Abstract
Purpose
This study was designed to evaluate the relationship between the minimal margin size and local tumor progression (LTP) following CT-guided radiofrequency ablation (RFA) of colorectal cancer liver metastases (CLM).
Methods
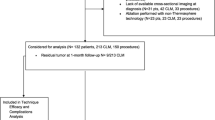
An institutional review board-approved, HIPPA-compliant review identified 73 patients with 94 previously untreated CLM that underwent RFA between March 2003 and May 2010, resulting in an ablation zone completely covering the tumor 4–8 weeks after RFA dynamic CT. Comparing the pre- with the post-RFA CT, the minimal margin size was categorized to 0, 1–5, 6–10, and 11–15 mm. Follow-up included CT every 2–4 months. Kaplan–Meier methodology and Cox regression analysis were used to evaluate the effect of the minimal margin size, tumor location, size, and proximity to a vessel on LTP.
Results
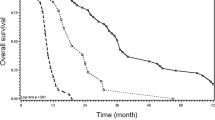
Forty-five of 94 (47.9 %) CLM progressed locally. Median LTP-free survival (LPFS) was 16 months. Two-year LPFS rates for ablated CLM with minimal margin of 0, 1–5 mm, 6–10 mm, 11–15 mm were 26, 46, 74, and 80 % (p < 0.011). Minimal margin (p = 0.002) and tumor size (p = 0.028) were independent risk factors for LTP. The risk for LTP decreased by 46 % for each 5-mm increase in minimal margin size, whereas each additional 5-mm increase in tumor size increased the risk of LTP by 22 %.
Conclusions
An ablation zone with a minimal margin uniformly larger than 5 mm 4–8 weeks postablation CT is associated with the best local tumor control.








Similar content being viewed by others
References
Berber E, Siperstein A (2008) Local recurrence after laparoscopic radiofrequency ablation of liver tumors: an analysis of 1032 tumors. Ann Surg Oncol 15(10):2757–2764
Mulier S, Ruers T, Jamart J, Michel L, Marchal G, Ni Y (2008) Radiofrequency ablation versus resection for resectable colorectal liver metastases: time for a randomized trial? An update. Dig Surg 25(6):445–460
Leen E, Horgan PG (2007) Radiofrequency ablation of colorectal liver metastases. Surg Oncol 16(1):47–51
Ayav A, Germain A, Marchal F et al (2010) Radiofrequency ablation of unresectable liver tumors: factors associated with incomplete ablation or local recurrence. Am J Surg 200(4):435–439
Sofocleous C, Nascimento R, Petrovic L et al (2008) Histopathology of tissue extracted on the probe after radiofrequency ablation of liver malignancy can predict local progression: initial results. Radiology 249(1(Oct)):364–374
Kim YS, Rhim H, Cho OK, Koh BH, Kim Y (2006) Intrahepatic recurrence after percutaneous radiofrequency ablation of hepatocellular carcinoma: analysis of the pattern and risk factors. Eur J Radiol 59(3):432–441
Mulier S, Ni Y, Jamart J, Ruers T, Marchal G, Michel L (2005) Local recurrence after hepatic radiofrequency coagulation: multivariate meta-analysis and review of contributing factors. Ann Surg Oncol 242:158–171
Kim YS, Lee WJ, Rhim H, Lim HK, Choi D, Lee JY (2010) The minimal ablative margin of radiofrequency ablation of hepatocellular carcinoma (>2 and <5 cm) needed to prevent local tumor progression: 3D quantitative assessment using CT image fusion. AJR Am J Roentgenol 195(3):758–765
Okuwaki Y, Nakazawa T, Shibuya A et al (2008) Intrahepatic distant recurrence after radiofrequency ablation for a single small hepatocellular carcinoma: risk factors and patterns. J Gastroenterol 43(1):71–78
Nakazawa T, Kokubu S, Shibuya A et al (2007) Radiofrequency ablation of hepatocellular carcinoma: correlation between local tumor progression after ablation and ablative margin. AJR Am J Roentgenol 188(2):480–488
Liu CH, Arellano RS, Uppot RN, Samir AE, Gervais DA, Mueller PR (2010) Radiofrequency ablation of hepatic tumours: effect of post-ablation margin on local tumour progression. Eur Radiol 20(4):877–885
Frich L, Hagen G, Brabrand K et al (2007) Local tumor progression after radiofrequency ablation of colorectal liver metastases: evaluation of ablative margin and three-dimensional volumetric analysis. J Vasc Interv Radiol 18(9):1134–1140
Crocetti L, de Baere T, Lencioni R (2010) Quality improvement guidelines for radiofrequency ablation of liver tumours. Cardiovasc Intervent Radiol 33(1):11–17
Goldberg SN, Grassi CJ, Cardella JF et al (2009) Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol 20(7 Suppl):S377–S390
Kei SK, Rhim H, Choi D, Lee WJ, Lim HK, Kim YS (2008) Local tumor progression after radiofrequency ablation of liver tumors: analysis of morphologic pattern and site of recurrence. AJR Am J Roentgenol 190(6):1544–1551
Fujioka C, Horiguchi J, Ishifuro M et al (2006) A feasibility study: evaluation of radiofrequency ablation therapy to hepatocellular carcinoma using image registration of preoperative and postoperative CT. Acad Radiol 13(8):986–994
Schraml C, Clasen S, Schwenzer NF et al (2008) Diagnostic performance of contrast-enhanced computed tomography in the immediate assessment of radiofrequency ablation success in colorectal liver metastases. Abdom Imaging 33(6):643–651
Kim KW, Lee JM, Klotz E et al (2011) Safety margin assessment after radiofrequency ablation of the liver using registration of preprocedure and postprocedure CT images. AJR Am J Roentgenol 196(5):W565–W572
Goldberg SN, Grassi CJ, Cardella JF et al (2005) Image-guided tumor ablation: standardization of terminology and reporting criteria. Radiology 235(3):728–739
Choi H, Loyer EM, DuBrow RA et al (2001) Radio-frequency ablation of liver tumors: assessment of therapeutic response and complications. Radiographics 21(Spec No):S41–S54
Pua BB, Sofocleous CT (2010) Imaging to optimize liver tumor ablation. Imaging Med 2(4):433–443
Fong Y, Cohen AM, Fortner JG et al (1997) Liver resection for colorectal metastases. J Clin Oncol 15(3):938–946
Jemal A, Murray T, Samuels A, Ghafoor A, Ward E, Thun MJ (2003) Cancer statistics 2003. CA Cancer J Clin 53(1):5–26
Kulaylat MN, Gibbs JF (2010) Thermoablation of colorectal liver metastasis. J Surg Oncol 101(8):699–705
Kuvshinoff BW, Ota DM (2002) Radiofrequency ablation of liver tumors: influence of technique and tumor size. Surgery 132(4):605–611 discussion 611-612
Pawlik TM, Izzo F, Cohen DS, Morris JS, Curley SA (2003) Combined resection and radiofrequency ablation for advanced hepatic malignancies: results in 172 patients. Ann Surg Oncol 10(9):1059–1069
Sofocleous CT, Petre EN, Gonen M et al (2011) CT-guided radiofrequency ablation as a salvage treatment of colorectal cancer hepatic metastases developing after hepatectomy. J Vasc Interv Radiol 22(6):755–761
Oshowo A, Gillams A, Harrison E, Lees WR, Taylor I (2003) Comparison of resection and radiofrequency ablation for treatment of solitary colorectal liver metastases. Br J Surg 90(10):1240–1243
Machi J, Oishi AJ, Sumida K et al (2006) Long-term outcome of radiofrequency ablation for unresectable liver metastases from colorectal cancer: evaluation of prognostic factors and effectiveness in first- and second-line management. Cancer J 12(4):318–326
Elias D, De Baere T, Smayra T, Ouellet JF, Roche A, Lasser P (2002) Percutaneous radiofrequency thermoablation as an alternative to surgery for treatment of liver tumour recurrence after hepatectomy. Br J Surg 89(6):752–756
Gillams AR, Lees WR (2009) Five-year survival in 309 patients with colorectal liver metastases treated with radiofrequency ablation. Eur Radiol 19(5):1206–1213
Hur H, Ko YT, Min BS et al (2009) Comparative study of resection and radiofrequency ablation in the treatment of solitary colorectal liver metastases. Am J Surg 197(6):728–736
Sorensen SM, Mortensen FV, Nielsen DT (2007) Radiofrequency ablation of colorectal liver metastases: long-term survival. Acta Radiol (Stockholm, Sweden: 1987) 48(3):253–258
Vogl TJ, Straub R, Eichler K, Sollner O, Mack MG (2004) Colorectal carcinoma metastases in liver: laser-induced interstitial thermotherapy–local tumor control rate and survival data. Radiology 230(2):450–458
Hayashi M, Inoue Y, Komeda K et al (2010) Clinicopathological analysis of recurrence patterns and prognostic factors for survival after hepatectomy for colorectal liver metastasis. BMC Surg 10:27
de Haas RJ, Wicherts DA, Flores E, Azoulay D, Castaing D, Adam R (2008) R1 resection by necessity for colorectal liver metastases: is it still a contraindication to surgery? Ann Surg 248(4):626–637
de Jong MC, Pulitano C, Ribero D et al (2009) Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg 250(3):440–448
Are C, Gonen M, Zazzali K et al (2007) The impact of margins on outcome after hepatic resection for colorectal metastasis. Ann Surg 246(2):295–300
Sofocleous CT, Klein KM, Hubbi B et al (2004) Histopathologic evaluation of tissue extracted on the radiofrequency probe after ablation of liver tumors: preliminary findings. AJR Am J Roentgenol 183(1):209–213
Snoeren N, Jansen MC, Rijken AM et al (2009) Assessment of viable tumour tissue attached to needle applicators after local ablation of liver tumours. Dig Surg 26(1):56–62
Snoeren N, Huiskens J, Rijken AM et al (2011) Viable tumor tissue adherent to needle applicators after local ablation: a risk factor for local tumor progression. Ann Surg Oncol 18(13):3702–3710
Sofocleous CT, Garg S, Petrovic LM et al (2012) Ki-67 is a Prognostic Biomarker of Survival after Radiofrequency Ablation of Liver Malignancies (In Press)
Lu DS, Raman SS, Limanond P et al (2003) Influence of large peritumoral vessels on outcome of radiofrequency ablation of liver tumors. J Vasc Interv Radiol 14(10):1267–1274
Keil S, Bruners P, Schiffl K et al (2010) Radiofrequency ablation of liver metastases-software-assisted evaluation of the ablation zone in MDCT: tumor-free follow-up versus local recurrent disease. Cardiovasc Intervent Radiol 33(2):297–306
Wood BJ, Locklin JK, Viswanathan A et al (2007) Technologies for guidance of radiofrequency ablation in the multimodality interventional suite of the future. J Vasc Interv Radiol 18(1 Pt 1):9–24
Acknowledgments
This work was supported in part by NIH Grant No. 5R21CA131763.
Conflict of interest
Authors Xiaodong Wang, Constantinos T. Sofocleous, Joseph P. Erinjeri, Elena N. Petre, Mithat Gonen, Kinh G. Do, Karen T. Brown, Anne M. Covey, Lynn A. Brody, William Alago, Raymond H. Thornton, and Kemeny NE have no conflict of interest to declare. Stephen B. Solomon—consultant for Covidien (Mansfield, MA) and Johnson and Johnson (Piscataway, NJ) and has a research contract with GE Healthcare (Milwaukee, WI).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, X., Sofocleous, C.T., Erinjeri, J.P. et al. Margin Size is an Independent Predictor of Local Tumor Progression After Ablation of Colon Cancer Liver Metastases. Cardiovasc Intervent Radiol 36, 166–175 (2013). https://doi.org/10.1007/s00270-012-0377-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-012-0377-1