Abstract
Background: Inhibition of the COX-2 enzyme has been shown to have a radiosensitizing effect in epithelial cancers. The aim of this study was to investigate whether the efficacy of radioimmunotherapy (RIT) using 131I-labeled anti-CEA monoclonal antibody MN-14 could be enhanced by co-administration of the selective COX-2 inhibitor Parecoxib in mice with small volume (1–3 mm) peritoneal carcinomatosis of colonic origin. Methods: First, the efficacy of 14 daily injections of Parecoxib monotherapy (0 – 0.2 – 1.0 – 5.0 – 25.0 mg/kg) was determined in mice with intraperitoneal LS174T xenografts. Second, the influence of Parecoxib (1.0 or 5.0 mg/kg) on the biodistribution of 125I-MN-14 was assessed. Finally, the efficacy of RIT alone [125 μCi 131I-MN-14/mouse ≈ 1/4 of the maximal tolerated dose (MTD)] was compared with that of Parecoxib monotherapy and RIT combined with daily injections of Parecoxib (1.0 or 5.0 mg/kg). Results: Parecoxib had no measurable antitumor effect up to the highest dose level (25 mg/kg). Parecoxib had no effect on the uptake of 125I-MN-14 in the intraperitoneal tumor xenografts or on normal tissue distribution. Median survival of the control mice and the mice treated with Parecoxib monotherapy (1.0 or 5.0 mg/kg) was 48.5 days, 52 days and 52 days (P=0.47). RIT alone significantly delayed the growth of the intraperitoneal xenografts resulting in a median survival of 87 days (P<0.0001). Mice treated with RIT + Parecoxib at 1.0 or 5.0 mg/kg had a median survival of 73.5 days and 76 days, respectively, which was not statistically different from survival after RIT alone (P=0.15). Conclusion: The COX-2 inhibitor Parecoxib does not enhance the therapeutic efficacy of RIT of experimental small volume peritoneal carcinomatosis of colonic origin.
Similar content being viewed by others
Introduction
Despite the promising results in hematological malignancies, the merely modest therapeutic efficacy of radioimmunotherapy (RIT) using radiolabeled monoclonal antibodies (MAbs) in patients with solid cancers has tempered the initial enthusiasm with which this treatment modality was once greeted [1]. The targeting of intravenously administered radiolabeled antibodies at solid tumors is a relatively inefficient process due to various tumor-related factors, including a limited vascular supply, heterogeneous uptake of the antibody in the tumor, and elevated interstitial pressure in combination with a relatively long transport distance in the interstitium [2]. As a result, tumor uptake of radiolabeled MAbs and, consequently, the radiation doses delivered to solid lesions are in most cases too low to induce objective tumor responses. Several innovative approaches have been pursued with the aim of improving the efficacy of RIT. These include strategies to improve the localization and retention of radiolabeled MAbs in the tumor (e.g. using high-affinity MAbs [3, 4]), strategies to accelerate the blood clearance of MAbs (e.g. using antibody fragments [5, 6] or the pretargeting method [7]), and strategies to increase the sensitivity of the tumor cells to radiation (e.g. by means of radiosensitizers [8–10]).
In the early 1990s, the inducible second isoform of cyclooxygenase (COX-2) was recognized to playing a significant role in colorectal carcinogenesis. This observation was derived from epidemiological studies indicating that chronic users of non-steroid anti-inflammatory drugs (NSAIDs) had a 40–50% reduced risk of developing colorectal cancer (CRC) [11]. The COX-2 enzyme catalyzes the conversion of arachidonic acid to prostaglandin derivatives and its expression is upregulated at sites of inflammation [12] and in various epithelial cancers, including 80–90% of human colon carcinomas [13]. To date, COX-2 has been acknowledged to be involved in various biological processes in epithelial and nonepithelial cancers, including the regulation of apoptosis [14, 15], tumor cell invasiveness and metastatic potential [16], tumor angiogenesis [17], and protection against radiation damage [18].
Because of the gastrointestinal and hematological toxicity of nonselective NSAIDs [19], the potential of selective inhibitors of the COX-2 enzyme (so-called Coxibs) to act as radiosensitizing agents has been the subject of investigation in various preclinical and ongoing clinical studies. Coxibs were indeed shown to increase the sensitivity of tumor cells to external beam radiation in various experimental models of colon cancer [20], breast cancer [21], head and neck cancer [20, 22], lung cancer [21, 23], sarcoma [24, 25], and glioma [26] without increasing radiation-induced toxicity to normal tissue. To date, however, there have been no publications on the use of COX-2 inhibitors in combination with RIT.
We have characterized a nude mouse model for RIT of small volume peritoneal carcinomatosis of colorectal origin using the human colon carcinoma cell line LS174T [27, 28]. RIT using the radiolabeled anti-CEA MAb MN-14 proved very effective in delaying the outgrowth of intraperitoneal tumor xenografts, even at relatively low activity doses. The COX-2 enzyme is upregulated and actively mediates the production of prostaglandin E2 (PGE2) in the LS174T tumor cells [29]. PGE2 has been shown to promote the growth and metastatic potential of colon carcinoma cells in vitro and implicated as a protector against radiation damage [18].
The novel, selective COX-2 inhibitor Parecoxib is a prodrug specifically designed for parenteral administration [30]. After systemic administration, Parecoxib is rapidly converted to the COX-2 inhibitor Valdecoxib by enzymatic hydrolysis in the liver [31, 32]. Valdecoxib is one of the most potent and selective COX-2 inhibitors that have been developed to date [33, 34]. Since Parecoxib monotherapy has been reported to have antitumor effects in mouse models of breast cancer and colon cancer [35, 36], we hypothesized that co-administration of the COX-2 inhibitor Parecoxib might sensitize the LS174T xenografts to radiation and improve the therapeutic efficacy of RIT in our model of small volume peritoneal carcinomatosis of colorectal origin.
To test this hypothesis, we designed a series of experiments that aimed to determine the efficacy of Parecoxib monotherapy, and to assess the effect of Parecoxib co-administration on the biodistribution and therapeutic efficacy of radiolabeled MN-14.
Materials and methods
Animal model of small peritoneal metastases
Male nude BALB/c mice (Charles River Laboratories, Germany), 7–9 weeks old, weighing 20–25 g, were used in the experiments. Mice were accustomed to laboratory conditions for at least week before experimental use and were housed under nonsterile standard conditions (temperature 20–24°C; relative humidity 50–60%; 12 h light/12 h dark) in filter-topped cages (up to five mice per cage), on sawdust with free access to animal chow (Snif Voer, Soest, The Netherlands) and water. Peritoneal metastases were induced as described previously [27]. Briefly, mice were inoculated intraperitoneally with 1.0×106 LS174T cells (CCL 188, American Type Culture Collection, Rockville, MD, USA), suspended in 500 μl of RPMI-1640 medium using a 23-gauge needle. In this model, the first macroscopic tumor nodules are seen 7–10 days thereafter, whereas bulky peritoneal carcinomatosis develops 3–6 weeks after tumor cell inoculation. Before initiating the experimental studies, the COX-2 expression of LS174T was immunohistochemically confirmed using a murine anti-COX-2 polyclonal antibody (Brunschwig Chemie, Amsterdam, The Netherlands), as shown in Fig. 1. The experiments were approved by the institutional Animal Welfare Committee of the University Medical Center Nijmegen and conducted in accordance with the principles set forth by the revised Dutch Act on Animal Experimentation (1997).
Monoclonal antibody
The murine MN-14 MAb is a high-affinity (K a =109 M−1) class-III anti-CEA IgG1 antibody, produced by a hybridoma cell line culture, kindly provided by Immunomedics, Inc. (Morris Plains, New Jersey, USA) [37]. The antibodies were purified by protein A chromatography, as described previously [38]. Purity was checked by SDS-PAGE under nonreduced conditions and by means of fast protein liquid chromatography (FPLC) on a Phenomenex Biosep 3000 column, eluted with phosphate buffered saline (PBS, pH 7.2, 1 ml/min).
Radioiodination and quality control
Antibodies were radioiodinated with 125I (Amersham, Den Bosch, The Netherlands) or 131I (MDS Nordion, Fleurus, Belgium) using the IODOGEN-method (1,3,4,6-tetrachloro-3α,6α-diphenyl-glycoluril; Pierce, Rockford, IL, USA). Briefly, antibodies and 125I or 131I were incubated at room temperature in 85 μl of PBS (0.10 M, pH 7.4) in a glass vial coated with 50–100 μg iodogen. After 12 min, the reaction mixture was separated on a PD-10 column (Amersham Biosciences, Uppsala, Sweden), eluted with PBS, 0.5% bovine serum albumin (BSA). Labeling efficiency of the radioiodination reactions exceeded 70%. In the biodistribution study the specific activity of the primary 125I-MN-14 preparation was 2.9 μCi/μg. Specific activity of the primary 131I-MN-14 preparation in the therapy study was 23.4 μCi/μg. In a previous study we demonstrated that the uptake of the radiolabeled MN-14 antibody in tumors was optimal at MN-14 protein doses up to 25 μg [27]. Therefore, in the present study the radiolabeled antibody preparations were augmented with unlabeled MN-14 to a total antibody protein dose of 20 μg per mouse.
The amount of free iodine was determined by instant thin layer chromatography (ITLC) with ITLC silica gel strips (Gelman Sciences, Inc., Ann Arbor, MI, USA) using 0.1 M citrate buffer (pH 6.0) as the mobile phase. Radiochemical purity of the radioiodinated antibody preparations used in the studies exceeded 98%. The immunoreactive fraction (IRF) at infinitive antigen excess of the radiolabeled MN-14 preparation was determined on freshly trypsinized LS174T cells essentially as described by Lindmo et al. [39] with minor modifications. Briefly, a fixed amount of labeled antibody (10,000 cpm) was incubated with increasing concentrations of LS174T tumor cells (1.2×106 – 20×106 cells/ml) in 0.5 ml binding buffer (RPMI medium containing 0.5% BSA and 0.05% NaN3). A duplicate of the lowest cell concentration was incubated in the presence of an excess unlabeled antibody to correct for non-specific binding. After 6 h of incubation at 37°C, the cells were washed and activity in the pellet was determined in a well-type gamma-counter. The inverse of the tumor cell bound fraction was plotted against the inverse of the cell concentration and the IRF was calculated from the Y-axis intercept. The IRFs of the 125I-MN-14 and 131I-MN-14 preparations were 80% and 76%, respectively. The radiolabeled antibody preparations were administered within 2 h after radiolabeling.
Parecoxib
Parecoxib sodium (Dynastat), a selective COX-2 inhibitor specifically developed for parenteral administration, was purchased from Pharmacia Europe EEIG (Buckinghamshire, UK) as a powder in glass vials (40 mg/vial). Parecoxib was dissolved in 0.9% sodium chloride (saline) to the appropriate concentrations immediately before use and administered intraperitoneally (0.2 ml/mouse).
Therapeutic efficacy of Parecoxib monotherapy
To evaluate the therapeutic efficacy of Parecoxib when given as monotherapy, mice bearing small peritoneal metastases were treated with daily intraperitoneal administrations of increasing doses of Parecoxib (0.2, 1.0, 5.0, or 25.0 mg/kg) for 14 consecutive days, starting on the tenth day after tumor cell inoculation. Control mice received saline only (eight mice per group). Prior to each administration, body weight, as a surrogate measure of toxicity, was recorded. Thirty days after tumor cell inoculation, all mice were killed by O2/CO2-asphyxiation and dissected. At dissection the intraperitoneal tumor load was scored semiquantitavely, according to the peritoneal cancer index (PCI) as described by Eggermont et al. [40]. In brief, the intraperitoneal tumor load could be given a PCI of 0, 1, 2, or 3, where 0 indicated no macroscopic tumor growth, 1 meant ≤3 pin-point tumor foci that have a diameter of ≤1 mm, 2 indicated moderate tumor growth, and 3 indicated abundant intraperitoneal tumor growth, replacing most of the peritoneal cavity. Subsequently, after designating a PCI rate, all macroscopic tumor deposits were meticulously excised and weighed.
Effect of Parecoxib on the biodistribution of radioiodinated MN-14
To assess the effect of daily Parecoxib therapy on the biodistribution of radioiodinated MN-14, 10 days after tumor cell inoculation 45 mice received an i.p. injection of 125I-MN-14 (5 μCi/20 μg/mouse). Parecoxib therapy, which consisted of daily intraperitoneal administrations of 1.0 mg/kg or 5.0 mg/kg per mouse, was started concurrently with the administration of the radiolabeled antibodies. Control mice received saline only. Mice were killed by O2/CO2-asphyxia and dissected at 24 h (i.e. after one administration of Parecoxib), 72 h (i.e. after two administration of Parecoxib) and 168 h (i.e. after six administrations of Parecoxib) after the administration of 125I-MN-14 (five mice per group). Tumor, blood, liver, spleen, kidney, small intestine, cecum, lung and muscle tissues were sampled, gently blotted dry, and immediately weighed. Radioactivity was measured with a shielded well-type gamma-counter (Wizard, Pharmacia-LKB, Sweden). To correct for physical decay and to calculate the uptake of the radioiodinated antibody in each sample as a fraction of the injected dose, aliquots of the injected dose were counted simultaneously. The results were expressed as percentage of the injected dose per gram tissue (% ID/g).
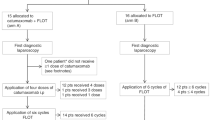
Combination therapy of RIT and Parecoxib
To assess the radiosensitizing effect of Parecoxib when combined with RIT, 10 days after tumor cell inoculation, groups of 12 mice each were treated with either 131I-MN-14 (125 μCi/mouse, which is approximately 25% of the maximal tolerated dose (MTD)), Parecoxib (either 1.0 mg/kg or 5.0 mg/kg/day for fourteen consecutive days) or 131I-MN-14 combined with Parecoxib. 131I-MN-14 was given intraperitoneally on day 10 in 200 μl of PBS, 0.5% BSA. Parecoxib was given daily by intraperitoneal injections in from day 10 till 23. Control mice received daily intraperitoneal injections of 200 μl of saline. Mice treated with RIT only, were given daily injections of 200 μl of saline. Prior to each administration, the mice were weighed to ensure that body weight loss did not exceed 20%. Mice were monitored daily and body weight was measured daily in the first 2 weeks after the first administration. Mice were monitored until the body weight had dropped more than 20% or until the humane endpoint had been reached, as determined by an experienced and independent animal technician, who was ignorant of the therapeutic regimen. At the time of the humane endpoint, mice were usually cachectic and drowsy, showing signs of advanced peritoneal carcinomatosis, such as the presence of bloody ascites or bulky intraperitoneal tumor growth, and were expected to die with one or two days. When body weight had dropped more than 20% or the humane endpoint had been reached, mice were killed by O2/CO2-asphyxiation and immediately dissected. At dissection, tumor load was scored by the PCI, as described above, and all tumor deposits were excised and weighed. The experiment was terminated at 118 days after tumorcell inoculation when the remaining mice were killed and dissected. The abdominal cavity was carefully inspected. Liver, spleen, lungs, pancreas, greater omentum and the diaphragm were removed for routine histopathological H & E-staining and immunohistochemical staining using a rabbit-anti-human anti-CEA polyclonal antibody (A 0115, DakoCytomation, Glostrup, Denmark).
Statistical analysis
Statistical analysis was performed by means of the GraphPad Prism 4.00 software (GraphPad Software, San Diego, CA, USA). Comparisons were analyzed using the one-way ANOVA test. Bonferroni correction for multiple testing was applied. Survival curves were compared using the Log-rank test. All tests were two-sided; the level of statistical significance was set a P-value of <0.05.
Results
Parecoxib monotherapy
Fourteen daily administrations of Parecoxib, when given as sole treatment, had no influence on body weight at any of the dose levels tested. Thirty days after tumor cell inoculation, one mouse of the control group, had abundant intraperitoneal tumor growth. At that time it was decided to terminate the experiment and dissect all animals. At dissection, all mice of the control group that had been treated with saline had macroscopic tumor growth. Of the mice treated with 0.2 mg/kg or 1.0 mg/kg per administration, one mouse of each group no macroscopic tumor growth. Of those mice that had been treated at dose levels of 5.0 mg/kg or 25.0 mg/kg per administration, two out of eight and four out of eight had no macroscopic tumor growth, respectively. The PCI designated to the mice is depicted in Fig. 2. The median PCI (range) varied between 2 (1–3) in the control group and 1 (0–3) in the mice treated with Parecoxib at 25.0 mg/kg. There was a borderline significant trend towards a lower PCI at higher Parecoxib dosages (P=0.097). In Fig. 3, the tumor weight found in each mouse is given. The mean (±SD) tumor weight varied between 1.3 (±1.5) g in the control group and 0.5 (±0.4) g in the mice treated with Parecoxib at 0.2 mg/kg (P=0.15 for trend). There was a highly significant correlation between the PCI and the weight of the dissected tumor deposits (Spearman r=0.9349, P<0.0001).
The PCI designated to mice with small intraperitoneal LS174T xenografts after treatment with either daily intraperitoneal administrations of saline or increasing dosages of Parecoxib (0.2 – 25.0 mg/kg) for 14 consecutive days. Lines indicate the median and range. There was a borderline significant trend towards a lower PCI at higher Parecoxib dosages (P=0.097)
Influence of Parecoxib on the biodistribution of radioiodinated MN-14
The results of the experiment in which the effect of Parecoxib on tumor uptake and biodistribution of 125I-labeled MN-14 was studied, are summarized in Table 1. Parecoxib co-administration had no effect on the uptake of 125I-MN-14 in tumor or on the blood levels or tumor-to-blood ratios. Mean uptake of 125I-MN-14 in tumor nodules obtained from the control mice at 24, 72 and 168 h post-injection (p.i.) amounted 51.4 (±13.8)% ID/g, 38.6 (±5.8)% ID/g and 35.6 (±21.6)% ID/g, respectively. Tumor uptake of 125I-MN-14 in the mice that received daily administration of either 1.0 mg/kg or 5.0 mg/kg Parecoxib was very similar to that in control mice, as shown in Fig. 4. Furthermore, Parecoxib co-administration had no influence on the normal tissue distribution of 125I-MN-14 at the various time points tested.
Combination therapy of Parecoxib and 131I-labeled MN-14
To test the hypothesis that the COX-2 inhibitor Parecoxib might improve the efficacy of RIT in small peritoneal metastases, Parecoxib was administered daily for fourteen consecutive days, starting concurrently with the administration of 131I-MN-14.
Control mice that were treated with daily injections of saline showed a maximum weight loss of 1.9±3.9% at 4 d after the start of treatment. RIT alone using 125 μCi 131I-MN-14 per mouse resulted in a maximum weight loss of 3.9±1.5% 4 days after administration of the radiolabeled antibodies. The toxicity of RIT was not affected by co-administration of Parecoxib. Maximum weight loss after RIT combined with daily administrations of Parecoxib at 1.0 mg/kg or 5.0 mg/kg was 3.5±2.6% and 4.8±0.9, respectively (P=0.42). There were no treatment-related deaths.
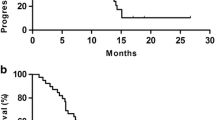
Five mice (7%) developed large subcutaneous tumors at the inoculation site and were excluded from the survival analysis. The survival curves for the various treatment groups are shown in Fig. 5. Median survival of the control mice was 48.5 days (range 38–73). Parecoxib monotherapy at 1.0 mg/kg or 5.0 mg/kg resulted in a median survival of 52 days (range 38–118) and 52 days (range 44–118), respectively (P=0.47). RIT alone resulted in a significantly improved median survival of 87 days (range 55–118, P<0.0001). Daily intraperitoneal injections of Parecoxib at 1.0 mg/kg or 5.0 mg/kg during fourteen consecutive days after the administration of 131I-MN-14 resulted in a median survival of 73.5 (range 55–118) and 76 (range 55–90) days, respectively (P=0.15, comparing RIT alone with RIT + Parecoxib 1.0 mg/kg or 5.0 mg/kg). Although the difference between the survival of the mice treated with RIT alone and the mice treated with RIT + Parecoxib 1.0 mg/kg was not significant (P=0.19), median survival of the mice treated with RIT alone was significantly better than that of the mice treated with RIT + Parecoxib 5.0 mg/kg (P=0.029).
At dissection, the PCI was three for all control mice. Median PCI for the mice treated with Parecoxib 1.0 mg/kg, Parecoxib 5.0 mg/kg, RIT alone, RIT + Parecoxib 1.0 mg/kg and RIT + Parecoxib 5.0 mg/kg was 2.6 (range 2–3), 3 (range 2–3), 3 (range 2–3), 3 (range 2–3) and 3 (range 2–3), respectively (P=0.56). Fig. 6 depicts the tumor weight that was found at dissection at the time mice reached their humane endpoints. It varied between 4.3±1.4 for the mice treated with Parecoxib 5.0 mg/kg and 4.9±1.6 for the mice treated with RIT + Parecoxib 5.0 mg/kg (P=0.94).
The highly similar tumor mass found in the mice demonstrates that there was no bias in determining the humane endpoint. The method of determining and comparing the survival was therefore reliable.
At the end of the experiment (118 days after tumor cell inoculation), there were five long-term survivors (two treated with RIT alone; one treated with RIT + Parecoxib 1.0 mg/kg; and two treated with Parecoxib monotherapy at 1.0 mg/kg and 5.0 mg/kg, respectively), without signs of intraperitoneal tumor growth. At dissection, the mouse that had been treated with Parecoxib monotherapy at 5.0 mg/kg had macroscopic tumor growth (0.36 g; PCI 2), whereas in the remaining four mice there was no evidence of disease. Histopathological examination of relevant organs, including the greater omentum, mesentery, diaphragm and pancreas did not reveal residual disease in any of these mice.
Discussion
The primary aim of the current study was to investigate the potential of the COX-2 inhibitor Parecoxib to act as a radiosensitizer when combined with RIT in a well-characterized animal model of small volume peritoneal carcinomatosis of colonic origin. Daily administration of Parecoxib, however, failed to improve the efficacy of RIT using 131I-MN-14 in this model.
The COX-2 inhibitor Parecoxib was selected, since it has several favorable properties that made it attractive as a potential radiosensitizer. In contrast to other commercially available selective COX-2 inhibitors that are poorly soluble in water and can only be given orally, Parecoxib is water-soluble and was specifically developed for parenteral (intramuscular or intravenous) administration. As such, Parecoxib allows more precise dosing. After hydrolysis in the liver, the active metabolite Valdecoxib binds non-covalently to COX-2, forming a firm and stable enzyme-inhibitor complex [41]. Valdecoxib has been shown to have a higher in vitro affinity to COX-2, and bind more rapidly to and dissociate from COX-2 more slowly than Celecoxib [42, 43], which has been one of the most used and studied COX-2 inhibitors. Although there are no published data on the pharmacokinetics of Parecoxib in mice, experimental studies in rats have shown that after intravenous administration Parecoxib is rapidly converted to Valdecoxib (conversion time, 8 min), which then has a plasma half-life of 4–5 h [34]. Zhang et al. [44] studied the pharmacokinetics of [14C]Valdecoxib after oral ingestion at 5 mg/kg in mice, and found a peak plasma concentration at 30 min after ingestion and the half-life in blood of approximately 4 h, with most of the [14C] Valdecoxib associated with the red blood cells.
COX-2 inhibition with Parecoxib has been shown to have antitumor effects in experimental breast cancer and colon cancer [35, 36]. O’Donoghue et al. [35] investigated the therapeutic efficacy of fifteen daily intraperitoneal administrations of Parecoxib (0.5 mg/kg) in mice bearing subcutaneous breast cancer xenografts and observed growth inhibition of the primary tumor and pulmonary metastases. Smakman et al. [36] studied the efficacy of twice-daily intraperitoneal injections of Parecoxib (5 mg/kg) for 6 days in mice immediately after inducing liver metastases of colon carcinoma, and reported greatly reduced intrahepatic tumor cell proliferation and the rate of liver metastases outgrowth. Therefore, before combining Parecoxib with RIT in the current model of peritoneal carcinomatosis, we first investigated the toxicity and efficacy of Parecoxib monotherapy. Parecoxib proved to be a safe agent; body weight loss among the treatment groups was similar to that of the control group, and none of the mice had gastric ulcers at dissection. Daily intraperitoneal injections of Parecoxib during fourteen consecutive days had no statistically significant antitumor effect in this study, although there was a borderline trend towards a dose-dependent antitumor effect. At the highest dose level (25.0 mg/kg) four out of eight mice had no macroscopic tumor growth, which suggests that high doses of Parecoxib might have an antitumor effect in this model.
COX-2 derived prostaglandins play an important role in tumor angiogenesis [45]. Selective inhibition of COX-2 has been shown to be associated with a decrease in new vessel formation [46, 47]. Therefore, it could not be excluded that COX-2 inhibition with Parecoxib might affect the tumor uptake of radiolabeled antibodies in RIT, which prompted us to conduct the biodistribution study. Daily administration of Parecoxib at 1.0 mg/kg or 5.0 mg/kg had no effect on the overall biodistribution and tumor uptake in particular, of radioiodinated MN-14 in this model.
To date, several papers have been published reporting synergistic or radiosensitizing activity of COX-2 inhibition when given prior to and concurrently with external beam gamma-irradiation in various epithelial cancers [18]. Celecoxib (Celebrex) or its bioactive compound SC-236, has been the COX-2 inhibitor used in most studies. In view of the pronounced expression of COX-2 in LS174T, and because the efficacy of RIT at relatively lowactivity doses is limited, we hypothesized that inhibition of the COX-2 enzyme might have a synergistic or radiosensitizing effect when combined with RIT in this model. RIT was given at 25% of the MTD, since we previously demonstrated that this activity dose significantly delays the development of peritoneal carcinomatosis but is not curative in this model. Thus, we assumed that a clinically relevant radiosensitizing effect of Parecoxib could be demonstrated at this dose. Since the radiosensitizing effect of Celecoxib has been demonstrated to be dose-dependent in external beam radiation [20], Parecoxib was combined with RIT at two dose in the current study. In concert with the results of the first experiment, in which Parecoxib had no significant antitumor effect, the median survival of the mice treated with Parecoxib monotherapy was similar to that of the control mice. RIT alone significantly improved the median survival as compared with that obtained in the control mice. Daily intraperitoneal administrations of Parecoxib, however, did not enhance the efficacy of RIT, and, of unknown significance, appeared even to be detrimental to the effect of RIT at the higher dose level of Parecoxib (5.0 mg/kg). All mice were killed at the time their clinical condition had deteriorated beyond the humane endpoint due to abundant intraperitoneal tumor growth. Mean tumor weight of all the treatment groups was very similar. Therefore, long-term adverse systemic effects of the COX-2 inhibition seem to be an unlikely explanation for the observed survival difference between the mice treated with RIT alone and those treated with RIT + Parecoxib 5 mg/kg.
Special features of the published experimental models, in which COX-2 inhibitors were successfully applied as radiosensitizers, that might explain the failure of Parecoxib to act as a radiosensitizer in the current model, include the type of radiotherapy (external beam radiation versus RIT), the animal model with respect to the localization of the xenografts (subcutaneous versus intraperitoneal), and the choice of the COX-2 inhibitor. RIT differs from external beam radiation in that in RIT the radiation energy is deposited over a long time interval (low dose rate), whereas in external beam radiation, the radiation energy is delivered in one or more fractions at a high dose rate [48]. Inhibition of the COX-2 enzyme might only sensitize tumor cells to radiation when given at a high dose rate. Furthermore, because of the long time-interval during which the radiation energy is delivered to the tumor nodules in RIT, it seems unlikely that a radiosensitizing effect of Parecoxib would have become apparent had the drug been administered prior to the injection of the radiolabeled antibodies.
Another explanation of the absence of any radiosensitizing activity by Parecoxib may be the intraperitoneal localization of the tumor xenografts, as opposed to the subcutaneous xenografts used in other studies reporting a radiosensitizing effect when COX-2 inhibition was combined with radiotherapy. Whereas in subcutaneous tumor models therapeutic efficacy is determined by measuring the growth of the subcutaneous tumors, in the current model of peritoneal carcinomatosis survival has been the primary endpoint. Failure of the animal model to reveal small differences in therapeutic efficacy might have obscured any additional therapeutic effect of Parecoxib co-administration. Furthermore, although RIT alone was noncurative in eight out of ten mice, its efficacy could have outshined a potential radiosensitizing effect of Parecoxib in this model.
Finally, since Parecoxib is a prodrug that needs to be hydrolyzed by the liver, its active metabolite Valdecoxib can only reach the intraperitoneal tumors via the blood. It cannot be excluded that the vascularization of the small intraperitoneal LS174T xenografts is too limited to allow sufficient supply of the COX-2 inhibitor Valdecoxib. Whether intraperitoneal administration of other COX-2 inhibitors that do not need conversion could reach the intraperitoneal xenografts more effectively and thus enhance RIT of peritoneal carcinomatosis of colonic origin remains to be ascertained.
In conclusion, monotherapy using the COX-2 inhibitor Parecoxib had no antitumor effect in nude mice with small intraperitoneal LS174T colon cancer xenografts. When given concurrently with RIT, Parecoxib had no effect on the biodistribution of the radiolabeled antibodies, did not enhance the therapeutic efficacy of RIT and appeared even to have a detrimental effect on the efficacy of RIT at the highest dose tested. Therefore, Parecoxib should not be used with the intent to sensitize small volume peritoneal metastases to RIT.
References
Koppe MJ, Bleichrodt RP, Oyen WJG, Boerman OC (2005) Radioimmunotherapy of colorectal cancer. Br J Surg (in press)
Jain RK (1990) Physiological barriers to delivery of monoclonal antibodies and other macromolecules in tumors. Cancer Res 50:814s–819s
Juweid M, Sharkey RM, Behr T, Swayne LC, Herskovic T, Pereira M, Rubin AD, Hanley D, Dunn R, Siegel J, Goldenberg DM (1996) Radioimmunotherapy of medullary thyroid cancer with iodine-131-labeled anti-CEA antibodies. J Nucl Med 37:905–911
Schlom J, Eggensperger D, Colcher D, Molinolo A, Houchens D, Miller LS, Hinkle G, Siler K (1992) Therapeutic advantage of high-affinity anticarcinoma radioimmunoconjugates. Cancer Res 52:1067–1072
Behr TM, Blumenthal RD, Memtsoudis S, Sharkey RM, Gratz S, Becker W, Goldenberg DM (2000) Cure of metastatic human colonic cancer in mice with radiolabeled monoclonal antibody fragments. Clin Cancer Res 6:4900–4907
Buchegger F, Mach J-P, Folli S, Delaloye B, Bischof-Delaloye A, Pelegrin A (1996) Higher efficacy of 131I-labeled anti-carcinoembryonic antigen-monoclonal antibody F(ab’)2 as compared to intact antibodies in radioimmunotherapy of established human colon carcinoma grafted in nuce mice. In: Sauter-Bihl M, Bihl H, Wannenmacher W (eds) Systemic radiotherapy with monoclonal antibodies—recent results in cancer research. Springer, Berlin, Heidelberg New york, pp 19–35
Boerman OC, van Schaijk FG, Oyen WJ, Corstens FH (2003) Pretargeted radioimmunotherapy of cancer: progress step by step. J Nucl Med 44:400–411
Cardillo TM, Blumenthal R, Ying Z, Gold DV (2002) Combined gemcitabine and radioimmunotherapy for the treatment of pancreatic cancer. Int J Cancer 97:386–392
Gold DV, Schutsky K, Modrak D, Cardillo TM (2003) Low-dose radioimmunotherapy ((90)Y-PAM4) combined with gemcitabine for the treatment of experimental pancreatic cancer. Clin Cancer Res 9:3929S–3937S
Gold DV, Modrak DE, Schutsky K, Cardillo TM (2004) Combined 90Yttrium-DOTA-labeled PAM4 antibody radioimmunotherapy and gemcitabine radiosensitization for the treatment of a human pancreatic cancer xenograft. Int J Cancer 109:618–626
Paganini-Hill A (1994) Aspirin and the prevention of colorectal cancer: a review of the evidence. Semin Surg Oncol 10:158–164
Gilroy DW, Colville-Nash PR, Willis D, Chivers J, Paul-Clark MJ, Willoughby DA (1999) Inducible cyclooxygenase may have anti-inflammatory properties. Nat Med 5:698–701
Eberhart CE, Coffey RJ, Radhika A, Giardiello FM, Ferrenbach S, DuBois RN (1994) Up-regulation of cyclooxygenase 2 gene expression in human colorectal adenomas and adenocarcinomas. Gastroenterology 107:1183–1188
Watson AJ (1998) Chemopreventive effects of NSAIDs against colorectal cancer: regulation of apoptosis and mitosis by COX-1 and COX-2. Histol Histopathol 13:591–597
Li M, Wu X, Xu XC (2001) Induction of apoptosis in colon cancer cells by cyclooxygenase-2 inhibitor NS398 through a cytochrome c-dependent pathway. Clin Cancer Res 7:1010–1016
Tsujii M, Kawano S, DuBois RN (1997) Cyclooxygenase-2 expression in human colon cancer cells increases metastatic potential. Proc Natl Acad Sci USA 94:3336–3340
Gately S, Li WW (2004) Multiple roles of COX-2 in tumor angiogenesis: a target for antiangiogenic therapy. Semin Oncol 31:2–11
Choy H, Milas L (2003) Enhancing radiotherapy with cyclooxygenase-2 enzyme inhibitors: a rational advance? J Natl Cancer Inst 95:1440–1452
Rostom A, Wells G, Tugwell P, Welch V, Dube C, McGowan J (2000) Prevention of chronic NSAID induced upper gastrointestinal toxicity. Cochrane Database Syst Rev CD002296
Davis TW, O’Neal JM, Pagel MD, Zweifel BS, Mehta PP, Heuvelman DM, Masferrer JL (2004) Synergy between celecoxib and radiotherapy results from inhibition of cyclooxygenase-2-derived prostaglandin E2, a survival factor for tumor and associated vasculature. Cancer Res 64:279–285
Liu W, Chen Y, Wang W, Keng P, Finkelstein J, Hu D, Liang L, Guo M, Fenton B, Okunieff P, Ding I (2003) Combination of radiation and celebrex (celecoxib) reduce mammary and lung tumor growth. Am J Clin Oncol 26:S103–S109
Amirghahari N, Harrison L, Smith M, Rong X, Naumann I, Ampil F, Shi R, Glass J, Nathan CA (2003) NS 398 radiosensitizes an HNSCC cell line by possibly inhibiting radiation-induced expression of COX-2. Int J Radiat Oncol Biol Phys 57:1405–1412
Pyo H, Choy H, Amorino GP, Kim JS, Cao Q, Hercules SK, DuBois RN (2001) A selective cyclooxygenase-2 inhibitor, NS-398, enhances the effect of radiation in vitro and in vivo preferentially on the cells that express cyclooxygenase-2. Clin Cancer Res 7:2998–3005
Kishi K, Petersen S, Petersen C, Hunter N, Mason K, Masferrer JL, Tofilon PJ, Milas L (2000) Preferential enhancement of tumor radioresponse by a cyclooxygenase-2 inhibitor. Cancer Res 60:1326–1331
Milas L, Kishi K, Hunter N, Mason K, Masferrer JL, Tofilon PJ (1999) Enhancement of tumor response to gamma-radiation by an inhibitor of cyclooxygenase-2 enzyme. J Natl Cancer Inst 91:1501–1504
Petersen C, Petersen S, Milas L, Lang FF, Tofilon PJ (2000) Enhancement of intrinsic tumor cell radiosensitivity induced by a selective cyclooxygenase-2 inhibitor. Clin Cancer Res 6:2513–2520
Koppe MJ, Soede AC, Pels W, Oyen WJ, Goldenberg DM, Bleichrodt RP, Boerman OC (2003) Experimental radioimmunotherapy of small peritoneal metastases of colorectal origin. Int J Cancer 106:965–972
Koppe MJ, Bleichrodt RP, Soede AC, Verhofstad AA, Goldenberg DM, Oyen WJ, Boerman OC (2004) Biodistribution and therapeutic efficacy of (125/131)I-, (186)Re-, (88/90)Y-, or (177)Lu-labeled monoclonal antibody MN-14 to carcinoembryonic antigen in mice with small peritoneal metastases of colorectal origin. J Nucl Med 45:1224–1232
Shao J, Sheng H, Inoue H, Morrow JD, DuBois RN (2000) Regulation of constitutive cyclooxygenase-2 expression in colon carcinoma cells. J Biol Chem 275:33951–33956
Barden J, Edwards JE, McQuay HJ, Moore RA (2003) Oral valdecoxib and injected parecoxib for acute postoperative pain: a quantitative systematic review. BMC Anesthesiol 3:1
Stichtenoth DO (2004) The second generation of COX-2 inhibitors: clinical pharmacological point of view. Mini Rev Med Chem 4:617–624
Padi SS, Jain NK, Singh S, Kulkarni SK (2004) Pharmacological profile of parecoxib: a novel, potent injectable selective cyclooxygenase-2 inhibitor. Eur J Pharmacol 491:69–76
Cheer SM, Goa KL (2001) Parecoxib (parecoxib sodium). Drugs 61:1133–1141
Talley JJ, Bertenshaw SR, Brown DL, Carter JS, Graneto MJ, Kellogg MS, Koboldt CM, Yuan J, Zhang YY, Seibert K (2000) N-[[(5-methyl-3-phenylisoxazol-4-yl)-phenyl]sulfonyl]propanamide, sodium salt, parecoxib sodium: a potent and selective inhibitor of COX-2 for parenteral administration. J Med Chem 43:1661–1663
O’Donghue GT, Roche-Nagel G, Harmey JH, Bouchier-Hayes DJ (2003) Cyclooxygenase-2 inhibition attenuates surgically induced residual tumour growth and metastases following cytoreductive surgery in a murine model of breast cancer. J Surg Res 114:227
Smakman N, Kranenburg O, Vogten JM, Bloemendaal AL, van Diest P, Borel RI (2005) Cyclooxygenase-2 is a target of KRASD12, which facilitates the outgrowth of murine C26 colorectal liver metastases. Clin Cancer Res 11:41–48
Hansen HJ, Goldenberg DM, Newman ES, Grebenau R, Sharkey RM (1993) Characterization of second-generation monoclonal antibodies against carcinoembryonic antigen. Cancer 71:3478–3485
Ey PL, Prowse SJ, Jenkin CR (1978) Isolation of pure IgG1, IgG2a and IgG2b immunoglobulins from mouse serum using protein A-sepharose. Immunochemistry 15:429–436
Lindmo T, Boven E, Cuttitta F, Fedorko J, Bunn PA Jr (1984) Determination of the immunoreactive fraction of radiolabeled monoclonal antibodies by linear extrapolation to binding at infinite antigen excess. J Immunol Methods 72:77–89
Eggermont AM, Steller EP, Sugarbaker PH (1987) Laparotomy enhances intraperitoneal tumor growth and abrogates the antitumor effects of interleukin-2 and lymphokine-activated killer cells. Surgery 102:71–78
Alsalameh S, Burian M, Mahr G, Woodcock BG, Geisslinger G (2003) Review article: the pharmacological properties and clinical use of valdecoxib, a new cyclo-oxygenase-2-selective inhibitor. Aliment Pharmacol Ther 17:489–501
Gierse JK, Zhang Y, Hood WF, Walker MC, Trigg JS, Maziasz TJ, Koboldt CM, Muhammad JL, Zweifel BS, Masferrer JL, Isakson PC, Seibert K (2004) Valdecoxib: assessment of COX-2 potency and selectivity. J Pharmacol Exp Ther 312(3):1206–121
Hood WF, Gierse JK, Isakson PC, Kiefer JR, Kurumbail RG, Seibert K, Monahan JB (2003) Characterization of celecoxib and valdecoxib binding to cyclooxygenase. Mol Pharmacol 63:870–877
Zhang JY, Yuan JJ, Wang YF, Bible RH Jr, Breau AP (2003) Pharmacokinetics and metabolism of a COX-2 inhibitor, valdecoxib, in mice. Drug Metab Dispos 31:491–501
Tsujii M, Kawano S, Tsuji S, Sawaoka H, Hori M, DuBois RN (1998) Cyclooxygenase regulates angiogenesis induced by colon cancer cells. Cell 93:705–716
Rozic JG, Chakraborty C, Lala PK (2001) Cyclooxygenase inhibitors retard murine mammary tumor progression by reducing tumor cell migration, invasiveness and angiogenesis. Int J Cancer 93:497–506
Sawaoka H, Tsuji S, Tsujii M, Gunawan ES, Sasaki Y, Kawano S, Hori M (1999) Cyclooxygenase inhibitors suppress angiogenesis and reduce tumor growth in vivo. Lab Invest 79:1469–1477
Buchsbaum DJ, Roberson PL (1996) Experimental radioimmunotherapy: biological effectiveness and comparison with external beam radiation. Recent Results Cancer Res 141:9–18
Acknowledgments
Part of this study was supported by a grant from the Netherlands Organization for Health Research and Development (ZonMw); Grant number: 920-03-220. The authors wish to thank Mr Hennie Eikholt, animal technician, for technical assistance during the experiments, and Ms. Anneke Voss, for her help in the histopathological examination.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koppe, M.J., Oyen, W.J.G., Bleichrodt, R.P. et al. Combination therapy using the cyclooxygenase-2 inhibitor Parecoxib and radioimmunotherapy in nude mice with small peritoneal metastases of colonic origin. Cancer Immunol Immunother 55, 47–55 (2006). https://doi.org/10.1007/s00262-005-0704-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-005-0704-3