Abstract
Objectives
To correlate the decrease in background parenchymal enhancement (BPE) and tumour response measured with MRI in breast cancer patients treated with neoadjuvant chemotherapy (NAC).
Methods
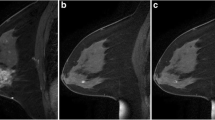
One hundred and forty-six MRI examinations of 73 patients with 80 biopsy-proven breast cancers who underwent breast MRI before and after NAC were retrospectively analysed. All images were reviewed by two blinded readers, who classified BPE into categories (BEC; 1 = minimal, 2 = mild, 3 = moderate, 4 = marked) before and after NAC. Histopathological and morphological tumour responses were analysed and compared.
Results
The distribution of BEC 1/2/3/4 was 25/46/18/11 % before and 78/20/2/0 % after NAC. On average, BPE decreased by 0.87 BEC. Cohen’s kappa showed substantial agreement (k = 0.73–0.77) before and moderate agreement (k = 0.43–0.60) after NAC and moderate agreement (k = 0.62–0.60) concerning the change in BEC. Correlating the change in BPE with tumour response, the average decrease in BEC was 1.3 in cases of complete remission, 0.83 in cases with partial response, 0.85 in cases with stable disease and 0.40 in cases with progressive disease. Correlation analysis showed a significant correlation between the decrease in BEC and tumour response (r = −0.24, p = 0.03).
Conclusions
BPE decreased by, on average, 0.87 BEC following NAC for breast cancer. The degree of BPE reduction seemed to correlate with tumour response.
Key Points
• BPE decreases by an average of 0.87 categories under neoadjuvant chemotherapy.
• The reduction of BPE following neoadjuvant chemotherapy correlates with the tumour response.
• The classification of the BPE shows good agreement among trained readers.




Similar content being viewed by others
References
Morris E, Comstock C, Lee C, et al (2013) Magnetic Resonance Imaging. In: ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System. Reston, VA, American College of Radiology
Hansen NL, Kuhl CK, Barabasch A, Strobel K, Schrading S (2014) Does MRI Breast “Density” (Degree of Background Enhancement) Correlate With Mammographic Breast Density? J Magn Reson Imaging 40:483–489
Cubuk R, Tasali N, Narin B, Keskiner F, Celik L, Guney S (2010) Correlation between breast density in mammography and background enhancement in MR mammography. Radiol Med 115:434–441
King V, Gu Y, Kaplan JB, Brooks JD, Pike MC, Morris EA (2012) Impact of menopausal status on background parenchymal enhancement and fibroglandular tissue on breast MRI. Eur Radiol 22:2641–2647
Muller-Schimpfle M, Ohmenhauser K, Stoll P, Dietz K, Claussen CD (1997) Menstrual cycle and age: influence on parenchymal contrast medium enhancement in MR imaging of the breast. Radiology 203:145–149
Kuhl CK, Bieling HB, Gieseke J et al (1997) Healthy premenopausal breast parenchyma in dynamic contrast-enhanced MR imaging of the breast: normal contrast medium enhancement and cyclical-phase dependency. Radiology 203:137–144
Baek JE, Kim SH, Lee AW (2014) Background parenchymal enhancement in breast MRIs of breast cancer patients: Impact on tumor size estimation. Eur J Radiol 83:1356–1362
Uematsu T, Kasami M, Watanabe J (2011) Does the degree of background enhancement in breast MRI affect the detection and staging of breast cancer? Eur Radiol 21:2261–2267
Park SY, Kang DK, Kim TH (2015) Does background parenchymal enhancement on MRI affect the rate of positive resection margin in breast cancer patients? Br J Radiol 88:20140638
Kim JY, Kim SH, Kim YJ et al (2015) Enhancement parameters on dynamic contrast enhanced breast MRI: do they correlate with prognostic factors and subtypes of breast cancers? Magn Reson Imaging 33:72–80
Kim S-A, Cho N, Ryu EB et al (2013) Background Parenchymal Signal Enhancement Ratio at Preoperative MR Imaging: Association with Subsequent Local Recurrence in Patients with Ductal Carcinoma in Situ after Breast Conservation Surgery. Radiology 270:699–707
DeLeo MJ 3rd, Domchek SM, Kontos D, Conant E, Chen J, Weinstein S (2015) Breast MRI fibroglandular volume and parenchymal enhancement in BRCA1 and BRCA2 mutation carriers before and immediately after risk-reducing salpingo-oophorectomy. AJR Am J Roentgenol 204:669–673
Kim YJ, Kim SH, Choi BG et al (2014) Impact of radiotherapy on background parenchymal enhancement in breast magnetic resonance imaging. Asian Pac J Cancer Prev 15:2939–2943
Chen JH, Yu HJ, Hsu C, Mehta RS, Carpenter PM, Su MY (2015) Background Parenchymal Enhancement of the Contralateral Normal Breast: Association with Tumor Response in Breast Cancer Patients Receiving Neoadjuvant Chemotherapy. Transl Oncol 8:204–209
Schrading S, Kuhl CK (2015) Breast Cancer: Influence of Taxanes on Response Assessment with Dynamic Contrast-enhanced MR Imaging. Radiology. doi:10.1148/radiol.2015150006:150006
King V, Goldfarb SB, Brooks JD et al (2012) Effect of aromatase inhibitors on background parenchymal enhancement and amount of fibroglandular tissue at breast MR imaging. Radiology 264:670–678
King V, Kaplan J, Pike MC et al (2012) Impact of tamoxifen on amount of fibroglandular tissue, background parenchymal enhancement, and cysts on breast magnetic resonance imaging. Breast J 18:527–534
Schrading S, Schild H, Kuhr M, Kuhl C (2014) Effects of tamoxifen and aromatase inhibitors on breast tissue enhancement in dynamic contrast-enhanced breast MR imaging: a longitudinal intraindividual cohort study. Radiology 271:45–55
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Giess CS, Yeh ED, Raza S, Birdwell RL (2014) Background parenchymal enhancement at breast MR imaging: normal patterns, diagnostic challenges, and potential for false-positive and false-negative interpretation. RadioGraphics 34:234–247
Jansen SA, Lin VC, Giger ML, Li H, Karczmar GS, Newstead GM (2011) Normal parenchymal enhancement patterns in women undergoing MR screening of the breast. Eur Radiol 21:1374–1382
Uematsu T, Kasami M, Watanabe J (2012) Background enhancement of mammary glandular tissue on breast dynamic MRI: imaging features and effect on assessment of breast cancer extent. Breast Cancer 19:259–265
Melsaether A, McDermott M, Gupta D, Pysarenko K, Shaylor SD, Moy L (2014) Inter- and intrareader agreement for categorization of background parenchymal enhancement at baseline and after training. AJR Am J Roentgenol 203:209–215
Edwards SD, Lipson JA, Ikeda DM, Lee JM (2013) Updates and revisions to the BI-RADS magnetic resonance imaging lexicon. Magn Reson Imaging Clin N Am 21:483–493
Dontchos BN, Rahbar H, Partridge SC et al (2015) Are Qualitative Assessments of Background Parenchymal Enhancement, Amount of Fibroglandular Tissue on MR Images, and Mammographic Density Associated with Breast Cancer Risk? Radiology 276:371–380
van der Velden BH, Dmitriev I, Loo CE, Pijnappel RM, Gilhuijs KG (2015) Association between Parenchymal Enhancement of the Contralateral Breast in Dynamic Contrast-enhanced MR Imaging and Outcome of Patients with Unilateral Invasive Breast Cancer. Radiology. doi:10.1148/radiol.15142192:142192
Hattangadi J, Park C, Rembert J et al (2008) Breast stromal enhancement on MRI is associated with response to neoadjuvant chemotherapy. AJR Am J Roentgenol 190:1630–1636
Acknowledgments
The scientific guarantor of this publication is Benjamin Wiesinger, M.D. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional review board approval was obtained.
Written informed consent was waived by the institutional review board. Methodology: retrospective, diagnostic or prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Preibsch, H., Wanner, L., Bahrs, S.D. et al. Background parenchymal enhancement in breast MRI before and after neoadjuvant chemotherapy: correlation with tumour response. Eur Radiol 26, 1590–1596 (2016). https://doi.org/10.1007/s00330-015-4011-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-4011-x