinsky GA, Lee VS, Thiese ND et al (2001) Hepatocellular carcinoma and dysplastic nodules in patients with cirrhosis: prospective diagnosis with MR imaging and explantation correlation. Radiology 219: 445–454
Krinsky GA, Lee VS, Theise ND et al (2002) Transplantation for hepatocellular carcinoma and cirrhosis: sensitivity of magnetic resonance imaging. Liver Transpl 8: 1156–1164
Tanaka M, Nakashima O, Wada Y et al (1996) Pathomorphological study of Kupffer cells in hepatocellular carcinoma and hyperplastic lesions in the liver. Hepatology 24: 807–812
Ransohoff DF, Feinstein AR (1978) Problems of spectum and bias in evaluating the efficacy of diagnostic tests. N Engl J Med 299: 926–930
Bossuyt PM, Reitsma JB, Bruns DE et al (2003) Standards for reporting of diagnostic accuracy the STARD statement for reporting studies of diagnostic accuracy explanation and elaboration. Ann Intern Med 138: W1–W12
Tanimoto A, Yuasa Y, Shinmoto H et al (2002) Superparamagnetic iron oxide mediated hepatic signal change in patients with and without cirrhosis: pulse sequence effects and Kupffer cell function. Radiology 222: 661–666
Macarini L, Marini S, Milillo P et al (2006) Double-contrast MRI (DC-MRI) in the study of the cirrhotic liver: utility of administering Gd-DTPA as a complement to examinations in which SPIO liver uptake and distribution alterations (SPIO-LUDA) are present and in the identification and characterisation of focal lesions. Radiol Med 111: 1087–1102
Ishiyama K, Hashimoto M, Izumi J et al (2008) Tumor-liver contrast and subjective tumor conspicuity of respiratory-triggered T2-weighted fast spin-echo sequence compared with T2*-weighted gradient recalled-echo sequence for ferucarbotran-enhanced magnetic resonance imaging of hepatic malignant tumors. J Magn Reson Imaging 27: 1322–1326
Lutz AM, Goepfert K, Willmann JK et al (2005) Hepatocellular carcinoma in cirrhosis: enhancement patterns at dynamic gadolinium and superparamagnetic-iron oxide-enhanced T1-weighted MR images. Radiology 237: 520–528
Marrero JA, Hussain HK, Nghiem HV et al (2005) Improving the prediction of hepatocellular carcinoma in cirrhotic patients with an arterially-enhancing liver mass. Liver Transpl 11: 281–289
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Golfieri, R., Marini, E., Bazzocchi, A. et al. Small (≤3 cm) hepatocellular carcinoma in cirrhosis: the role of double contrast agents in MR imaging vs. multidetector-row CT. Radiol med 114, 1239–1266 (2009). https://doi.org/10.1007/s11547-009-0439-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-009-0439-x
Keywords
- Liver
- Neoplasms
- Hepatocellular carcinoma
- Cirrhosis
- Contrast agents
- SPIO-Enhanced MRI
- Gd-DTPA-enhanced MRI
- Multiphasic helical multidetector row CT (MDCT)