Abstract
Purpose
Recent data have indicated that 68Ga-DOTA-NOC positron emission tomography/X-ray computed tomography (PET/CT) may yield improved images in a shorter acquisition protocol than 111In-DTPA-octreotide (OctreoScan®, OCT). Therefore, we performed a prospective comparison of 68Ga-DOTA-NOC and OCT for the detection of neuroendocrine tumors (NETs).
Methods
Nineteen patients (eight carcinoid, nine pancreatic NETs, and two NE carcinoma of unknown origin) with previous positive OCT scans underwent 68Ga-DOTA-NOC PET/CT and OCT single-photon emission computed tomography imaging for staging or follow-up. Findings were compared by region and verified with conventional imaging.
Results
All images of both modalities demonstrated focal uptake, often at multiple sites. 68Ga-DOTA-NOC images were clearer than OCT images, facilitating interpretation. Similar foci were identified with both modalities in 41 regions, with additional foci on 68Ga-DOTA-NOC in 21 and on OCT in 15 regions. CT, magnetic resonance imaging, or ultrasound confirmed the concordant findings in 31 of 41 regions and findings seen with 68Ga-DOTA-NOC only in 15 of 21 regions. Findings seen with OCT only were less clear and were only confirmed in 4 of 15 regions. 68Ga-DOTA-NOC had impact on staging in four patients and on management in three patients.
Conclusions
Although 68Ga-DOTA-NOC and OCT images were similar, in this study, 68Ga-DOTA-NOC demonstrated more true positive tumor foci and was better tolerated by patients. This direct comparison supports replacement of OCT with 68Ga-DOTA-NOC-PET/CT in the evaluation of NETs.
Similar content being viewed by others
Introduction
Neuroendocrine tumors (NETs) are considered a rare class of tumors; however, due to greater awareness and more accurate diagnostic modalities, their identification has increased substantially over the last decades [1]. Localization of primary tumors and detection of metastases are crucial for optimizing treatment strategies. Slow-growing NETs are best treated by complete surgical removal, but in the presence of metastases or non-resectable disease, unnecessary surgery should be spared. However, even with morphological imaging, such as X-ray computed tomography (CT) and/or magnetic resonance imaging (MRI), NETs are frequently difficult to localize due to small size, multiplicity, presence in hollow organs, and morphological changes caused by prior surgery [2], with detection rates of 22–45% for gastrinomas and mid-gut carcinoids [1].
Exploiting the unique biological characteristics of NETs, functional imaging techniques have therefore been introduced, mostly based on radioligands for agonist binding to somatostatin receptors (SSTR), which are over-expressed in many NETs [3]. One of the most widely used tracers, 111In-DTPA-Octreotide (OctreoScan®, OCT), has become the standard technique for localization, staging, and management of NETs, detecting metastatic disease with sensitivity of 67–100%, depending on tumor type and location [4]. OCT may reveal small tumor sites prior to identification on morphological imaging, but it is limited by the low spatial resolution of single-photon emission computed tomography (SPECT), poor uptake by some tumors, and prolonged acquisition time. In addition, imaging with 111In-labeled peptides is demanding for both the patient and hospital staff since it is usually performed over a 24-h period, extending occasionally even to 48 h to allow for adequate uptake in tumors and washout from normal tissues, and requires at least 2–4 h of technician and machine time.
In recent years, 68Ga-labeled somatostatin analogs have been developed for somatostatin receptor imaging of NETs with positron emission tomography (PET). Preclinical [5–7] and clinical studies have described the use of several analogs, including DOTA-Tyr3 octreotide (DOTA-TOC) [8–10], DOTA-Tyr3, Thr8 octreotide (DOTA-TATE) [11], and DOTA-1-Nal3-octreotide (DOTA-NOC) [12]. In addition to the advantages conveyed by the superior physical characteristics of PET (spatial resolution, sensitivity, and quantitation) as compared to SPECT or planar imaging, 68Ga-labeled ligands show a higher affinity for somatostatin receptor types 2 and 5 and more rapid blood clearance than the corresponding 111In-labeled tracers [6]. As a result, accurate images of NETs with a high density of somatostatin receptors can be obtained by PET as soon as 60–90 min after tracer injection, without a repeated scan on the following day. Furthermore, the radiation dose using these tracers is lower than that of OCT [13, 14].
While DOTA-TOC, DOTA-TATE, DOTA-NOC, and other tracers all show promise for imaging NETs, DOTA-NOC appears to have some advantages, including wider specificity for somatostatin receptor type 3 [7], and this was the tracer chosen for use in this study.
Clinical application of 68Ga-DOTA-NOC was first described in 2005 [12, 15]. Very high diagnostic sensitivity and specificity was documented, including the detection of very small lesions in lymph nodes and in the bone. Pettinato et al. [13] reported on the biodistribution of 68Ga-DOTA-NOC and described uptake in various NETs in nine patients. The utility of 68Ga-DOTA-NOC has also been demonstrated in 11 patients with bronchial carcinoid [16], in 13 patients with gastro-entero-pancreatic and lung NETs [17], in 14 cases of unusual NETs [18], and in 35 of 59 patients with unknown primary NE tumors [19]. In these studies, 68Ga-DOTA-NOC findings were compared with morphological imaging and/or 6-[18F]fluoro-L-DOPA PET [17], but no consistent direct comparison with the standard somatostatin receptor imaging procedure with OCT has been reported. In this prospective study, we performed 68Ga-DOTA-NOC PET/CT and OCT scintigraphy using SPECT and/or SPECT/CT in 19 patients with various NETs. Since our objective was to compare positive findings in the two imaging modalities, we selected patients with histologically confirmed diagnoses of NETs and a high density of receptors as documented by a previous OCT.
Patients and Methods
Patients
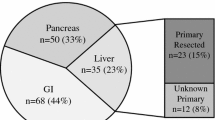
Nineteen patients (7 women and 12 men; age range 26–82 years, mean 60.3 ± 13.6) were enrolled for comparison of 68Ga-DOTA-NOC PET/CT and OCT in imaging NETs. Patients were referred for tumor staging, detection of somatostatin receptors prior to peptide receptor radionuclide therapy (PRRT), and for evaluation of response to therapy. The tumors included well-differentiated endocrine carcinoma and poorly differentiated endocrine carcinoma: carcinoid (n = 8), pancreatic NE tumor (n = 9), and NE carcinoma of unknown origin (n = 2). Patient information, together with pathologic diagnosis based on World Health Organization criteria, is shown in Table 1.
All patients had a definitive histological diagnosis of NET at surgery (n = 10) or biopsy (n = 9) and previous positive findings on OCT. Patients who were below 18 years of age, pregnant or nursing, or unwilling or unable to comply with the protocol were excluded from the study. All patients gave written, informed consent for the study, which was approved by the Institutional Review Board.
Image Acquisition
Treatment with the short-acting octreotide SC or the long-acting somatostatin analog (octreotide-LAR or lanreotide autogel) was withdrawn 3 days or 6 weeks, respectively, prior to scans.
All patients underwent 68Ga-DOTA-NOC PET/CT and OCT imaging within 10–65 days of each other (median 24 days).
68Ga-DOTA-NOC was acquired first in six patients, and OCT was acquired first in 13 patients. To avoid the possibility of blocking receptors by unlabeled DOTA-NOC or octreotide, at least 10 days were allowed to elapse between 68Ga-DOTA-NOC PET/CT and OCT SPECT, and when the OCT image was acquired first, at least 18 days were allowed to elapse before the 68Ga-DOTA-NOC PET/CT to allow for decay of 111In (half-life 2.81 days). In addition, patients underwent conventional localization studies, depending on the site of disease and clinical condition, as part of the routine staging. These included CT with intravenous contrast media, MRI, ultrasound (US), endoscopic US, and/or 2-deoxy-2-[18F]fluoro-d-glucose PET/CT.
68Ga-DOTA-NOC-PET/CT
PET/CT scans were acquired on a GE Discovery ST PET/CT scanner (GE Medical System, Waukesha, WI, USA). Synthesis of 68Ga-DOTA-NOC is described in the Appendix. 68Ga-DOTA-NOC 83.2–184.3 MBq (mean 144.7 ± 23.8; median 146.5 MBq) was administered intravenously, with scan beginning 56–96 min (mean 77 ± 13 min) after tracer injection. The PET/CT protocol consisted of a CT scan acquired with oral contrast, to provide anatomic localization as well as attenuation correction for the PET data, and was followed by a PET scan. PET images were acquired for 3–4 min per 15-cm axial field of view in a 3D acquisition. Both CT and PET images were acquired from vertex to mid-thigh. PET images were corrected for tissue attenuation using the CT data and reconstructed using iterative reconstruction (3D FORE-Iterative).
PET images were evaluated qualitatively and semi-quantitatively using standardized uptake values (SUVs), defined as [20]:
111In-DTPA-Octreotide Scintigraphy
Thirteen patients underwent OCT imaging at our institution and the remaining six at other hospitals. The scan protocol at our institution is described here. Protocols at the other hospitals were comparable; all included both planar and SPECT/CT scans. OCT imaging was performed after intravenous administration of 222 MBq of OctreoScan® (Mallinckrodt Medical, Petten, Holland). Images were acquired using a dual-head, large field-of-view gamma camera equipped with a medium-energy collimator. Planar WB scans from vertex to mid-thigh were acquired at 4 h when possible and in all patients at 24 h after tracer injection. Seven patients also underwent SPECT of the abdomen at 4 h, with or without co-registered CT. SPECT of the abdomen, pelvis, chest, neck, and head as required, with or without CT, was acquired in all patients at 24 h after tracer injection. Images were reconstructed iteratively using the ordered subsets expectation maximization algorithm. The transmission data obtained during SPECT/CT were used for anatomic localization of the scintigraphic findings and for the reevaluation or guidance of high-resolution CT/MRI.
For assessment of tracer uptake on OCT imaging, intensity of tumor foci was compared with intensity of the physiological liver uptake on the planar WB scan. Intensity on attenuation-corrected SPECT/CT was also taken into account.
Analysis
68Ga-DOTA-NOC PET/CT and OCT SPECT images were viewed and interpreted separately by two nuclear medicine physicians (YK, RR), each blinded to the other set of images and to other imaging modalities. Any area with intensity greater than the background not attributable to physiological activity was considered indicative of tumor tissue. Findings of 68Ga-DOTA-NOC and OCT imaging were then compared; since foci of enhanced tracer uptake were often numerous, multifocal, and sometimes confluent, the comparison was carried out region-by-region rather than enumerating each focus.
Findings in each region were classified as concordant if the same foci were seen in that region on both modalities or discordant if foci were seen only on one modality. In case of discrepancy, images were reviewed and compared with CT, MRI, or US, acquired within the last 3 months, and additional studies, including diagnostic CT, MRI, US, and/or endoscopic US were performed, as indicated, to validate the findings. Tissue confirmation of every lesion was not feasible and not justifiable ethically because of tumor burden in many patients. The contribution of 68Ga-DOTA-NOC PET was determined by comparing the scan results with the final, composite clinical evaluation obtained after all relevant conventional imaging studies, as detailed above, were completed and evaluated. The treating physician was asked to evaluate how, if at all, the 68Ga-DOTA-NOC PET/CT results affected the therapeutic decisions.
Results
Clinical details of the 19 patients are reported in Table 1. Positive findings of tracer uptake in at least one lesion were seen in all patients both on 68Ga-DOTA-NOC and OCT images, as expected since only subjects with previous positive OCT SPECT imaging were included. Findings on 68Ga-DOTA-NOC PET/CT were overall more numerous and more distinct, with much better tumor to background contrast and less image noise. Findings of both imaging modalities are listed for individual patients and regions, together with comparison with morphological data in Table 2, and summarized by regions for all patients in Table 3.
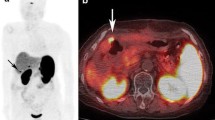
Similar pathological tumor sites were visible on both 68Ga-DOTA-NOC and OCT in a total of 41 regions in all 19 patients. Additional foci of pathological uptake were seen in 21 regions on 68Ga-DOTA-NOC only and in 15 regions on OCT only. Foci of tracer uptake were observed in the liver, pancreas, bone, lymph nodes, digestive tract, as well as a few additional findings in other parts of the body including soft tissue, brain, thyroid, and tonsils. Differences between the two imaging modalities did not appear to be more prevalent in specific regions (see Table 3). 68Ga-DOTA-NOC uptake in tumor foci was often very intense, and this is reflected in the maximum SUV which ranged from 2 to 165 (see Table 2). As seen from Tables 2 and 3, many findings were comparable in both imaging modalities, though even in those regions where identical tumor foci were described, foci of enhanced tracer uptake were generally clearer on the 68Ga-DOTA-NOC images, and with the assistance of co-registered CT for all scans, anatomical localization of findings was easier and more precise. Examples of images showing comparable findings in both modalities, but illustrating greater clarity and contrast with 68Ga-DOTA-NOC, are shown in Figs. 1 and 2.
Patient 19: a PET 68Ga-DOTA-NOC maximum intensity projection showing two distinct foci of enhanced activity in the liver (thin arrow) and in two retroperitoneal nodes (thick arrow). b Whole body planar OCT image (anterior view) showing the same two foci in the liver (thin arrow). The retroperitoneal nodes are not visualized here; these nodes were also not visible on the posterior view (not shown).
Patient 19: a Transaxial PET 68Ga-DOTA-NOC image showing the two foci in the liver (thin arrow) seen in Fig. 1. b Corresponding CT image. c Transaxial SPECT OCT image showing the same two foci in the liver (thin arrow). d Corresponding CT image. Note the lack of complete correspondence between the slices on the two modalities due primarily to difference in patient position (arms up for the PET, arms down for the SPECT); difference in CT images is also due to respiration during prolonged CT acquisition on SPECT/CT.
An example of tumor foci seen only on 68Ga-DOTA-NOC, with no corresponding foci on OCT, is shown in Fig. 3 where intense uptake is clearly seen in a pre-aortic lymph node on 68Ga-DOTA-NOC, while no corresponding abnormality is visible on OCT. Additional findings on 68Ga-DOTA-NOC included a site of primary tumor in the tail of the pancreas in the case of a patient with MEN1; this tumor, shown in Fig. 4, was not identified on OCT. In contrast, Fig. 5 shows an example of findings on OCT that were not seen on 68Ga-DOTA-NOC; however, apart from this example and one other, all the remaining 13 findings seen only on OCT were faint and described as suspicious areas rather than well-defined tumor foci, such as in Fig. 5.
Patient 19: a Transaxial PET 68Ga-DOTA-NOC image showing one of the two retroperitoneal nodes (thin arrow) seen in Fig. 1. b Corresponding CT image. c Transaxial SPECT OCT image, like the planar image, fails to demonstrate this node. d Corresponding CT image.
Verification from anatomical imaging (CT, MRI, or US) was found for 31 of the 41 (76%) regions with concordant 68Ga-DOTA-NOC and OCT findings. CT, MRI, or US verification was also found for 15 of 21 (71%) regions seen on 68Ga-DOTA-NOC only, suggesting that most if not all of these findings were indeed true positive findings. On the other hand, confirmation was only available for 4 of 15 (27%) regions, with findings seen only on OCT, most of which were faint and poorly delineated and thus could not be clearly and unambiguously identified as tumor foci.
The additional foci of enhanced 68Ga-DOTA-NOC uptake had implications for disease staging in 4 of 19 patients. There were also implications for patient management in three patients, resulting in the referral of two patients for PRRT and more intensive follow-up in the third patient.
Discussion
In this study, we compared imaging with 68Ga-DOTA-NOC PET/CT and OCT, including both WB planar imaging and SPECT/CT of parts of the body, for localization of primary and metastatic NE tumors in a series of 19 patients. Our results show that 68Ga-DOTA-NOC, for the most part, detected the same NE tumor sites as OCT, but demonstrated their presence and location much more precisely. 68Ga-DOTA-NOC suggested additional NE tumor sites not seen on OCT in 21 regions of 14 patients, with verification in 15 of the 21 regions. Though there were also few tumor foci seen only on OCT, verification was available in only 4 of 15 foci. A similar trend was documented for PET imaging with 68Ga-DOTA-TOC. Buchmann et al. [8] compared 68Ga-DOTA-TOC and OCT in 27 patients with NETs and reported that in 18 of 31 (58%) discrepant regions that could be verified, 68Ga-DOTA-TOC was correct and OCT provided false negatives. 68Ga-DOTA-TOC also showed higher detection rates when compared with 111In111-DOTA-TOC and with 99mTc-HYNIC-TOC in the study of Gabriel et al. [9].
Our series included patients with carcinoid, pancreatic tumor, and metastatic NE tumor with unknown primary. Differences in findings between the two imaging modalities appeared throughout and did not depend on the type of disease. Likewise, tumor foci were seen throughout the body in the liver, pancreas, bone, lymph nodes, digestive tract, and a few other locations, and in all organs involved, there were findings that were concordant as well as some that were discordant between the PET and SPECT imaging modalities. This is in contrast to the findings with 68Ga-DOTA-TOC in the study of Buchmann et al. [8] who found discrepancies between 68Ga-DOTA-TOC and OCT in the lung and skeletal system, but not in the liver and brain. However, only one patient in our small series had brain involvement, and none had lung manifestations.
Ideally, the time interval between the two scans should have been as short as possible to preclude the possibility of disease progression during this interval. In fact, the median time interval was 24 days, maximum 64 days. This is unlikely to be associated with major progression in patients with well-differentiated NE carcinoma, but it is a potential cause of discordance in patients with higher-grade tumors. Only one among our patients was diagnosed with poorly differentiated NE carcinoma, and the time interval between her two scans was 33 days. Thus, time interval between 68Ga-DOTA-NOC PET and OCT imaging is unlikely to have contributed to the observed discrepancies.
Tracer activity concentration in tumor foci on 68Ga-DOTA-NOC was often very high, with maximum SUV ranging up to 165. Such high values of SUV resulted from intense uptake in the tumors, presumably due to the high density of somatostatin receptors combined with very low uptake in most of the remainder of the body. The possibility of performing exact quantitation of tracer uptake either for PRRT and/or for monitoring the effects of therapy with serial scans constitutes an additional important advantage for PET tracers. Future work will be required to investigate the role of 68Ga-DOTA-NOC imaging in the selection of patients for targeted radionuclide treatment and for the prediction of outcome. However, DOTA-NOC is currently not used for PRRT, in part because the uptake of 177Lu-DOTA-NOC was found to be higher in normal tissues and lower in tumor lesions, with lower mean absorbed tumor dose compared with 177Lu-DOTA-Tyr3-octreotate [21]. Furthermore, since the radiometal influences the pharmacological properties of the radiopeptides, distribution of the corresponding molecule labeled with 90Y or 177Lu for therapy purposes cannot necessarily be simply predicted [6].
Precise comparison between 68Ga-DOTA-NOC and OCT was difficult, if not impossible, because of essential differences between the images available for comparison. 68Ga-DOTA-NOC images were all tomographic images, acquired with higher spatial resolution and sensitivity, and with co-registered CT, while OCT images were all acquired with lower spatial resolution and comprised for the most part of SPECT with co-registered CT (in some cases of limited quality) with supplementary planar images. In addition, the much longer duration of imaging with planar or SPECT imaging increases the possibility of blurring due to patient motion. As a result of the inferior quality of the OCT images, it was not always possible to distinguish tumor foci from neighboring structures or from adjacent foci, and in some parts of the body, it was not possible to be certain in which structure a tumor focus was located, as in the case of a rib lesion adjacent to the apex of the lung in patient 4. Furthermore, the higher noise in the OCT images caused more difficulty in deciding confidently whether to interpret lower intensity foci as tumors or simply as image noise.
Further discrepancies between 68Ga-DOTA-NOC and OCT may result from differences in the use of the metal 68Ga rather than 111In and the chelate group DOTA rather than DTPA. These differences in the tracer molecules contribute to the broader somatostatin receptor subtype profile of 68Ga-DOTA-NOC, with higher affinity and internalization for SSTR2 and SSTR5 as well as affinity for SSTR3, with improved pharmacokinetics, permitting imaging soon after injection, and improved target to background contrast. This could also explain uptake in additional tumor foci seen only on 68Ga-DOTA-NOC and better visualization. There were also some apparently false negative findings on 68Ga-DOTA-NOC such as failure to visualize a pathological focus in the liver seen on OCT and on CT in the case of patient 12. 68Ga-DOTA-NOC activity was no higher in this pathological focus than in the surrounding liver tissue, although differences in somatostatin receptors between tumor and liver background were reflected in the visibility of the tumor on OCT 30 days previously. Possibly the different kinetics of 68Ga-DOTA-NOC uptake in the tumor versus normal liver tissue may be such that the tumor might have been visible with later 68Ga-DOTA-NOC acquisition. Investigation of tracer kinetics with a view to optimizing scan timing remains an issue for future work. While we did see 68Ga-DOTA-NOC uptake in normal tissues with somatostatin receptors, including pituitary, adrenals, and spleen, as described by others [13], this did not interfere with the identification of pathological foci of enhanced tracer activity. We saw no cases of known inflammation associated with increased tracer accumulation, though this has been described by Fanti el al. [18] as a possible cause for false positive findings on 68Ga-DOTA-NOC.
Analysis of the observed discrepancies between 68Ga-DOTA-NOC images and OCT requires independent validation of the findings. Meticulous validation of every tumor focus is impossible in many cases of NET not only because patients will only undergo subsequent surgery or biopsy when justified by their clinical situation but also because of the sheer multitude of tumor foci often seen. Biopsy of each focus would be impractical as well as ethically unjustifiable. As a result, there is generally no ultimate gold standard, and for the most part, even when available, morphological imaging findings and clinical course provide support rather than absolute confirmation of 68Ga-DOTA-NOC and OCT findings. The shortcomings of validation by morphological imaging have been noted by Buchmann et al. [8] who stated that verification of 68Ga-DOTA-TOC PET by CT and MRI is limited by the low sensitivity of these modalities for small metastases of NETs. In addition, therapy-induced or tumor progression-related changes in function, imaged by 68Ga-DOTA-NOC and OCT, may precede changes in structure seen on morphological imaging. While the resulting possibility of early detection of disease progression on receptor imaging is one of the strongest aspects of functional imaging, it is also a potential cause for true discrepancy between functional and morphological imaging, generating caution in dismissing foci of enhanced uptake seen on functional but not on morphological imaging as false positive findings. Examples of such findings seen in our study include foci in the pancreas in patients 15 and 18 not visible on MRI and also in the pancreas in patient 7 with negative endoscopic US. Likewise, retroperitoneal nodes seen in patient 6 were not seen on CT.
In clinical practice, acquisition of 68Ga-DOTA-NOC imaging is quicker and simpler than OCT. 68Ga is a generator nuclide that is easily accessible, and to further facilitate easy and consistent access to 68Ga-DOTA-NOC, we developed a method for synthesis using a modification to the readily available GE Tracerlab fluorination module that enabled us to routinely produce 68Ga-DOTA-NOC in a consistent manner (see Appendix). Furthermore, while 68Ga-DOTA-NOC is not yet available commercially, this and other 68Ga-labeled tracers have now been used widely in research studies.
The acquisition protocol of 68Ga-DOTA-NOC PET/CT is much more favorable that those for OCT SPECT for both patients and personnel, involving <3 h from tracer injection to the end of imaging and including only about 30 min lying still on the scanner bed. In contrast, the OCT protocol may require patients to return for lengthy imaging sessions at 4, 24, and, occasionally, at 48 h after tracer injection for differentiation of pathologic bowel involvement from physiological activity. Furthermore, in clinical practice, while a CT scan is performed quickly and routinely as a part of the PET/CT acquisition protocol, SPECT is often performed without CT, and many centers do not have SPECT/CT and/or prefer not to perform CT with SPECT to reduce radiation dose and/or acquisition time, bearing in mind the need for repeated acquisitions. In addition, it should be noted that radiation exposure to the patients is lower with 68Ga-DOTA-NOC (effective dose equivalent 0.017 mSv/MBq) than with OCT (0.077 mSv/MBq) [13, 14]. Furthermore, reduced acquisition times will lead to more efficient use of resources.
This study has certain limitations due to its design and related clinical considerations. Our goal was to perform a direct comparison between two functional imaging modalities and compare these to validated clinical status and morphological imaging. Because of the strict inclusion criteria and prolonged imaging protocol, only a small number of patients were studied. In addition, since complete histological verification of all lesions was both ethically and practically not feasible, a composite endpoint based on morphologic studies, limited histological verification and clinical follow-up was used. It is possible that some lesions considered true positives were in fact not tumor-related, although given the evidence of the accuracy of 68Ga-DOTA-NOC findings in NETs that has been reported in the literature [12, 15–19], it is unlikely that this problem significantly affected the results. On the other hand, it is likely that some, if not most of the 13 lesions with weak uptake on OCT and no uptake on 68Ga-DOTA-NOC or morphologic validation, might in fact be false positives.
Conclusion
In this small prospective study, 68Ga-DOTA-NOC was comparable, if not superior, to OCT in the detection of NE tumor sites. Moreover, 68Ga-DOTA-NOC images were much clearer than OCT images and therefore easier to interpret. In addition, 68Ga-DOTA-NOC PET/CT has many practical advantages: shorter imaging procedure, tolerated better by the patient, requires fewer personnel and scanner time, and incurs lower radiation dose to the patient. 68Ga-DOTA-NOC can be synthesized in large tracer quantities for routine clinical use using 68Ga from a generator without need for an on-site cyclotron. For all these reasons, 68Ga-DOTA-NOC PET/CT is preferable to OCT SPECT imaging for staging and long-term follow-up of NET patients.
References
Modlin IM, Oberg K, Chung DC, Jensen RT, de Herder WW, Thakker RV, Caplin M, Delle Fave G, Kaltsas GA, Krenning EP, Moss SF, Nilsson O, Rindi G, Salazar R, Ruszniewski P, Sundin A (2008) Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol 9:61–72
Oberg K, Eriksson B (2005) Nuclear medicine in the detection, staging and treatment of gastrointestinal carcinoid tumours. Best Pract Res Clin Endocrinol Metab 19:265–276
Kwekkeboom DJ, Krenning EP, de Jong M (2000) Peptide receptor imaging and therapy. J Nucl Med 41:1704–1713
Kaltsas G, Rockall A, Papadogias D, Reznek R, Grossman AB (2004) Recent advances in radiological and radionuclide imaging and therapy of neuroendocrine tumours. Eur J Endocrinol 151:15–27
Froidevaux S, Eberle AN, Christe M, Sumanovski L, Heppeler A, Schmitt JS, Eisenwiener K, Beglinger C, Mäcke HR (2002) Neuroendocrine tumor targeting: study of novel gallium-labeled somatostatin radiopeptides in a rat pancreatic tumor model. Int J Cancer 98:930–937
Antunes P, Ginj M, Zhang H, Waser B, Baum RP, Reubi JC, Maecke H (2007) Are radiogallium-labelled DOTA-conjugated somatostatin analogues superior to those labelled with other radiometals? Eur J Nucl Med Mol Imaging 34:982–993
Wild D, Schmitt JS, Ginj M, Mäcke HR, Bernard BF, Krenning E, De Jong M, Wenger S, Reubi JC (2003) DOTA-NOC, a high-affinity ligand of somatostatin receptor subtypes 2, 3 and 5 for labelling with various radiometals. Eur J Nucl Med Mol Imaging 30:1338–1347
Buchmann I, Henze M, Engelbrecht S, Eisenhut M, Runz A, Schäfer M, Schilling T, Haufe S, Herrmann T, Haberkorn U (2007) Comparison of 68Ga-DOTATOC and 111In-DTPAOC (Octreoscan) SPECT in patients with neuroendocrine tumours. Eur J Nucl Med Mol Imaging 34:1617–1626
Gabriel M, Decristoforo C, Kendler D, Dobrozemsky G, Heute D, Uprimny C, Kovacs P, Von Guggenberg E, Bale R, Virgolini IJ (2007) 68Ga-DOTA-Tyr3-Octreotide PET in neuroendocrine tumors: comparison with somatostatin receptor scintigraphy and CT. J Nucl Med 48:508–518
Gabriel M, Oberauer A, Dobrozemsky G, Decristoforo C, Putzer D, Kendler D, Uprimny C, Kovacs P, Bale R, Virgolini IJ (2009) 68Ga-DOTA-Tyr3-Octreotide PET for assessing response to somatostatin-receptor-mediated radionuclide therapy. J Nucl Med 50:1427–1434
Win Z, Al-Nahhas A, Towey D, Todd JF, Rubello D, Lewington V, Gishen P (2007) 68Ga-DOTATATE PET in neuroectodermal tumours: first experience. Nucl Med Commun 28:359–363
Wild D, Mäcke HR, Waser B, Reubi JC, Ginj M, Rasch H, Müller-Brand J, Hofmann M (2005) 68Ga-DOTANOC: a first compound for PET imaging with high affinity for somatostatin receptor subtypes 2 and 5. Eur J Nucl Med Mol Imaging 32:724
Pettinato C, Sarnelli A, Di Donna M, Civollani S, Nanni C, Montini G, Di Pierro D, Ferrari M, Marengo M, Bergamini C (2008) 68Ga-DOTANOC: biodistribution and dosimetry in patients affected by neuroendocrine tumors. Eur J Nucl Med Mol Imaging 35:72–79
Kwekkeboom DJ, Kooij PP, Bakker WH, Macke HR, Krenning EP (1999) Comparison of 111In-DOTA-Tyr3-octreotide and 111In-DTPA-octreotide in the same patients: biodistribution, kinetics, organ and tumor uptake. J Nucl Med 40:762–767
Baum R, Niesen A, Leonhardi J, Wortmann R, Mueller D, Roesch F (2005) Receptor PET/CT imaging of neuroendocrine tumours using the Ga-68 labelled, high affinity somatostatin analogue DOTA-1-Nal3 Octreotide (DOTA-NOC): clinical results in 327 patients. Eur J Nucl Med Mol Imaging 32(Suppl 1):54–55S (Abstract)
Ambrosini V, Castellucci P, Rubello D, Nanni C, Musto A, Allegri V, Montini GC, Mattioli S, Grassetto G, Al-Nahhas A, Franchi R, Fanti S (2009) 68Ga-DOTA-NOC: a new PET tracer for evaluating patients with bronchial carcinoid. Nucl Med Commun 30:281–286
Ambrosini V, Tomassetti P, Castellucci P, Campana D, Montini G, Rubello D, Nanni C, Rizzello A, Franchi R, Fanti S (2008) Comparison between 68Ga-DOTA-NOC and 18F-DOPA PET for the detection of gastro-entero-pancreatic and lung neuro-endocrine tumours. Eur J Nucl Med Mol Imaging 35:1431–1438
Fanti S, Ambrosini V, Tomassetti P, Castellucci P, Montini G, Allegri V, Grassetto G, Rubello D, Nanni C, Franchi R (2008) Evaluation of unusual neuroendocrine tumours by means of 68Ga-DOTA-NOC PET. Biomed Pharmacother 62:667–671
Prasad V, Ambrosini V, Hommann M, Hoersch D, Fanti S, Baum RP (2010) Detection of unknown primary neuroendocrine tumours (CUP-NET) using 68Ga-DOTA-NOC receptor PET/CT. Eur J Nucl Med Mol Imaging 37:67–77
Zasadny KR, Wahl RL (1993) Standardized uptake values of normal tissues at PET with 2-[fluorine-18]-fluoro-2-deoxy-d-glucose: variations with body weight and a method for correction. Radiology 189:847–850
Wehrmann C, Senftleben S, Zachert C, Müller D, Baum RP (2007) Results of individual patient dosimetry in peptide receptor radionuclide therapy with 177Lu DOTA-TATE and 177Lu DOTA-NOC. Cancer Biother Radiopharm 22:406–416
Zhernosekov KP, Filosofov DV, Baum RP, Aschoff P, Bihl H, Razbash AA, Jahn M, Jennewein M, Rösch F (2007) Processing of generator-produced 68Ga for medical application. J Nucl Med 48:1741–1748
Acknowledgments
We gratefully acknowledge the help of Dganit Barak and Ella Shamalove in assisting with patient preparation and organization. We acknowledge the role of Desideriu Laky of the Cyclotron/Radiochemistry Unit, Hadassah Hebrew University Hospital, Jerusalem, in the development of the tracer synthesis. We also acknowledge the contribution of Dani Vaknin and Avihai Y Bross of the Radiochemistry Department, Nahal Soreq NRC, Yavne, and Kobi Ben-Meir, Roni Michael of the Cyclotron Department, Nahal Soreq NRC, Yavne, for their part in organizing and participating in the synthesis of 68Ga-DOTA-NOC.
Conflict of Interest Disclosure
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
The manuscript’s significance: Our small prospective study investigates the clinical relevance of differences between imaging NETs with OctreoScan and the newer PET tracer, DOTA-NOC, with its improved patient tolerability, reduced machine and personnel time, and cost. Although the advantages of the new tracer have been described by others, systematic comparison is important to assess the differences between the two imaging methods before switching to DOTA-NOC.
Yodphat Krausz and Nanette Freedman contributed equally to this work.
Appendix: 68Ga-DOTA-NOC Synthesis
Appendix: 68Ga-DOTA-NOC Synthesis
68Ga-DOTA-NOC was prepared according to the procedure described by Zhernosekov et al. [22]. The radiochemical transformation was fully automated using the GE F-18 fluorination Tracerlab module with major hardware and software modifications. To the GE module, an electric Valco valve with 14 channels was added and connected to ten reagent vials and to a nitrogen gas supply valve. This electric Valco valve was connected by its exit to a three-way valve, which was further connected to a cation exchange column. The latter three-way valve was also connected via a series of valves to the 68Ge/68Ga generator (1,125–1,875 MBq, Obninsk Inc. Russia). The 68Ga was eluted with 5–7 ml 0.1 N HC1 (Ultrapure). The solution was passed through the cation exchanger column (Biorad 1X8, donated by Dr. Frank Roesch, Germany). In this manner, 99% of the activity eluted from the generator was trapped by the cation exchange column. Then, the column was washed with 1 ml, 80% acetone/20% 0.15 N HCl solution for the removal of 68Ge and other metal impurities. In the next step, 0.2 ml of the eluting solution (97.6% acetone/2.4% 0.05 N HCl) was loaded onto the column and left for 2.5 min; then, the 68Ga was eluted from the column using an additional 0.2 ml of the same eluting solution. In this manner, approx. 90% of the activity was recovered and transferred to the reactor which contained the starting material (DOTA-NOC [1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid]-1-NaI3-Octreotide acetate salt, 50 μg, GMP grade, ABX Germany) dissolved in 7.6 ml of HEPES buffer (pH 4.1). The peptide solution was pre-heated under vacuum for 1 min at approx 30°C prior to the addition of the solution of 68Ga, which was added drop-wise. Then, this solution was further heated to 98°C for an additional 8 min. The final pH of the reaction solution was 3.7. After cooling the solution to 30°C, the reaction mixture was loaded by nitrogen gas pressure onto RP C-18 (STRATA) column, which was further washed toward a waste vial by 5 ml of water (WFI). The pure 68Ga-DOTA-NOC was eluted from the column using 0.4 ml ethanol and 8.5 ml saline solution. Finally, the product solution was filtered via 0.22-μm GV sterile filter and collected in the product vial. During the process, the 68Ga activity was monitored by built-in radioactive detectors. The 68Ge content in both the generator eluent and in the final product was periodically measured by gamma spectroscopy using HPGE detector. The 68Ge eluted with the 68Ga was always in accordance with the manufacturer analysis certificate, while its presence in the final product was under the detectable limit. The chemical and radiochemical purity of the final product was determined by ITLC and HPLC: Method 1: ITLC-SG 60, mobile phase 0.1 M sodium citrate, pH 5, 68Ga-DOTA-NOC Rf = 0, free Ga-68 Rf = 0.9. Method 2: ITLC-SG 60 mobile phase 1 M ammonium acetate/methanol (1:1) 68Ga-DOTA-NOC Rf = 0.8–1, colloid Ga Rf = 0–0.2 HPLC; C18 column 250 × 4 mm; flow rate of 1 ml/min using a gradient solution. The gradient was gradually changed during the first 20 min from initial 20% acetonitrile/80% water +0.01% TFA to 40% acetonitrile/60% water + 0.01% TFA and following the end of the procedure was reversed gradually back to the original 20% acetonitrile/80% water +0.01% TFA, 68Ga-DOTA-NOC Rt = 18 min, and free 68Ga Rt = 2 min. The ethanol and acetone content in the final product were determined by GC. The acetone content was <0.5% and the ethanol was <5%. The average synthesis time including the generator eluting time (n = 40) was 23 min. The average radiochemical decay-corrected yield was 54 ± 4.74%, and the non-decay-corrected yield was 70 ± 3%. Radiochemical and chemical purity were >95%.
Initially, when working with low doses of activity, not more than approximately 500 MBq, we performed the synthesis in water (WFI), with a final pH of 2.2. However, when increasing the activity level to above 500 MBq, additional radioactive peaks were detected in the HPLC with retention times between 14 and 17 min. The calculated area percentage of these labeled by-products was dependent on the starting radioactivity levels, and it ranged between 10% and 35%. When the process was done in HEPES buffer, these impurities were eliminated and the purity of the final obtained product was >95%. The nature of these labeled by-products is unclear. We assume that when working with high activity doses, degradation of the starting material ensues. It seems that the HEPES molecules have a radio-protective effect. The stability of the product was monitored by ITLC and HPLC, 2.5 h post-EOS. There was no significant change in the purity of the 68Ga DOTA-NOC, and this permitted successful production.
Rights and permissions
About this article
Cite this article
Krausz, Y., Freedman, N., Rubinstein, R. et al. 68Ga-DOTA-NOC PET/CT Imaging of Neuroendocrine Tumors: Comparison with 111In-DTPA-Octreotide (OctreoScan®). Mol Imaging Biol 13, 583–593 (2011). https://doi.org/10.1007/s11307-010-0374-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-010-0374-1