Abstract
Background: Historically, patients with thick (≥4 mm) primary melanoma have not been considered candidates for elective lymph node dissection, because their risk for occult distant disease is significant. Sentinel lymph node (SLN) biopsy offers an alternative approach to assess disease in the regional nodal basin, but no studies have specifically addressed the role for this technique in patients with thick melanoma. Although adjuvant therapy benefits patients who develop nodal metastases, data that supports its routine use in all patients with thick melanoma is both limited and controversial. This study was performed to determine whether pathological status of the SLN is an important risk factor in this heterogeneous group and, thus, provides a rationale for SLN biopsy.
Methods: The records of 131 patients with primary cutaneous melanoma whose primary tumors were at least 4 mm thick and who underwent lymphatic mapping and SLN biopsy were reviewed. Several known prognostic factors, i.e., tumor thickness, ulceration, Clark level, location, sex, as well as SLN pathological status were analyzed with respect to disease-free and overall survival.
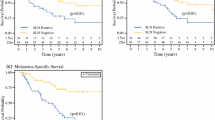
Results: Lymphatic mapping and SLN biopsy was successful in 126 (96%) of 131 patients who underwent the procedure. In 49 patients (39%), the SLN biopsy was positive by conventional histology, although it was negative in 77 patients (61%). The median follow-up was 3 years. Although presence of ulceration and SLN status were independent prognostic factors with respect to disease-free and overall survival, SLN status was the most powerful predictor of overall survival by univariate and multivariate analyses.
Conclusions: Lymphatic mapping and SLN biopsy is a highly accurate method of staging lymph node basins at risk for regional metastases in patients with thick melanoma and identifies those patients who may benefit from earlier lymphadenectomy as well as patients with a more favorable prognosis. Pathological status of the SLN in these patients with clinically negative nodes is the most important prognostic factor for survival and is essential to establish stratification criteria for future adjuvant trials in this high-risk group.
Similar content being viewed by others
References
Reintgen D., Rapaport D., Tanabe K., Ross M. Lymphatic mapping and sentinel lymphadenectomy. In: Balch C., Houghton A., Sober A., Soong S-j, eds. Cutaneous Melanoma. St. Louis: Quality Medical Publishing, 1997:239.
Gershenwald J., Thompson W., Mansfield P, et al. Multi-institutional lymphatic mapping experience: the prognostic value of sentinel lymph node status in 612 stage I or II melanoma patients. J Clin Oncol 1999;17:976–983.
Gershenwald J., Tseng C-h, Thompson W, et al. Improved sentinel lymph node localization in primary melanoma patients with the use of radiolabeled colloid. Surgery 1998;124:203–210.
Balch C., Urist M., Karakousis C, et al. Efficacy of 2-cm surgical margins for intermediate-thickness melanomas (1 to 4 mm): results of a multi-institutional randomized surgical trial. Ann Surg 1993;218:262–267.
Veronesi U., Cascinelli N. Narrow excision (1-cm margin): a safe procedure for thin cutaneous melanoma. Arch Surg 1991;126:438–441.
Gershenwald J., Thompson W., Mansfield P, et al. Patterns of recurrence following a negative sentinel lymph node biopsy in 243 patients with stage I or II melanoma. J Clin Oncol 1998;16:2253–2260.
Coit D., Sauven P., Brennan M. Prognosis of thick cutaneous melanoma of the trunk and extremity. Arch Surg 1990;125:322–326.
Kim S., Garcia C., Rodriguez J., Coit D. Prognosis of thick cutaneous melanoma. J Am Coll Surg 1999;188:241–247.
Heaton K., Sussman J., Gershenwald J, et al. Surgical margins and prognostic factors in patients with thick (>4 mm) primary melanoma. Ann Surg Oncol 1998;5:322–328.
Schneebaum S., Briele H., Walker M, et al. Cutaneous thick melanoma: prognosis and treatment. Arch Surg 1987;122:707–711.
Kirkwood J., Strawderman M., Ernstoff M, et al. Interferon-alfa-2b adjuvant therapy of high-risk resected cutaneous melanoma: the Eastern Cooperative Oncology Group Trial EST 1684. J Clin Oncol 1996;14:7–17.
Morton D., Wen D., Wong J, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 1992;127:392–399.
Albertini J., Cruse C., Rapaport D, et al. Intraoperative adiolymphoscintigraphy improves sentinel lymph node identification for patients with melanoma. Ann Surg 1996;223:217–224.
Thompson J., McCarthy W., Bosch C, et al. Sentinel lymph node status as an indicator of the presence of metastatic melanoma in regional lymph nodes. Melanoma Res 1995;5:255–260.
Slingluff JCL., Stidham K., Ricci W, et al. Surgical management of regional lymph nodes in patients with melanoma. Ann Surg 1994;219:120–130.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Gershenwald, J.E., Mansfield, P.F., Lee, J.E. et al. Role for Lymphatic Mapping and Sentinel Lymph Node Biopsy in Patients With Thick (≥4 mm) Primary Melanoma. Ann Surg Oncol 7, 160–165 (2000). https://doi.org/10.1007/s10434-000-0160-4
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10434-000-0160-4