Abstract
Human epidermal growth factor receptor 2 (HER2) amplification/overexpression is an effective therapeutic target in breast and gastric cancer. Although HER2 positivity has been reported in other malignancies, previous studies generally focused on one cancer type, making it challenging to compare HER2 positivity across studies/malignancies. Herein, we examined 37,992 patient samples for HER2 expression (+/− amplification) in a single laboratory. All 37,992 patients were tested by immunohistochemistry (IHC); 21,642 of them were also examined for HER2 amplification with either fluorescent in situ hybridization (FISH) (11,670 patients) or chromogenic in situ hybridization (CISH) (9,972 patients); 18,262 patients had tumors other than breast or gastric cancer. All tissues were analyzed in a Clinical Laboratory Improvement Amendments (CLIA) laboratory (Caris Life Sciences) at the request of referring physicians. HER2 protein overexpression was found in 2.7 % of samples. Over-expressed HER2 was detected predominantly in malignancies of epithelial origin; for cancers derived from mesenchyme, neuroendocrine tissue, central nervous system, and kidney, HER2 expression and amplification were remarkably rare or non-existent. Bladder carcinomas, gallbladder, extrahepatic cholangiocarcinomas, cervical, uterine, and testicular cancers showed HER2 positivity rates of 12.4, 9.8, 6.3, 3.9, 3.0, and 2.4 %, respectively. HER2 overexpression and/or amplification is frequently found across tumor types. These observations may have significant therapeutic implications in cancers not traditionally thought to benefit from anti-HER2 therapies.
Similar content being viewed by others
1 Introduction
The oncogenic potential of human epidermal growth factor receptor 2 (HER2) has been firmly established in preclinical and clinical settings. Among all four HER family proteins, HER2 has the strongest catalytic kinase activity and functions as the most active signaling complex of the HER family after dimerization with other HER family members [1, 2]. Overexpression of HER2 in breast cancer leads to increased homodimerization (HER2:HER2) and heterodimerization (e.g., HER2:HER3), which initiates a strong pro-tumorigenic signaling cascade [3]. Overexpression of HER2 protein drives malignant transformation in cell culture and transgenic mouse models [4, 5]. The anti-HER2 antibody trastuzumab represents an effective, targeted therapy with significant efficacy in treatment of HER2-positive breast and gastric cancer [6, 7]. Indeed, trastuzumab in combination with cisplatin and a fluoropyrimidine (capecitabine or 5-fluorouracil) has been approved for the treatment of patients with HER2 overexpressing metastatic gastric or gastroesophageal (GE) junction adenocarcinoma, who have not received prior treatment for metastatic disease [8]. The latter approval is based on a significant improvement in median overall survival (OS) of 2.5 months with trastuzumab plus chemotherapy treatment compared to chemotherapy alone, demonstrated in an international, multicenter, open-label, randomized clinical trial, BO18255 (ToGA trial) [6]. Furthermore, the family of approved anti-HER2 agents has been expanding in recent years, with the addition of small molecule inhibitors (e.g., lapatinib), antibodies (pertuzumab), and an antibody-drug conjugate (ado-trastuzumab emtansine, T-DM1). Used alone or in combination with other targeting agents or chemotherapy, these anti-HER2 agents have remarkably improved the outcome of patients with HER2-positive breast cancer [9, 10].
Breast and gastric cancers cases demonstrate a substantial HER2 protein overexpression by immunohistochemistry, predominantly driven by HER2 amplification at the DNA level. The majority of studies of HER2-targeting therapies have been focused on this group of HER2-positive breast or gastric cancer cases. However, HER2 amplification/overexpression is known to exist in a non-negligible subset of cancers outside of breast and stomach. For example, approximately 15–37 % of salivary duct carcinomas exhibit 3+ HER2 expression [11, 12]. Other malignancies including, but not limited to, non-small cell lung (NSCLC), ovarian, colon, and pancreatic cancer, overexpress HER2 protein and/or exhibit gene amplification in a variable percentage of cases [13, 14]. Additionally, mutations in HER2 have been described in a small subset of cancers of the breast, lung, ovary, and colon [13]. Anecdotal reports of patients with diverse cancers and HER2 amplification or mutation responding to anti-HER2 agents have been published [15–18], implying a potential role for anti-HER2 agents outside of breast and gastric cancer.
Multiple reports of studies evaluating the percentage of HER2 positivity in individual cancer types have shed some light on the distribution of HER2 positivity across individual cancer types [13]; however, given a lack of standardized methodology and interpretation criteria, it is challenging to compare the rate of HER2 positivity across studies and tumor types. Herein, we reviewed 37,992 patients with cancer, whose tumors were interrogated for HER2 protein expression with or without amplification in a single-lab setting. To our knowledge, this is the largest database that allows examination of HER2 across diverse malignancies. Overall, 2.7 % (1014/37,992) of all tumors tested demonstrated HER2 positivity determined by immunohistochemistry (IHC), and most types of cancer had a subset of patients, albeit often small, who demonstrated HER2 positivity determined by either in situ hybridization (ISH) and/or IHC. These data form the foundation for possible studies that assess HER2 therapy in a pan-cancer fashion.
2 Materials and methods
2.1 Tissue samples
Solid tumor specimens submitted to a commercial molecular profiling laboratory (Caris Life Sciences, Phoenix, Arizona; a CLIA, CAP, NYSDOH and ISO certified laboratory) were initially evaluated for this retrospective analysis of HER2. The pathologic diagnosis was obtained from the pathology report provided by the outside lab and was further reviewed and verified by board-certified pathologists at Caris. Tissue requirements and detailed processing methods in collection locations can be found in the Supplemental Methods. Multi-platform profiling included immunohistochemistry and in situ hybridization either by fluorescent in situ hybridization (FISH) or chromogenic in situ hybridization (CISH). This investigation was performed in accordance with UC San Diego IRB guidelines.
2.2 Immunohistochemistry
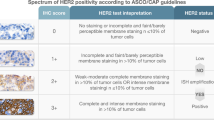
IHC analysis was performed on formalin-fixed, paraffin-embedded tissue utilizing the commercially available antibody PATHWAY anti-HER2 (4B5) rabbit monoclonal primary antibody (Ventana Medical Systems). All IHCs were performed using commercially available detection kits and automated membranous staining techniques (Benchmark XT, Ventana, USA). HER2 scoring was reported per American Society of Clinical Oncology/College of American Pathologists (ASCO/CAP) guidelines published in 2007 [14] and updated in 2013 [19, 20]. For the purpose of our analysis, an IHC test was considered positive (IHC+) when IHC3+ was obtained above the guidelines defined thresholds; an IHC test was considered negative (IHC-) when IHC 2+ (equivocal), IHC 1+, or IHC 0 was obtained.
2.3 HER2 in situ hybridization
Among the 37,992 samples analyzed by IHC, 21,642 samples were also examined with ISH. FISH was used for evaluation of the HER2 amplification status. HER2/CEP17 ratio higher than 2.2 was considered amplified [14] (ISH+), and HER2/CEP17 ratio between 1.8 and 2.2 (equivocal) in FISH or HER2/CEP17 ratio <1.8 in FISH was considered non-amplified (ISH-). HER2 amplification was also evaluated by CISH (INFORM HER2 dual ISH DNA probe cocktail, Ventana). Consistent with the CISH package insert, HER2/CEP17 ratio higher than 2.0 was considered amplified (ISH+); HER2/CEP17 ratio <2.0 in CISH was considered non-amplified (ISH-).
2.3.1 HER2 fluorescent in situ hybridization
FISH was performed with a probe specific for HER2 (17q11.2-q12 region) and a probe for the pericentromeric region of chromosome 17 (Abbott Molecular/Vysis). Interphase nuclei were examined and the ratio of HER2 signals to chromosome 17 centromere signals were evaluated to indicate amplification status of this gene. The HER2 Pathvysion probe has been approved by the US Food and Drug Administration for selection of patients for trastuzumab and pertuzumab therapy.
2.3.2 HER2 chromogenic in situ hybridization
CISH was performed by using Ventana Medical Systems, Inc.’s (Ventana) INFORM HER2 Dual ISH DNA Probe Cocktail as intended to determine HER2 gene status by enumeration of the ratio of the HER2 gene to chromosome 17. The HER2 and chromosome 17 probes are detected using two color ISH in formalin-fixed, paraffin-embedded human cancer tissue specimens following staining on VENTANA BenchMark XT automated slide stainer, and visualized by light microscopy. The INFORM HER2 Dual ISH DNA Probe Cocktail has been approved by the US Food and Drug Administration for selection of patients to HER2 targeted therapies in breast cancer.
2.4 Statistical methods
Descriptive statistics were used. For Table 2, the concordance between the IHC and ISH tests was calculated by dividing the number of samples that had concordant results for both IHC and ISH tests (IHC+ and ISH+; or IHC- and ISH-) by the total number of samples within each malignancy types. JMPv10.0 (SAS Institute Inc., Cary, NC) was utilized.
3 Results
3.1 HER2 protein expression in various malignancies
As shown in Table 1 and Fig. 1, HER2 protein 3+ expression by IHC was demonstrated in a subset of virtually all examined carcinomas derived from epithelial origin. The frequency ranged from 0.4 % in hepatocellular carcinoma to 12.4 % in bladder cancer. Table 3 gives examples of positivity rates found in the literature. Interestingly, HER2 protein 3+ expression was very rare, often non-existent, in malignancies of non-epithelial origin. In 965 melanoma samples, only one showed HER2 3+ expression. In 1,211 sarcomas (soft tissues) and 1,136 neuroendocrine tumors, none exhibited 3+ HER2 protein expression. No HER2 3+ expression was detected in gastrointestinal stromal tumors (GIST), small cell lung cancers (SCLC), kidney cancers, and glioblastomas.
3.2 HER2 positivity determined by IHC and ISH in various malignancies
HER2 protein expression determined by IHC and HER2 gene amplification determined by ISH were examined in a total of 21,642 samples. Consistent with HER2 protein expression pattern, HER2 gene amplification was predominantly detected in malignancies derived from epithelial origin and very rarely found in cancers derived from other tissue origins; HER2 amplification was seen in only one out of 60 retroperitoneal/peritoneal sarcomas, four out of 237 kidney cancers, and none in GISTs (0/59), small cell lung cancers (0/108), or melanomas (0/388). A total of 705 samples were found to be HER2 positive by IHC; 638 (90.5 %) of them were also positive by ISH testing. Among breast cancer cases, 286 samples tested IHC+; 266 of them (93 %) were also positive by ISH. The overall concordance rate (IHC+ and ISH+; or IHC- and ISH-) between the two tests was 96.3 % (Table 2).
4 Discussion
Our recent review of the literature that examined HER2 amplification/overexpression in a variety of cancers outside of breast and stomach [13] found that almost all studies focused on HER2 status in one type of malignancy, making it difficult to compare the rate of HER2 positivity across studies and tumor types. Herein, we have analyzed 37,992 patients with cancer whose tumors were interrogated for HER2 protein expression in a single, accredited laboratory setting. We report that 2.7 % of all cancer samples demonstrated HER2 overexpression (3+ on IHC) (Table 1). To our knowledge, this is the largest database that interrogated HER2 across diverse malignancies. These observations provide a consistent comparison of HER2 status between individual tumor types that could be used to inform future trials of anti-HER2 therapy outside of breast and stomach cancer. For example, the incidence of HER2 overexpression by IHC in bladder cancers (12.4 %) is even higher than that found in breast cancer (10.5 %) (Fig. 1), suggesting that a trial of anti-HER2 agents may be warranted in patients with advanced bladder cancer. HER2 overexpression by IHC was also substantial in gallbladder cancers (9.8 %). When reviewing the literature, it was noticeable that studies demonstrated variability in rates of HER2 overexpression (Table 3), making our results difficult to compare with other published series. This variability can be explained by the differing criteria used for the evaluation of HER2 positivity in the studies found in the literature, due in part by the lack of standardized methodology for HER2 detection outside of gastric and breast cancers [13]. Of interest, we report that approximately 10.5 % of breast cancer patients are HER2 positive by IHC, which appears to be in the lower range when compared to published reports (11–25 %, Table 3). Varga et al. [26] investigated HER2 positivity in more than 7,000 patients with breast cancers over a 12-year period and showed a drop in the expression rate (probably due to the modified ASCO criteria in 2007), which went from 22 to 12 % over the years. The decrease in HER2 positivity rate can also potentially be explained by the introduction of mammography screening with improved detection of early breast cancers, as screen detection resulted in a shift to a different patient population with less HER2 positive cases in early breast cancer and with younger age at diagnosis [39, 40]. Lastly, the lower percentage of HER2 positivity rate in our study may be due to a higher proportion of triple-negative breast cancer specimens sent to the testing laboratory (35.8 % (Caris, data on file) as compared to 15–20 % of the general breast cancer population [19, 41]). Due to the aggressive nature of triple-negative breast cancer, a higher percentage may be evaluated for the molecular profiling that generally is performed with HER2 testing in the laboratory. One interesting pattern of HER2 positivity became apparent with direct comparison of HER2 status across different tumor types: overexpressed HER2 is predominantly found in malignancies of epithelial origin. For cancers derived from mesenchyme, neuroendocrine tissue, central nervous system, and kidney, HER2 expression and HER2 gene amplification are negligible (Fig. 1).
HER2 gene amplification is the major mechanism driving HER2 overexpression in breast cancer [39]. It has been noted before that HER2 protein may not be consistently analyzed in formalin-fixed tissues because of variations in methods and duration of fixation, in comparison to ISH analysis that is less dependent on tissue fixation methods [14, 39, 40]. Alternatively, it is plausible that there are transcriptional or translational mechanisms that could attenuate HER2 expression in some cases, even in the presence of amplification. The overall (positive and negative) concordance rate between methodologies was about 96 % in our cohort, which is in accordance with the American Society of Clinical Oncology/College of American Pathologists guideline that any two diagnostic companion tests should establish a concordance rate of >95 % for positive and negative assay values [14]. Further, 90 % of all samples and 93 % of breast cancer cases that were tested HER2 positive by IHC, were also found positive by ISH. This percentage stands in the higher range of what has been published. For example, the positivity concordance rates (IHC+ tests also found positive by FISH) reported by different groups ranged from 69 to 98 %, with most of them being around 85 % [26, 41–43].
There are several limitations to our study. The current pool of samples cover a wide range of malignancies but there may be selection bias of the specimens, as patients/physicians may have elected to submit tissue when there were fewer standard therapeutic options left, and often for advanced and/or more difficult to treat cancers (refractory and recurrent). Also, the samples came from diverse institutes and practices, and differences in processing and storage could still have affected samples, even if the HER2 analysis itself was performed by a single organization. Finally, the current study addressed HER2 overexpression. It has recently been shown that HER2 can demonstrate mutations in about 1.8 % of diverse cancers (∼7300 solid tumor specimens tested) and that rearrangements can be seen, albeit very rarely (∼0.02 % of patients) [44]. In summary, we have examined 37,992 samples for HER2 expression (with 21,642 of them also examined for HER2 amplification) and profiled HER2 status across different tumor types. Overall, 2.7 % of all cancers tested were IHC 3+ positive. High levels of HER2 were seen in a subset of patients with most epithelial malignancies examined. For non-epithelial cancers such as melanoma, GIST, small cell lung cancers, and glioblastomas, almost no HER2 overexpression was discerned. Some tumors such as bladder, gallbladder, and cholangiocarcinomas showed significant rates of HER2 positivity (greater than 5 %), and testicular, ovarian, uterine, cervical, head and neck, non-small cell lung, and colorectal cancer as well as tumors of unknown origin all showed small but not negligible rates of positivity. Of additional interest, a small percentage of tumors may also have HER2 mutations that are amenable to targeted HER2 agents, and these patients would not be expected to have high expression levels of HER2 [13, 15–18]. An early histology-independent trial using lapatinib monotherapy for HER2-expressing tumors faced logistical challenges and showed only modest activity [45]. However, in the last several years, there has been increasing experience with target-driven trials and overcoming their logistical challenges [46–48]. Our data presented herein, as well as the advent of numerous, potent small molecule inhibitors, antibodies and other agents that target HER2, suggest that it may be worthwhile to enrich clinical trials using HER2-targeting agents with patients that have HER2-positive tumors other than breast and gastric.
References
Garrett, T. P. J., McKern, N. M., Lou, M., Elleman, T. C., Adams, T. E., Lovrecz, G. O., … Ward, C. W. (2003). The crystal structure of a truncated ErbB2 ectodomain reveals an active conformation, poised to interact with other ErbB receptors. Molecular Cell, 11(2), 495–505.
Graus-Porta, D., Beerli, R. R., Daly, J. M., & Hynes, N. E. (1997). ErbB-2, the preferred heterodimerization partner of all ErbB receptors, is a mediator of lateral signaling. The EMBO Journal, 16(7), 1647–1655. doi:10.1093/emboj/16.7.1647.
Holbro, T., Beerli, R. R., Maurer, F., Koziczak, M., Barbas, C. F., 3rd, & Hynes, N. E. (2003). The ErbB2/ErbB3 heterodimer functions as an oncogenic unit: ErbB2 requires ErbB3 to drive breast tumor cell proliferation. Proceedings of the National Academy of Sciences of the United States of America, 100(15), 8933–8938. doi:10.1073/pnas.1537685100.
Di Fiore, P. P., Pierce, J. H., Kraus, M. H., Segatto, O., King, C. R., & Aaronson, S. A. (1987). erbB-2 is a potent oncogene when overexpressed in NIH/3T3 cells. Science (New York, N.Y.), 237(4811), 178–182.
Ursini-Siegel, J., Schade, B., Cardiff, R. D., & Muller, W. J. (2007). Insights from transgenic mouse models of ERBB2-induced breast cancer. Nature reviews. Cancer, 7(5), 389–397. doi:10.1038/nrc2127.
Bang, Y.-J., Van Cutsem, E., Feyereislova, A., Chung, H. C., Shen, L., Sawaki, A., … ToGA Trial Investigators. (2010). Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet, 376(9742), 687–697. doi:10.1016/S0140-6736(10)61121-X.
Romond, E. H., Perez, E. A., Bryant, J., Suman, V. J., Geyer, C. E., Jr, Davidson, N. E., … Wolmark, N. (2005). Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. The New England Journal of Medicine, 353(16), 1673–1684. doi:10.1056/NEJMoa052122.
CDER. (n.d.). Retrieved from http://www.fda.gov/AboutFDA/CentersOffices/OfficeofMedicalProductsandTobacco/CDER/ucm230418.htm
Baselga, J., Cortés, J., Kim, S.-B., Im, S.-A., Hegg, R., Im, Y.-H., … Swain, S. M. (2012). Pertuzumab plus Trastuzumab plus Docetaxel for Metastatic Breast Cancer. New England Journal of Medicine, 366(2), 109–119. doi:10.1056/NEJMoa1113216.
Verma, S., Miles, D., Gianni, L., Krop, I. E., Welslau, M., Baselga, J., … EMILIA Study Group. (2012). Trastuzumab emtansine for HER2-positive advanced breast cancer. The New England Journal of Medicine, 367(19), 1783–1791. doi:10.1056/NEJMoa1209124.
Nardi, V., Sadow, P. M., Juric, D., Zhao, D., Cosper, A. K., Bergethon, K., … Dias-Santagata, D. (2013). Detection of novel actionable genetic changes in salivary duct carcinoma helps direct patient treatment. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research, 19(2), 480–490. doi:10.1158/1078-0432.CCR-12-1842
Williams, M. D., Roberts, D. B., Kies, M. S., Mao, L., Weber, R. S., & El-Naggar, A. K. (2010). Genetic and expression analysis of HER-2 and EGFR genes in salivary duct carcinoma: empirical and therapeutic significance. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research, 16(8), 2266–2274. doi:10.1158/1078-0432.CCR-09-0238.
Yan, M., Parker, B. A., Schwab, R., & Kurzrock, R. (n.d.). HER2 aberrations in cancer: Implications for therapy. Cancer Treatment Reviews. doi:10.1016/j.ctrv.2014.02.008
Wolff, A. C., Hammond, M. E. H., Schwartz, J. N., Hagerty, K. L., Allred, D. C., Cote, R. J., … College of American Pathologists. (2007). American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 25(1), 118–145. doi:10.1200/JCO.2006.09.2775
Falchook, G. S., Janku, F., Tsao, A. S., Bastida, C. C., Stewart, D. J., & Kurzrock, R. (2013). Non-small-cell lung cancer with HER2 exon 20 mutation: regression with dual HER2 inhibition and anti-VEGF combination treatment. Journal of Thoracic Oncology: official Publication of the International Association for the Study of Lung Cancer, 8(2), e19–e20. doi:10.1097/JTO.0b013e31827ce38e.
Falchook, G. S., Lippman, S. M., Bastida, C. C., & Kurzrock, R. (2014). Human epidermal receptor 2-amplified salivary duct carcinoma: regression with dual human epidermal receptor 2 inhibition and anti-vascular endothelial growth factor combination treatment. Head & Neck, 36(3), E25–E27. doi:10.1002/hed.23429.
Cappuzzo, F., Bemis, L., & Varella-Garcia, M. (2006). HER2 mutation and response to trastuzumab therapy in non-small-cell lung cancer. The New England Journal of Medicine, 354(24), 2619–2621. doi:10.1056/NEJMc060020.
Kelly, R. J., Carter, C. A., & Giaccone, G. (2012). HER2 mutations in non-small-cell lung cancer can be continually targeted. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 30(26), 3318–3319. doi:10.1200/JCO.2012.43.4902.
Wolff, A. C., Hammond, M. E. H., Hicks, D. G., Dowsett, M., McShane, L. M., Allison, K. H., … College of American Pathologists. (2013). Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 31(31), 3997–4013. doi:10.1200/JCO.2013.50.9984.
Ruschoff, J., Dietel, M., Baretton, G., Arbogast, S., Walch, A., Monges, G., … Kreipe, H. H. (2010). HER2 diagnostics in gastric cancer--guideline validation and development of standardized immunohistochemical testing. Virchows Archiv, 457(3), 299–307. doi:10.1007/s00428-010-0952-2.
Charfi, S., Khabir, A., Mnif, H., Ellouze, S., Mhiri, M. N., & Boudawara-Sellami, T. (2013). Immunohistochemical expression of HER2 in urothelial bladder carcinoma and its correlation with p53 and p63 expression. Journal of Microscopy and Ultrastructure, 1(1–2), 17–21. doi:10.1016/j.jmau.2013.06.001.
Fleischmann, A., Rotzer, D., Seiler, R., Studer, U. E., & Thalmann, G. N. (2011). Her2 amplification is significantly more frequent in lymph node metastases from urothelial bladder cancer than in the primary tumours. European Urology, 60(2), 350–357. doi:10.1016/j.eururo.2011.05.035.
Laé, M., Couturier, J., Oudard, S., Radvanyi, F., Beuzeboc, P., & Vieillefond, A. (2010). Assessing HER2 gene amplification as a potential target for therapy in invasive urothelial bladder cancer with a standardized methodology: results in 1005 patients. Annals of Oncology: Official Journal of the European Society for Medical Oncology / ESMO, 21(4), 815–819. doi:10.1093/annonc/mdp488.
Caner, V., Turk, N. S., Duzcan, F., Tufan, N. L. S., Kelten, E. C., Zencir, S., … Duzcan, S. E. (2008). No strong association between HER-2/neu protein overexpression and gene amplification in high-grade invasive urothelial carcinomas. Pathology oncology research: POR, 14(3), 261–266. doi:10.1007/s12253-008-9027-y.
Gandour-Edwards, R., Lara, P. N., Folkins, A. K., LaSalle, J. M., Beckett, L., Li, Y., … DeVere-White, R. (2002). Does HER2/neu expression provide prognostic information in patients with advanced urothelial carcinoma? Cancer, 95(5), 1009–1015. doi:10.1002/cncr.10808.
Varga, Z., Noske, A., Ramach, C., Padberg, B., & Moch, H. (2013). Assessment of HER2 status in breast cancer: overall positivity rate and accuracy by fluorescence in situ hybridization and immunohistochemistry in a single institution over 12 years: a quality control study. BMC Cancer, 13(1), 615. doi:10.1186/1471-2407-13-615.
Stenehjem, D. D., Yoo, M., Unni, S. K., Singhal, M., Bauer, H., Saverno, K., … Brixner, D. I. (2014). Assessment of HER2 testing patterns, HER2+ disease, and the utilization of HER2-directed therapy in early breast cancer. Breast Cancer (Dove Medical Press), 6, 169–177. doi:10.2147/BCTT.S69416
Chavez-Blanco, A., Perez-Sanchez, V., Gonzalez-Fierro, A., Vela-Chavez, T., Candelaria, M., Cetina, L., … Dueñas-Gonzalez, A. (2004). HER2 expression in cervical cancer as a potential therapeutic target. BMC Cancer, 4(1), 59. doi:10.1186/1471-2407-4-59.
Yoshikawa, D., Ojima, H., Iwasaki, M., Hiraoka, N., Kosuge, T., Kasai, S., … Shibata, T. (2008). Clinicopathological and prognostic significance of EGFR, VEGF, and HER2 expression in cholangiocarcinoma. British Journal of Cancer, 98(2), 418–425. doi:10.1038/sj.bjc.6604129
Seo, A. N., Kwak, Y., Kim, D.-W., Kang, S.-B., Choe, G., Kim, W. H., & Lee, H. S. (2014). HER2 status in colorectal cancer: its clinical significance and the relationship between HER2 gene amplification and expression. PloS One, 9(5), e98528. doi:10.1371/journal.pone.0098528.
Schuell, B., Gruenberger, T., Scheithauer, W., Zielinski, C., & Wrba, F. (2006). HER 2/neu protein expression in colorectal cancer. BMC Cancer, 6(1), 123. doi:10.1186/1471-2407-6-123.
Ingold Heppner, B., Behrens, H.-M., Balschun, K., Haag, J., Krüger, S., Becker, T., & Röcken, C. (2014). HER2/neu testing in primary colorectal carcinoma. British Journal of Cancer, 111(10), 1977–1984. doi:10.1038/bjc.2014.483.
Yoon, H. H., Shi, Q., Sukov, W. R., Sattler, C. A., Wiktor, A. E., Wu, T.-T., … Sinicrope, F. A. (2013). HER2 testing in esophageal adenocarcinoma (EAC) using parallel tissue-based methods. Journal of Clinical Oncology, 31(suppl 4; abstr 2). Retrieved from http://meetinglibrary.asco.org/content/105406-133
Wang, T., Hsieh, E. T., Henry, P., Hanna, W., Streutker, C. J., & Grin, A. (2014). Matched biopsy and resection specimens of gastric and gastroesophageal adenocarcinoma show high concordance in HER2 status. Human Pathology, 45(5), 970–975. doi:10.1016/j.humpath.2013.12.010.
König, A. M., Reeh, M., Dancau, A.-M., Rathjens, M., Gros, S., Uzunoglu, F. G., … Izbicki, J. R. (2013). Concordance of HER2 status in primary tumour and lymph node metastases in patients with esophageal carcinoma. Anticancer Research, 33(11), 4975–4982.
Roa, I., de Toro, G., Schalper, K., de Aretxabala, X., Churi, C., & Javle, M. (2014). Overexpression of the HER2/neu Gene: a new therapeutic possibility for patients with advanced gallbladder cancer. Gastrointestinal Cancer Research : GCR, 7(2), 42–48.
Rüschoff, J., Hanna, W., Bilous, M., Hofmann, M., Osamura, R. Y., Penault-Llorca, F., … Viale, G. (2012). HER2 testing in gastric cancer: a practical approach. Modern Pathology, 25(5), 637–650. doi:10.1038/modpathol.2011.198.
Hofmann, M., Stoss, O., Shi, D., Büttner, R., Van De Vijver, M., Kim, W., … Henkel, T. (2008). Assessment of a HER2 scoring system for gastric cancer: results from a validation study. Histopathology, 52(7), 797–805. doi:10.1111/j.1365-2559.2008.03028.x.
Sauter, G., Lee, J., Bartlett, J. M. S., Slamon, D. J., & Press, M. F. (2009). Guidelines for human epidermal growth factor receptor 2 testing: biologic and methodologic considerations. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 27(8), 1323–1333. doi:10.1200/JCO.2007.14.8197.
Perez, E. A., Cortés, J., Gonzalez-Angulo, A. M., & Bartlett, J. M. S. (2014). HER2 testing: current status and future directions. Cancer Treatment Reviews, 40(2), 276–284. doi:10.1016/j.ctrv.2013.09.001.
Gown, A. M., Goldstein, L. C., Barry, T. S., Kussick, S. J., Kandalaft, P. L., Kim, P. M., & Tse, C. C. (2008). High concordance between immunohistochemistry and fluorescence in situ hybridization testing for HER2 status in breast cancer requires a normalized IHC scoring system. Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc, 21(10), 1271–1277. doi:10.1038/modpathol.2008.83.
Perez, E. A., Press, M. F., Dueck, A. C., Jenkins, R. B., Kim, C., Chen, B., … Slamon, D. J. (2013). Immunohistochemistry and fluorescence in situ hybridization assessment of HER2 in clinical trials of adjuvant therapy for breast cancer (NCCTG N9831, BCIRG 006, and BCIRG 005). Breast Cancer Research and Treatment, 138(1), 99–108. doi:10.1007/s10549-013-2444-y.
Bahreini, F., Soltanian, A. R., & Mehdipour, P. (2014). A meta-analysis on concordance between immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH) to detect HER2 gene overexpression in breast cancer. Breast cancer (Tokyo, Japan). doi:10.1007/s12282-014-0528-0.
Chmielecki, J., Ross, J. S., Wang, K., Frampton, G. M., Palmer, G. A., Ali, S. M., … Stephens, P. J. (2015). Oncogenic Alterations in ERBB2/HER2 Represent Potential Therapeutic Targets Across Tumors From Diverse Anatomic Sites of Origin. The Oncologist, 20(1), 7–12. doi:10.1634/theoncologist.2014-0234
Galsky, M. D., Von Hoff, D. D., Neubauer, M., Anderson, T., Fleming, M., Nagarwala, Y., … Zaks, T. Z. (2012). Target-specific, histology-independent, randomized discontinuation study of lapatinib in patients with HER2-amplified solid tumors. Investigational New Drugs, 30(2), 695–701. doi:10.1007/s10637-010-9541-0.
Tsimberidou, A.-M., Iskander, N. G., Hong, D. S., Wheler, J. J., Falchook, G. S., Fu, S., … Kurzrock, R. (2012). Personalized medicine in a phase I clinical trials program: the MD Anderson Cancer Center initiative. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research, 18(22), 6373–6383. doi:10.1158/1078-0432.CCR-12-1627.
Heinrich, M. C., Joensuu, H., Demetri, G. D., Corless, C. L., Apperley, J., Fletcher, J. A., … Imatinib Target Exploration Consortium Study B2225. (2008). Phase II, open-label study evaluating the activity of imatinib in treating life-threatening malignancies known to be associated with imatinib-sensitive tyrosine kinases. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research, 14(9), 2717–2725. doi:10.1158/1078-0432.CCR-07-4575.
Janku, F., Hong, D. S., Fu, S., Piha-Paul, S. A., Naing, A., Falchook, G. S., … Kurzrock, R. (2014). Assessing PIK3CA and PTEN in early-phase trials with PI3K/AKT/mTOR inhibitors. Cell Reports, 6(2), 377–387. doi:10.1016/j.celrep.2013.12.035
Acknowledgments
Funded in part by the Joan and Irwin Jacobs Fund philanthropic fund.
Conflicts of interest
ZG, SM, and DA are employees of Caris Life Sciences; DA and ZG disclose stock ownership. Dr. Kurzrock is a founder of RScueRX and receives consultant fees from Sequenom. The other author(s) indicated no potential conflicts of interest.
Financial support
Funded in part by the Joan and Irwin Jacobs philanthropic fund.
Author information
Authors and Affiliations
Corresponding author
Additional information
Min Yan and Maria Schwaederle contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 37 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Yan, M., Schwaederle, M., Arguello, D. et al. HER2 expression status in diverse cancers: review of results from 37,992 patients. Cancer Metastasis Rev 34, 157–164 (2015). https://doi.org/10.1007/s10555-015-9552-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-015-9552-6