Abstract
Neoadjuvant chemotherapy trials have consistently reported lower response rates in hormone receptor-positive (HR+) breast cancer when compared with HR− cases. Preoperative endocrine therapy has therefore become a logical alternative and has gained considerable momentum from the finding that aromatase inhibitors (AIs) are more effective than tamoxifen for HR+ breast cancer in both the neoadjuvant and adjuvant settings. The most convincing neoadjuvant trial to demonstrate the superiority of an AI versus tamoxifen was the P024 study, a large multinational double-blind trial in postmenopausal women with HR+ breast cancer ineligible for breast-conserving surgery. The overall response rate (ORR) was 55% for letrozole and 36% for tamoxifen (P < 0.001). Significantly more letrozole-treated patients underwent breast-conserving surgery (45 vs. 35%, respectively; P = 0.022). In addition, ORR was significantly higher with letrozole than tamoxifen in the human epidermal growth factor receptor HER1/HER2+ subgroup (P = 0.0004). The clinical efficacy of letrozole in HER2+ breast cancer was confirmed by fluorescent in situ hybridization analysis and was found to be comparable to that of HER2− cases (ORR 71% in both subsets). Biomarker studies confirmed the superiority of letrozole in centrally assessed estrogen receptor-positive (ER+) tumors and found a strong relationship with the degree of ER positivity for both agents. Interestingly, letrozole was effective even in marginally ER+ tumors and, unlike tamoxifen, consistently reduced the expression from estrogen-regulated genes (progesterone receptor and trefoil factor 1). Furthermore, when analyzed by Ki67 immunohistochemistry, letrozole was significantly more effective than tamoxifen in reducing tumor proliferation (P = 0.0009). Thus, neoadjuvant letrozole is safe and superior to tamoxifen in the treatment of postmenopausal women with HR+ locally advanced breast cancer.
Similar content being viewed by others
Introduction and rationale
Early-stage breast cancer is traditionally treated with an initial surgery such as lumpectomy or mastectomy followed by subsequent adjuvant therapy, including radiotherapy, chemotherapy, and hormone therapy [1, 2]. Numerous studies have investigated the use of preoperative (neoadjuvant) hormonal therapy or chemotherapy prior to surgical intervention, with the goals to improve surgical outcome and obtain long-term disease-free survival (DFS) (see Table 1). The National Surgical Adjuvant Breast and Bowel Project B-18 trial demonstrated that doxorubicin and cyclophosphamide administered as neoadjuvant or adjuvant therapy had equivalent outcomes in terms of both DFS and overall survival (OS) [3]. Adding a taxane in the B-27 trial significantly reduced the local recurrence rate but did not significantly increase DFS or OS [4]. Importantly, neoadjuvant chemotherapy has been shown to increase the rate of breast-conserving surgery (BCS) without adversely affecting DFS or OS [3, 5–7]. Therefore, neoadjuvant chemotherapy has become the standard treatment approach for locally advanced breast cancer and an accepted option for patients with primary operable disease [8].
Significant tumor reduction from neoadjuvant chemotherapy occurs in only subsets of breast cancer, however. For example, patients with estrogen receptor-negative (ER−), high-grade, and highly proliferative tumors appear to benefit the most from neoadjuvant chemotherapy [9–11]. In contrast, significantly lower response rates have been reported in patients with ER+ tumors in neoadjuvant chemotherapy trials [12–15]. The German Breast Group demonstrated that the pathologic complete response (pCR) rates were 6.2 versus 22.8% for ER+ and ER− tumors, respectively (odds ratio 3.23, 95% confidence intervals [CIs] 1.91, 5.46; P = 0.0001) [12]. Recent studies indicate that the sensitivity to chemotherapy is likely determined by the underlying gene expression pattern and the molecular subtype of the tumor [16, 17]. The luminal subtype categorized by gene expression profiling, which encompasses most of the ER+ tumors, is less responsive to preoperative chemotherapy than the basal-like and human epidermal growth factor receptor 2-positive (HER2+) cancer. In addition, neoadjuvant chemotherapy is associated with substantial toxicity that may limit its clinical benefits and acceptability, especially in the elderly patient population [13, 18–20]. Thus, there is great need for effective alternatives to cytotoxic chemotherapy in hormone-responsive locally advanced breast cancer.
Endocrine treatment is an attractive alternative to chemotherapy as neoadjuvant or primary systemic therapy for women with hormone-responsive primary breast tumors [21–23]. A study comparing neoadjuvant endocrine therapy with exemestane versus chemotherapy in 152 patients with ER+/progesterone receptor-positive (PgR+) breast cancer found that while efficacy outcomes were comparable in the two groups, chemotherapy treatment was significantly more toxic, confirming that endocrine therapy could be used as an alternative to chemotherapy in older women [24]. Early studies of primary tamoxifen as an alternative to surgery were conducted in older women with hormone-responsive breast cancer who were unfit for chemotherapy [23, 25–27]. While these studies demonstrated a reduction in tumor size with primary tamoxifen, long-term local disease control was found to be poor. The omission of primary surgery resulted in an increased rate of progression, therapeutic intervention, and mortality [28]. Thus, primary tamoxifen treatment is indicated for only the most frail, medically ill, or noncompliant patients [29]. Although primary therapy with tamoxifen was found to be well-tolerated, adverse effects were reported including hot flushes, skin rash, vaginal discharge, breast pain, sleepiness, headache, vertigo, itching, hair loss, cystitis, acute thrombophlebitis, nausea, and indigestion [29]. Furthermore, more serious adverse effects, such as an increased risk of endometrial cancer and thromboembolic events, have been reported in large trials of adjuvant tamoxifen [30].
In view of the limitations of tamoxifen as a single modality treatment, attention has switched to the neoadjuvant use of endocrine therapy to increase the rate of breast conservation [21]. Data from preclinical models [31] and clinical studies in advanced breast cancer [32] predict that aromatase inhibitors (AIs) may be more effective than tamoxifen in the neoadjuvant setting. Furthermore, preclinical and clinical evidence suggests that letrozole may be the most effective AI in this setting [33–35]. In postmenopausal women with endocrine-responsive locally advanced or metastatic breast cancer, first-line treatment with letrozole was shown to be significantly more effective than tamoxifen in terms of response rate (overall response rate [ORR], 30 vs. 20%, P = 0.0006) and time to disease progression (41 vs. 26 weeks) [32]. A phase 1–2 pilot study showed a clinical response rate of 88% (21/24 patients) in postmenopausal women with ER+ locally advanced breast cancer treated with letrozole for 3 months prior to surgery [36]. All patients in the study were eligible for breast conserving surgery following neoadjuvant letrozole.
A large multinational trial, P024, was designed to assess the efficacy of neoadjuvant letrozole compared with tamoxifen in postmenopausal women with hormone receptor-positive (HR+) breast cancer who were ineligible for breast-conserving surgery [21]. The clinical objectives of the trial were to compare response rates and surgical outcomes between the two treatment arms. In addition, the trial provided the opportunity to conduct prospective biomarker studies to explore the biologic basis for response to neoadjuvant endocrine therapy [37]. This review describes the results of the P024 study and the follow-up biomarker studies, focusing on the treatment implications in the neoadjuvant setting.
Trial design and patients
PO24 was a multinational, randomized, double-blind controlled trial comparing letrozole and tamoxifen in postmenopausal women with hormone-responsive primary invasive breast cancer who were not eligible for breast-conserving surgery [21]. The trial was conducted in 55 centers in 16 countries between March 1998 and August 1999. Local ethics review boards approved the protocol and all patients gave written informed consent before study enrollment.
Randomized clinical trial design
Patients were randomly assigned to receive letrozole 2.5 mg or tamoxifen 20 mg administered orally once daily for 4 months prior to scheduled surgery [21]. Patients were considered to have completed the study when they had received 4 months of treatment and had been assessed for surgery. Following surgery, patients were treated at the investigator’s discretion and were followed for 5 years for local recurrence, distant metastasis, and survival.
Patient population
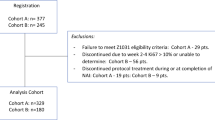
A total of 337 postmenopausal women were enrolled into the trial, and 324 were included in the intent-to-treat population (see Fig. 1). Eligible patients were postmenopausal women with untreated, primary HR+ (≥10% nuclear staining for ER or PgR) invasive breast tumors (stages T2–4a–c, N0–2, M0). The minimum tumor size was ≥3 cm, and all patients were considered inoperable or ineligible for breast-conserving surgery, mostly because of a non-favorable ratio tumor size/breast size. Exclusion criteria included previous exposure to AIs, uncontrolled endocrine or cardiac disease, bilateral or inflammatory breast cancer, distant metastasis, and other malignant disease. In addition, administration of other cancer treatment or hormone replacement therapy was not allowed during study participation.
Patient disposition [21]
Trial end points
The primary end point was ORR, defined as the percentage of patients in each treatment arm with a complete response (CR) or a partial response (PR) as determined by breast palpation [21]. Response categories were CR, PR, no change, progressive disease, or not assessable/not evaluable. The secondary end points were the percentage of patients who underwent breast-conserving surgery and the response rate (CR + PR) determined at 4 months by mammography and by ultrasound [21]. Safety was assessed and adverse events graded according to the National Cancer Institute Common Toxicity Criteria.
Correlative science studies
In parallel, studies were conducted in which tumor biopsies and blood samples were taken from all patients prior to the initiation of therapy and at the end of treatment to generate a database from which changes in molecular markers could be assessed [37–41]. These studies were prospectively designed to assess the biological basis for letrozole efficacy. The specific objectives of the biomarker sub-studies were as follows:
-
1.
To confirm ER and PgR status in a central laboratory. ER and PgR were determined using immunohistochemistry (IHC) performed on pretreatment biopsies; the criterion for minimal ER positivity was 10% positive cells [37]. The Allred histopathological score was applied to further assess the level of ER and PgR expression in both the baseline and surgical specimens [42].
-
2.
To explore relationships between ER and PgR expression levels and response to treatment [37].
-
3.
To examine the relationship between the expression of HER1 and HER2 and the likelihood of primary response [37]. Previous studies have shown that HER2 overexpression may be a predictor of tamoxifen resistance [43, 44], and HER1 has also been linked with endocrine therapy resistance [45]. HER2 IHC was initially scored as 0/+ (negative) or ++/+++ (positive or overexpressed) [46]. Since fluorescent in situ hybridization (FISH) testing has replaced IHC as the gold standard for HER2 assessment, the P024 tumor bank was reassessed using HER1 and HER2 FISH probes, and these data on HER2 gene amplification status were supplemented with 106 tumor samples [40]. Pre- and post-treatment tumor biopsy samples were also analyzed for ER and several indices of ER function, including PgR and trefoil factor 1 (TFF1), HER1 and HER2, and the proliferation marker Ki67 [38].
-
4.
To assess gene expression profiling as a means to further investigate the transcriptional programs that underlie resistance and sensitivity to estrogen deprivation [39]. Gene expression (mRNA) profiles were collected from the tumor biopsies collected prior to surgery, at 1 month of treatment, and at surgery. The analysis was done using an Affymetrix U 133 subA Gene Chip.
-
5.
To measure aromatase expression in tumors before and after 4 months of letrozole or tamoxifen treatment. Aromatase is the key enzyme responsible for estrogen biosynthesis and is present in about 70% of tumors. IHC was performed with a monoclonal aromatase antibody (677) on trial samples prior to and following letrozole or tamoxifen treatment (n = 185); scoring was measured as a proportion of immuno-positive cells and their intensity of reactivity in malignant epithelial, stromal, adipose, and normal compartments [41].
Efficacy
In the intent-to-treat population, 154 patients received letrozole and 170 received tamoxifen. Similar proportions of patients in the letrozole and tamoxifen groups had inoperable tumors (13 and 14%, respectively). Other baseline characteristics were also well-balanced for age, race, HR status, and tumor/nodal stage of disease. More patients in the tamoxifen group (n = 41) discontinued treatment than in the letrozole arm (n = 23). The main reason for premature discontinuation was disease progression.
Clinical response and breast-conserving surgery
Letrozole was consistently superior to tamoxifen for primary and secondary efficacy end points [21]. The ORR was 55% for letrozole versus 36% for tamoxifen (P < 0.001). Median time to response was 66 days in the letrozole group and 70 days in the tamoxifen group. The odds ratio for achieving CR + PR was more than doubled with letrozole (2.23, 95% CI 1.43, 3.50; P = 0.0005). In terms of clinical progression, 12% of patients on letrozole and 17% on tamoxifen progressed, while 24% of letrozole- and 35% of tamoxifen-treated patients had stable disease. Letrozole was also shown to be significantly more effective than tamoxifen when response rates were assessed by mammography (34 vs. 16%, respectively; P < 0.001) and ultrasound (35 vs. 25%, respectively; P = 0.042).
The proportion of patients able to undergo breast-conserving surgery was significantly higher in the letrozole group than in the tamoxifen group (45 vs. 35%, respectively; P = 0.022). Of note, the odds ratio for breast-conserving surgery was 4.56 (P = 0.0001) for patients presenting with T2 tumors compared with all other T stages. The only other factor that increased the odds of undergoing breast-conserving surgery was treatment with letrozole (odds ratio 1.71, P = 0.03).
ER and PgR
A supportive analysis of clinical efficacy data conducted in patients with centrally confirmed ER+ or PgR+ tumors also showed that outcomes were significantly improved with letrozole (n = 124) compared with tamoxifen (n = 126) [37]. In this subgroup, the ORR was 60% for letrozole versus 41% for tamoxifen (P = 0.004), and breast-conserving surgery was performed in 48 versus 36%, respectively (P = 0.036).
There was a linear relationship between ER Allred expression scores and response rates to both letrozole and tamoxifen (see Fig. 2). Tumors with low ER expression were still responsive to letrozole but not to tamoxifen [37]. Of note, letrozole response rates were numerically superior to tamoxifen response rates in every ER Allred category from three to eight, indicating that letrozole is more effective than tamoxifen regardless of the level of ER expression [37]. This finding is important, because of all the AIs, only letrozole has demonstrated clear ORR superiority over tamoxifen in ER-poor tumors. When the effects of letrozole and anastrozole on tumors with low ER values (Allred scores 2–5) were compared in the neoadjuvant setting, only letrozole achieved a significant reduction in cell proliferation in ER-poor tumors [35].
Clinical response rate versus estrogen receptor (ER) Allred score for letrozole and tamoxifen. The P value for a linear logistic model was 0.0013 for letrozole and 0.0061 for tamoxifen according the Wald test. In this analysis, ER−, PgR+ cases (determined by conventional cut points) were excluded. Reprinted from [37] with permission from the American Society of Clinical Oncology
Letrozole, but not tamoxifen, significantly reduced the expression of estrogen-regulated proteins PgR and TFF1 [38]. Average tumor PgR expression decreased dramatically on letrozole treatment (P = 0.0001), and only 4.4% of surgical specimens exhibited an Allred score of between six and eight for PgR expression. The significant decrease in PgR expression with letrozole remained significant in the ER+, HER2+ subpopulation. In contrast, changes in PgR expression with tamoxifen therapy were not consistent, with both increases and decreases in expression frequently observed in the overall and ER+, HER2+ subpopulations. Analysis of changes in TFF1 produced similar conclusions, with letrozole markedly reducing expression (P = 0.0001) and tamoxifen producing no overall trend in either direction.
HER1/HER2 and response
Approximately 15% of tumors were ER+ and overexpressed both HER1 and HER2. The response rate in this patient subgroup was significantly higher with letrozole than with tamoxifen (88 vs. 21%) [37]. The odds ratio for response to letrozole versus tamoxifen was 28 (95% CI 4.5, 177; P = 0.0004). Letrozole was equally effective for HER1/HER2+ and HER1/HER2− tumors, whereas tamoxifen was significantly less effective in HER2+ compared with HER2− tumors (P = 0.045). These data suggest that although HER1 and HER2 status might not be the only explanation for the superiority of letrozole over tamoxifen, overcoming resistance pathways associated with HER1 and HER2 expression is a significant component of the improvement in outcomes associated with letrozole treatment observed in this clinical trial. FISH analysis of tumor samples confirmed the clinical efficacy of letrozole in breast cancers with or without HER2 amplification (ORR 71% in both subsets; P = 0.98). In contrast, tamoxifen-treated tumors with HER2 gene amplification had lower clinical response rates than tamoxifen-treated HER2− tumors (33 vs. 49%, P = 0.49) (see Table 2) [40].
Biomarkers of tumor proliferation
Letrozole inhibited tumor proliferation, measured by the biomarker Ki67, to a greater extent than tamoxifen (reduction in geometric mean Ki67 level 87 vs. 75%, respectively; P = 0.0009). The differences in Ki67 reduction were also observed in ER+, HER1 and/or HER2 overexpressing tumors (88% for letrozole vs. 45% for tamoxifen, respectively; P = 0.0018) [38]. Changes in the percentage of Ki67-positive cells in HER1/2+ tumors treated with letrozole or tamoxifen are shown in Fig. 3.
A box plot of before and after treatment Ki67 values in the estrogen-receptor-positive, human epidermal growth factor receptor (HER) 1/2+ subset. With letrozole (n = 15), 11 showed a decrease, one exhibited no change, and three showed an increase, of which only one was >2-fold (0.1–0.3%). With tamoxifen (n = 17), ten showed a decrease and seven an increase, of which three were relatively dramatic (9.5–22.7, 20.9–40.7, and 0.1–17.3%). Reprinted from [38] with permission from the American Association for Cancer Research
More recently, it was found that HER2 FISH-positive tumors showed higher histologic grade (P = 0.009), higher pretreatment Ki67 (P = 0.005), and less Ki67 suppression after letrozole when compared with HER2 FISH-negative tumors (P = 0.0001) [40]. Letrozole significantly decreased the geometric mean Ki67 level in HER2 FISH-negative tumors (from 6.25 [95% CI 5.16, 7.58%] to 0.68% [95% CI 0.53, 0.87%]; P = 0.0001), but the decrease in HER2 FISH-positive tumors was blunted (from 14.73 [95% CI 9.67, 22.44%] to 8.1% [95% CI 4.16, 15.75%]; not significant). A similar observation for Ki67 was made in a smaller cohort of tamoxifen-treated tumors [40].
The relationship between cell cycle CR, defined as ≤1% of post-treatment Ki67 staining in the infiltrating component of the tumor, and HER2 status of tumors treated with letrozole was also analyzed [40]. Significantly more HER2 FISH-negative than FISH-positive tumors met the definition of a cell cycle CR at the time of surgery (60 vs. 12%; P = 0.0001). There was a high level of correlation between lack of cell cycle CR and the presence of a positive HER2 FISH test (P = 0.0001) for letrozole- and tamoxifen-treated tumors, which is consistent with the conclusion that HER2 gene amplification generates resistance at the level of cell cycle progression regardless of which endocrine therapy is used [40].
These biomarker findings are discordant with clinical observations that tumor regression is unaffected by HER2 amplification status in patients treated with neoadjuvant letrozole and may imply therapeutic resistance that could manifest later in the clinical course of the disease. Consistent with this finding, Miller and colleagues also reported that neoadjuvant letrozole produces rapid and profound decreases in expression of Ki67 and PgR that do not always correlate with clinical and pathological responses [47].
Gene expression profiling
Preliminary gene expression profiling analysis of biopsies taken pretreatment and 1 month post letrozole treatment showed down-regulation of genes involved in DNA replication and synthesis, cell cycle progression, apoptosis suppression, and tissue invasion [39]. These results illustrate the molecular basis for estrogen-deprivation letrozole therapy which may be useful in the development of predictive models of ER+ breast cancer.
Aromatase
Sufficient pre- and post-treatment tumor material was available from 171 cases (81 on letrozole and 90 on tamoxifen) from the P024 trial for immunohistochemistry analysis of aromatase protein expression [41]. Aromatase was detected in all tumor compartments, with the strongest staining observed in malignant epithelial cells. Median aromatase values did not change significantly with letrozole or tamoxifen treatment; however, changes in score did occur in individual cases, with more noticeable effects observed in letrozole-treated patients [41]. A positive correlation existed between baseline ER and aromatase staining in cancer cells, while a negative correlation was observed between baseline Ki67 and aromatase expression in cancer plus stroma. Baseline aromatase expression did not predict response to letrozole or tamoxifen, or changes in Ki67 induced by treatment. However, negative staining in both stroma and cancer after treatment was strongly associated with fewer cell cycle CR and smaller Ki67 declines with letrozole (but not tamoxifen) treatment [48].
Safety and duration of therapy
P024 demonstrated that letrozole is well-tolerated in the neoadjuvant setting [21]. There were no major tolerability differences between letrozole and tamoxifen, and adverse effects of a similar nature were seen in 57% of patients in each arm [21]. The most common treatment-related adverse event was hot flushes, occurring in 20% of patients in the letrozole group and 24% of patients in the tamoxifen group.
The excellent tolerability, predictable pharmacokinetics, and minimal drug–drug interactions [49, 50] make letrozole a particularly suitable option for older women unable to tolerate or unwilling to accept neoadjuvant chemotherapy and in whom the presence of comorbidities and use of concomitant therapies complicate treatment selection [20]. The median age of patients in P024 treated with letrozole was 68 years, and 46% of patients were at least 70 years old. The feasibility and safety of letrozole was also reported recently from another trial using letrozole as primary systemic therapy in elderly patients (median age 79 years) with breast cancer [51]. In addition, letrozole has been successfully administered to elderly patients (median age of the elderly subgroup 75 years; range 70–96 years) in the advanced breast cancer setting [52].
The favorable safety profile of letrozole also allows for the extension of the neoadjuvant treatment beyond the 4 months used in the P024 trial. In a recent study, 33 postmenopausal women with HR+ breast cancer ineligible for breast-conserving surgery were treated with letrozole for 4 months. Continued administration of letrozole for a further 4 months in responders and patients with stable disease resulted in a statistically significant improvement in tumor size reduction (P = 0.039); ORR was 90% in patients receiving preoperative treatment for longer than 4 months compared with 57% in patients receiving treatment up to 4 months [53].
In another study, 42 patients who were unsuitable for breast-conserving surgery or had refused surgery after responding to initial neoadjuvant therapy with letrozole for 3 months benefited from continuing tumor volume reduction during further letrozole treatment administered for up to 12 months [54]. The median reductions in tumor volume were 52% (95% CI 37, 62) from 0 to 3 months, 57% (95% CI 26, 100) from 3 to 6 months, and 66% (95% CI 22, 100) from 6 to 12 months. Extending the duration of letrozole also improved the CR rate, which increased from 4/42 patients (9.5%) at 3 months to 12/42 (29%) by 6 months and 8/22 (36%) by 12 months.
Conclusions
Neoadjuvant therapy with AIs is a safe and effective treatment option for postmenopausal women who are unwilling or unable to undergo surgery or preoperative chemotherapy [21, 22, 55–57]. Letrozole is significantly more effective than tamoxifen in the neoadjuvant setting in terms of ORR and increased rate of breast-conserving surgery [21, 55].
One of the advantages of using a neoadjuvant strategy is the opportunity to gain information on tumor response early in the course of treatment. Detailed studies correlating clinical response to neoadjuvant therapy with changes in tumor biomarkers and gene expression may ultimately prove useful to tailor therapy for individual patients and to gain a better understanding of the biology of HR+ breast cancer. Correlative studies conducted using tumor samples from P024 have revealed important information about how breast tumors respond to letrozole [37–40]. Letrozole was shown to be significantly more effective than tamoxifen in the inhibition of ER+ tumor proliferation, since letrozole produced a greater reduction in levels of the proliferation biomarker Ki67 [38]. It has been suggested that a greater suppression in proliferation could lead to greater long-term survival in the adjuvant setting. Preliminary data from the Immediate Preoperative Anastrozole Tamoxifen or Combined with Tamoxifen trial have indicated that short-term changes in Ki67 levels, after 2 and 12 weeks, may be a useful predictive marker for relapse-free survival in patients treated with neoadjuvant AI therapy [58]. It has also been suggested that changes in proliferation and concurrent changes in apoptosis may be expected to be more predictive of adjuvant benefit from endocrine therapy than clinical response [59].
Correlative studies have also highlighted the complexity of breast cancer biology and revealed discordance between clinical and biomarker responses [40]. Amplification of HER2 was shown to be associated with a more aggressive breast cancer phenotype and greater resistance to tamoxifen [37, 40]. Clinical response data from the P024 trial have shown that letrozole is equally effective in HER2+ and HER2− tumors, whereas tamoxifen is less effective in HER2+ tumors [37]. These data suggest that letrozole could be a superior option to tamoxifen for postmenopausal women with HER2+, HR+ tumors [37]. However, analysis of proliferation markers has provided evidence of estrogen-independent proliferation of ER+, HER2+ breast cancer despite neoadjuvant letrozole [40]. It appears that cell-cycle regulation is partially or completely estrogen-independent in the majority of primary tumors showing HER2 gene amplification, and patients with such tumors may eventually develop resistance to adjuvant AI therapy. Novel strategies to delay or overcome hormone resistance are described elsewhere in this supplement, in the article, “Femara and the future.”
Gene expression profiling has demonstrated that letrozole targets genes responsible for DNA replication and synthesis, cell cycle progression, apoptosis, and tissue invasion [39]. Research into genetic profiling is continuing, with the aim of developing clinically relevant predictive models that can accurately classify ER+ disease according to likely response to specific neoadjuvant therapies. Predictive models will improve treatment individualization and help to avoid unnecessary treatment-related toxicity in patients unlikely to benefit from systemic therapies [17, 60].
The P024 trial has clearly demonstrated the therapeutic superiority of letrozole over tamoxifen for the neoadjuvant management of primary breast cancer. The trial has also provided the oncology community with a validated research setting within which to gain valuable insights into the molecular features of ER+ breast cancer and its treatment that will help shape new therapies in the years to come.
References
NIH (1992) Consensus development conference on the statement: treatment of early-stage breast cancer. Bethesda, Maryland, 18–21 June 1990. J Natl Cancer Inst Monogr 11:1–15
Carlson RW, Brown E, Burstein HJ, Gradishar WJ, Hudis CA, Loprinzi C, Mamounas EP, Perez EA, Pritchard K, Ravdin P, Recht A, Somlo G, Theriault RL, Winer EP, Wolff AC (2006) National Comprehensive Cancer Network. NCCN Task Force Report: adjuvant therapy for breast cancer. J Natl Compr Canc Netw 4(suppl 1):S1–26
Fisher B, Bryant J, Wolmark N, Mamounas E, Brown A, Fisher ER, Wickerham DL, Begovic M, DeCillis A, Robidoux A, Margolese RG, Cruz AB Jr, Hoehn JL, Lees AW, Dimitrov NV, Bear HD (1998) Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J Clin Oncol 16:2672–2685
Bear HD, Anderson S, Smith RE, Geyer CE Jr, Mamounas EP, Fisher B, Brown AM, Robidoux A, Margolese R, Kahlenberg MS, Paik S, Soran A, Wickerham DL, Wolmark N (2006) Sequential preoperative or postoperative docetaxel added to preoperative doxorubicin plus cyclophosphamide for operable breast cancer: National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol 24:2019–2027
Mauriac L, Durand M, Avril A, Dilhuydy JM (1991) Effects of primary chemotherapy in conservative treatment of breast cancer patients with operable tumors larger than 3 cm. Results of a randomized trial in a single centre. Ann Oncol 2:347–354
Chen AM, Meric-Bernstam F, Hunt KK, Thames HD, Oswald MJ, Outlaw ED, Strom EA, McNeese MD, Kuerer HM, Ross MI, Singletary SE, Ames FC, Feig BW, Sahin AA, Perkins GH, Schechter NR, Hortobagyi GN, Buchholz TA (2004) Breast conservation after neoadjuvant chemotherapy: the MD Anderson Cancer Center experience. J Clin Oncol 22:2303–2312
Boughey JC, Peintinger F, Meric-Bernstam F, Perry AC, Hunt KK, Babiera GV, Singletary SE, Bedrosian I, Lucci A, Buzdar AU, Pusztai L, Kuerer HM (2006) Impact of preoperative versus postoperative chemotherapy on the extent and number of surgical procedures in patients treated in randomized clinical trials for breast cancer. Ann Surg 244:464–470
Kaufmann M, Hortobagyi GN, Goldhirsch A, Scholl S, Makris A, Valagussa P, Blohmer JU, Eiermann W, Jackesz R, Jonat W, Lebeau A, Loibl S, Miller W, Seeber S, Semiglazov V, Smith R, Souchon R, Stearns V, Untch M, von Minckwitz G (2006) Recommendations from an international expert panel on the use of neoadjuvant (primary) systemic treatment of operable breast cancer: an update. J Clin Oncol 24:1940–1949. Erratum in: J Clin Oncol 2006;24:3221
Rouzier R, Pusztai L, Delaloge S, Gonzalez-Angulo AM, Andre F, Hess KR, Buzdar AU, Garbay JR, Spielmann M, Mathieu MC, Symmans WF, Wagner P, Atallah D, Valero V, Berry DA, Hortobagyi GN (2005) Nomograms to predict pathologic complete response and metastasis-free survival after preoperative chemotherapy for breast cancer. J Clin Oncol 23:8331–8339
Ross JS, Linette GP, Stec J, Clark E, Ayers M, Leschly N, Symmans WF, Hortobagyi GN, Pusztai L (2003) Breast cancer biomarkers and molecular medicine, part I. Expert Rev Mol Diagn 3:573–585
Bast RC Jr, Ravdin P, Hayes DF, Bates S, Fritsche H Jr, Jessup JM, Kemeny N, Locker GY, Mennel RG, Somerfield MR; American Society of Clinical Oncology Tumor Markers Expert Panel (2001) 2000 update of recommendations for the use of tumor markers in breast and colorectal cancer: clinical practice guidelines of the American Society of Clinical Oncology. J Clin Oncol 19:1865–1878. Erratum in: J Clin Oncol 2001;19:4185–4188 and J Clin Oncol 2002;20:2213
von Minckwitz G, Raab G, Caputo A, Schutte M, Hilfrich J, Blohmer JU, Gerber B, Costa SD, Merkle E, Eidtmann H, Lampe D, Jackisch C, du Bois A, Kaufmann M (2005) Doxorubicin with cyclophosphamide followed by docetaxel every 21 days compared with doxorubicin and docetaxel every 14 days as preoperative treatment in operable breast cancer: the GEPARDUO study of the German Breast Group. J Clin Oncol 23:2676–2685
von Minckwitz G, Blohmer JU, Raab G, Lohr A, Gerber B, Heinrich G, Eidtmann H, Kaufmann M, Hilfrich J, Jackisch C, Zuna I, Costa SD; German Breast Group (2005) In vivo chemosensitivity-adapted preoperative chemotherapy in patients with early-stage breast cancer: the GEPARTRIO pilot study. Ann Oncol 16:56–63
Gianni L, Baselga J, Eiermann W, Guillem Porta V, Semiglazov V, Lluch A, Zambetti M, Sabadell D, Raab G, Llombart Cussac A, Bozhok A, Martinez-Agullo A, Greco M, Byakhov M, Lopez Lopez JJ, Mansutti M, Valagussa P, Bonadonna G, European Cooperative Trial in Operable Breast Cancer Study Group (2005) Feasibility and tolerability of sequential doxorubicin/paclitaxel followed by cyclophosphamide, methotrexate, and fluorouracil and its effects on tumor response as preoperative therapy. Clin Cancer Res 11(24 Pt 1):8715–8721
Colleoni M, Viale G, Zahrieh D, Pruneri G, Gentilini O, Veronesi P, Gelber RD, Curigliano G, Torrisi R, Luini A, Intra M, Galimberti V, Renne G, Nole F, Peruzzotti G, Goldhirsch A (2004) Chemotherapy is more effective in patients with breast cancer not expressing steroid hormone receptors: a study of preoperative treatment. Clin Cancer Res 10:6622–6628
Hess KR, Anderson K, Symmans WF, Valero V, Ibrahim N, Mejia JA, Booser D, Theriault RL, Buzdar AU, Dempsey PJ, Rouzier R, Sneige N, Ross JS, Vidaurre T, Gomez HL, Hortobagyi GN, Pusztai L (2006) Pharmacogenomic predictor of sensitivity to preoperative chemotherapy with paclitaxel and fluorouracil, doxorubicin, and cyclophosphamide in breast cancer. J Clin Oncol 24:4236–4244
Rouzier R, Perou CM, Symmans WF, Ibrahim N, Cristofanilli M, Anderson K, Hess KR, Stec J, Ayers M, Wagner P, Morandi P, Fan C, Rabiul I, Ross JS, Hortobagyi GN, Pusztai L (2005) Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res 11:5678–5685
Crivellari D, Bonetti M, Castiglione-Gertsch M, Gelber RD, Rudenstam CM, Thurlimann B, Price KN, Coates AS, Hurny C, Bernhard J, Lindtner J, Collins J, Senn HJ, Cavalli F, Forbes J, Gudgeon A, Simoncini E, Cortes-Funes H, Veronesi A, Fey M, Goldhirsch A (2000) Burdens and benefits of adjuvant cyclophosphamide, methotrexate, and fluorouracil and tamoxifen for elderly patients with breast cancer: the International Breast Cancer Study Group trial VII. J Clin Oncol 18:1412–1422
Doyle JJ, Neugut AI, Jacobson JS, Grann VR, Hershman DL (2005) Chemotherapy and cardiotoxicity in older breast cancer patients: a population-based study. J Clin Oncol 23:8597–8605
Balducci L, Yates J (2000) General guidelines for the management of older patients with cancer. Oncology (Williston Park) 14:221–227
Eiermann W, Paepke S, Appfelstaedt J, Llombart-Cussac A, Eremin J, Vinholes J, Mauriac L, Ellis M, Lassus M, Chaudri-Ross HA, Dugan M, Borgs M, Letrozole Neo-Adjuvant Breast Cancer Study Group (2001) Preoperative treatment of postmenopausal breast cancer patients with letrozole: a randomized double-blind multicenter study. Ann Oncol 12:1527–1532
Smith IE, Dowsett M, Ebbs SR, Dixon JM, Skene A, Blohmer JU, Ashley SE, Francis S, Boeddinghaus I, Walsh G, IMPACT Trialists Group (2005) Neoadjuvant treatment of postmenopausal breast cancer with anastrozole, tamoxifen, or both in combination: the immediate preoperative anastrozole, tamoxifen, or combined with tamoxifen (IMPACT) multicenter double-blind randomized trial. J Clin Oncol 23:5108–5116
Mustacchi G, Ceccherini R, Milani S, Pluchinotta A, De Matteis A, Maiorino L, Farris A, Scanni A, Sasso F, Italian Cooperative Group GRETA (2003) Tamoxifen alone versus adjuvant tamoxifen for operable breast cancer of the elderly: long-term results of the phase III randomized controlled multicenter GRETA trial. Ann Oncol 14:414–420
Semiglazov V, Ivanov V, Bozhok A, Kletzel A, Ziltzova E, Melnikova O, Paltuev R, Dashyan G, Berstein L, Petrov NN (2005) Direct comparison of primary (neoadjuvant) endocrine therapy vs primary chemotherapy in postmenopausal women with ER-positive breast cancer. Breast 14(suppl 1):S39. Abstract P85
Bates T, Riley DL, Houghton J, Fallowfield L, Baum M (1991) Breast cancer in elderly women: a Cancer Research Campaign trial comparing treatment with tamoxifen and optimal surgery with tamoxifen alone. The Elderly Breast Cancer Working Party. Br J Surg 78:591–594
Robertson JF, Ellis IO, Elston CW, Blamey RW (1992) Mastectomy or tamoxifen as initial therapy for operable breast cancer in elderly patients: 5-year follow-up. Eur J Cancer 28A(4–5):908–910
Gazet JC, Ford HT, Coombes RC, Bland JM, Sutcliffe R, Quilliam J, Lowndes S (1994) Prospective randomized trial of tamoxifen vs surgery in elderly patients with breast cancer. Eur J Surg Oncol 20:207–214
Fennessy M, Bates T, MacRae K, Riley D, Houghton J, Baum M (2004) Late follow-up of a randomized trial of surgery plus tamoxifen versus tamoxifen alone in women aged over 70 years with operable breast cancer. Br J Surg 91:699–704
Hind D, Wyld L, Beverley CB, Reed MW (2006) Surgery versus primary endocrine therapy for operable primary breast cancer in elderly women (70 years plus). Cochrane Database Syst Rev 1:CD004272
Fisher B, Costantino JP, Redmond CK, Fisher ER, Wickerham DL, Cronin WM (1994) Endometrial cancer in tamoxifen-treated breast cancer patients: findings from the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-14. J Natl Cancer Inst 86:527–537
Lu Q, Yue W, Wang J, Liu Y, Long B, Brodie A (1998) The effects of aromatase inhibitors and antiestrogens in the nude mouse model. Breast Cancer Res Treat 50:63–71
Mouridsen H, Gershanovich M, Sun Y, Perez-Carrion R, Boni C, Monnier A, Apffelstaedt J, Smith R, Sleeboom HP, Janicke F, Pluzanska A, Dank M, Becquart D, Bapsy PP, Salminen E, Snyder R, Lassus M, Verbeek JA, Staffler B, Chaudri-Ross HA, Dugan M (2001) Superior efficacy of letrozole versus tamoxifen as first-line therapy for postmenopausal women with advanced breast cancer: results of a phase III study of the International Letrozole Breast Cancer Group. J Clin Oncol 2001;19:2596–2606. Erratum in: J Clin Oncol 2001;19:3302
Haynes BP, Dowsett M, Miller WR, Dixon JM, Bhatnagar AS (2003) The pharmacology of letrozole. J Steroid Biochem Mol Biol 87:35–45
Geisler J, Haynes B, Anker G, Dowsett M, Lonning PE (2002) Influence of letrozole and anastrozole on total body aromatization and plasma estrogen levels in postmenopausal breast cancer patients evaluated in a randomized, cross-over study. J Clin Oncol 20:751–757
Murray J, Young O, Renshaw L, White S, Prescot RJ, Krause A, Evans DB, Salem R, Cameron D, Dowsett M, Miller WR, Dixon JM (2004) Letrozole and anastrozole: a pre-operative study of their effects on ER positive breast cancers in postmenopausal women. Presented at the 27th Annual San Antonio Breast Cancer Symposium, 8–11 December 2004. Abstract 406
Dixon JM, Love CD, Bellamy CO, Cameron DA, Leonard RC, Smith H, Miller WR (2001) Letrozole as primary medical therapy for locally advanced and large operable breast cancer. Breast Cancer Res Treat 66:191–199
Ellis MJ, Coop A, Singh B, Mauriac L, Llombert-Cussac A, Janicke F, Miller WR, Evans DB, Dugan M, Brady C, Quebe-Fehling E, Borgs M (2001) Letrozole is more effective neoadjuvant endocrine therapy than tamoxifen for ErbB-1- and/or ErbB-2-positive, estrogen receptor-positive primary breast cancer: evidence from a phase III randomized trial. J Clin Oncol 19:3808–3816
Ellis MJ, Coop A, Singh B, Tao Y, Llombart-Cussac A, Janicke F, Mauriac L, Quebe-Fehling E, Chaudri-Ross HA, Evans DB, Miller WR (2003) Letrozole inhibits tumor proliferation more effectively than tamoxifen independent of HER1/2 expression status. Cancer Res 63:6523–6531
Ellis MJ, Rosen E, Dressman H, Marks J (2003) Neoadjuvant comparisons of aromatase inhibitors and tamoxifen: pretreatment determinants of response and on-treatment effect. J Steroid Biochem Mol Biol 86:301–307
Ellis MJ, Tao Y, Young O, White S, Proia AD, Murray J, Renshaw L, Faratian D, Thomas J, Dowsett M, Krause A, Evans DB, Miller WR, Dixon JM (2006) Estrogen-independent proliferation is present in estrogen-receptor HER2-positive primary breast cancer after neoadjuvant letrozole. J Clin Oncol 24:3019–3025
Miller W, Tao Y, Ellis M, Bhatnagar A, Evans D, Sasano H (2006) Tumour aromatase as measured by immunohistochemistry in patients treated neoadjuvantly with either letrozole or tamoxifen in the P024 randomised trial—correlations with other biomarkers. Eur J Cancer Suppl 4:143. Abstract 326
Allred DC, Harvey JM, Berardo M, Clark GM (1998) Prognostic and predictive factors in breast cancer by immunohistochemical analysis. Mod Pathol 11:155–168
Carlomagno C, Perrone F, Gallo C, De Laurentiis M, Lauria R, Morabito A, Pettinato G, Panico L, D’Antonio A, Bianco AR, De Placido S (1996) c-erb B2 overexpression decreases the benefit of adjuvant tamoxifen in early-stage breast cancer without axillary lymph node metastases. J Clin Oncol 14:2702–2708
De Laurentiis M, Arpino G, Massarelli E, Ruggiero A, Carlomagno C, Ciardiello F, Tortora G, D’Agostino D, Caputo F, Cancello G, Montagna E, Malorni L, Zinno L, Lauria R, Bianco AR, De Placido S (2005) A meta-analysis on the interaction between HER-2 expression and response to endocrine treatment in advanced breast cancer. Clin Cancer Res 11:4741–4748
Newby JC, Johnston SR, Smith IE, Dowsett M (1997) Expression of epidermal growth factor receptor and c-erbB2 during the development of tamoxifen resistance in human breast cancer. Clin Cancer Res 3:1643–1651
Jacobs TW, Gown AM, Yaziji H, Barnes MJ, Schnitt SJ (1999) Specificity of HercepTest in determining HER-2/neu status of breast cancers using the United States food and drug administration-approved scoring system. J Clin Oncol 17:1983–1987
Miller WR, White S, Dixon JM, Murray J, Renshaw L, Anderson TJ (2006) Proliferation, steroid receptors and clinical/pathological response in breast cancer treated with letrozole. Br J Cancer 94:1051–1056
Miller WR, Ellis MJ, Tao Y, Bhatnagar A, Evans DB, Sasano H (2006) Absence of post treatment tumor expression of aromatase is associated with reduced antiproliferative effects of letrozole (but not tamoxifen) in the P024 adjuvant endocrine therapy trial. Breast Cancer Res Treat 100(suppl 1):S186
Pfister CU, Martoni A, Zamagni C, Lelli G, De Braud F, Souppart C, Duval M, Hornberger U (2001) Effect of age and single versus multiple dose pharmacokinetics of letrozole (Femara) in breast cancer patients. Biopharm Drug Dispos 22:191–197
Femara prescribing information (2005) Novartis
Bottini A, Generali D, Brizzi MP, Fox SB, Bersiga A, Bonardi S, Allevi G, Aguggini S, Bodini G, Milani M, Dionisio R, Bernardi C, Montruccoli A, Bruzzi P, Harris AL, Dogliotti L, Berruti A (2006) Randomized phase II trial of letrozole and letrozole plus low-dose metronomic oral cyclophosphamide as primary systemic treatment in elderly breast cancer patients. J Clin Oncol 24:3623–3628
Mouridsen H, Chaudri-Ross HA (2004) Efficacy of first-line letrozole versus tamoxifen as a function of age in postmenopausal women with advanced breast cancer. Oncologist 9:497–506
Paepke S, Tulusan A, Kiesel L, Bastert G, Jaenicke FK, Bouterfa H, Wackwitz B, Wallwiener D (2003) A multi-center study of pre-operative treatment with letrozole for optimal duration of treatment in postmenopausal women with ER and/or PGR positive breast cancer. Proc Am Soc Clin Oncol 22:2003. Abstract 321
Renshaw L, Murray J, Young O, Cameron D, Miller WR, Dixon JM (2004) Is there an optimal duration of neoadjuvant letrozole therapy? Presented at the 27th Annual San Antonio Breast Cancer Symposium, 8–11 December 2004. Abstract 405
Llombart A, Galán A, Fuster C, Buch E, Carañana V, Rodríguez-Lescure A, Vázquez C, Guerrero A, Ruiz A, Guillam-Porta V (2006) Phase II trial with letrozole (2.5 mg) to maximal response as neoadjuvant endocrine therapy in postmenopausal patients with ER/PgR[+] operable breast cancer. Eur J Cancer Suppl 4:153. Abstract 362
Semiglazov V, Kletsel A, Semiglazov V, Zhiltzova E, Ivanov V, Dashyan G, Bozhok A, Melnikova O, Paltuev R, Berstein L (2005) Exemestane (E) vs tamoxifen (T) as neoadjuvant endocrine therapy for postmenopausal women with ER+ breast cancer (T2N1-2, T3N0-1, T4N0M0) J Clin Oncol 23(16S):11S. Abstract 530
Cataliotti L, Buzdar AU, Noguchi S, Bines J, Takatsuka Y, Petrakova K, Dube P, de Oliveira CT (2006) Comparison of anastrozole versus tamoxifen as preoperative therapy in postmenopausal women with hormone receptor-positive breast cancer: the Pre-Operative “Arimidex” Compared to Tamoxifen (PROACT) trial. Cancer 15(106):2095–2103
Dowsett M, Ebbs SR, Dixon JM, Skene A, Griffith C, Boeddinghaus I, Salter J, Detre S, Hills M, Ashley S, Francis S, Walsh G, Smith IE (2005) Biomarker changes during neoadjuvant anastrozole, tamoxifen, or the combination: influence of hormonal status and HER-2 in breast cancer—a study from the IMPACT trialists. J Clin Oncol 23:2477–2492
Dowsett M, Smith IE, Ebbs SR, Dixon JM, Skene A, Griffith C, Boeddinghaus I, Salter J, Detre S, Hills M, Ashley S, Francis S, Walsh G, A’Hern R (2006) Proliferation and apoptosis as markers of benefit in neoadjuvant endocrine therapy of breast cancer. Clin Cancer Res 12(3 Pt 2):1024s–1030s
Pawitan Y, Bjohle J, Amler L, Borg AL, Egyhazi S, Hall P, Han X, Holmberg L, Huang F, Klaar S, Liu ET, Miller L, Nordgren H, Ploner A, Sandelin K, Shaw PM, Smeds J, Skoog L, Wedren S, Bergh J (2005) Gene expression profiling spares early breast cancer patients from adjuvant therapy: derived and validated in two population-based cohorts. Breast Cancer Res 7:R953–R964
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s10549-007-9850-y
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 2.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by-nc/2.0/.
About this article
Cite this article
Ellis, M.J., Ma, C. Letrozole in the neoadjuvant setting: the P024 trial. Breast Cancer Res Treat 105 (Suppl 1), 33–43 (2007). https://doi.org/10.1007/s10549-007-9701-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-007-9701-x