Abstract
Purpose
Loss of brain synapses is an early pathological feature of Alzheimer’s disease. The current study assessed synaptic loss in vivo with positron emission tomography and an 18F-labelled radiotracer of the synaptic vesicle protein 2A, [18F]UCB-H.
Methods
Twenty-four patients with mild cognitive impairment or Alzheimer’s disease and positive [18F]Flutemetamol amyloid-PET were compared to 19 healthy controls. [18F]UCB-H brain uptake was quantified with Logan graphical analysis using an image-derived blood input function. SPM12 and regions-of-interest (ROI) analyses were used for group comparisons of regional brain distribution volumes and for correlation with cognitive measures.
Results
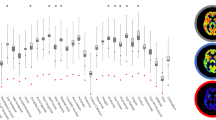
A significant decrease of [18F]UCB-H uptake was observed in several cortical areas (11 to 18% difference) and in the thalamus (16% difference), with the largest effect size in the hippocampus (31% difference). Reduced hippocampal uptake was related to patients’ cognitive decline (ROI analysis) and unawareness of memory problems (SPM and ROI analyses).
Conclusions
The findings thus highlight predominant synaptic loss in the hippocampus, confirming previous autopsy-based studies and a recent PET study with an 11C-labelled SV2A radiotracer. [18F]UCB-H PET allows to image in vivo synaptic changes in Alzheimer’s disease and to relate them to patients’ cognitive impairment.





Similar content being viewed by others
Notes
Signal from the two carotids was used to increase the quality of the data, but distribution volumes obtained by considering the signal from the left and right carotid independently were highly similar (left/right ratio = 0.99 ± 0.05) and each was also highly similar to the distribution volume considering the two carotids together (left/total ratio, 0.99 ± 0.01; right/total ratio, 0.99 ± 0.04).
References
Terry RD, Masliah E, Salmon DP, Butters N, DeTeresa R, Hill R, et al. Physical basis of cognitive alterations in Alzheimer’s disease: synapse loss is the major correlate of cognitive impairment. Ann Neurol. 1991;30:572–80. https://doi.org/10.1002/ana.410300410.
Scheff SW, Price DA, Schmitt FA, Mufson EJ. Hippocampal synaptic loss in early Alzheimer’s disease and mild cognitive impairment. Neurobiol Aging. 2006;27:1372–84. https://doi.org/10.1016/j.neurobiolaging.2005.09.012.
Honer W. Pathology of presynaptic proteins in Alzheimer’s disease: more than simple loss of terminals. Neurobiol Aging. 2003;24:1047–62. https://doi.org/10.1016/j.neurobiolaging.2003.04.005.
de Wilde MC, Overk CR, Sijben JW, Masliah E. Meta-analysis of synaptic pathology in Alzheimer’s disease reveals selective molecular vesicular machinery vulnerability. Alzheimers Dement. 2016;12:633–44. https://doi.org/10.1016/j.jalz.2015.12.005.
Schmitz TW, Nathan Spreng R. Alzheimer’s disease neuroimaging I. Basal forebrain degeneration precedes and predicts the cortical spread of Alzheimer’s pathology. Nat Commun. 2016;7:13249. https://doi.org/10.1038/ncomms13249.
Counts SE, Nadeem M, Lad SP, Wuu J, Mufson EJ. Differential expression of synaptic proteins in the frontal and temporal cortex of elderly subjects with mild cognitive impairment. J Neuropathol Exp Neurol. 2006;65:592–601.
Counts SE, He B, Nadeem M, Wuu J, Scheff SW, Mufson EJ. Hippocampal drebrin loss in mild cognitive impairment. Neurodegener Dis. 2012;10:216–9. https://doi.org/10.1159/000333122.
Scheff SW, Price DA, Ansari MA, Roberts KN, Schmitt FA, Ikonomovic MD, et al. Synaptic change in the posterior cingulate gyrus in the progression of Alzheimer’s disease. J Alzheimers Dis. 2015;43:1073–90. https://doi.org/10.3233/JAD-141518.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–9. https://doi.org/10.1016/j.jalz.2011.03.005.
Nabulsi NB, Mercier J, Holden D, Carre S, Najafzadeh S, Vandergeten MC, et al. Synthesis and preclinical evaluation of 11C-UCB-J as a PET tracer for imaging the synaptic vesicle glycoprotein 2A in the brain. J Nucl Med. 2016;57:777–84. https://doi.org/10.2967/jnumed.115.168179.
Estrada S, Lubberink M, Thibblin A, Sprycha M, Buchanan T, Mestdagh N, et al. [(11)C]UCB-A, a novel PET tracer for synaptic vesicle protein 2A. Nucl Med Biol. 2016;43:325–32. https://doi.org/10.1016/j.nucmedbio.2016.03.004.
Warnock GI, Aerts J, Bahri MA, Bretin F, Lemaire C, Giacomelli F, et al. Evaluation of 18F-UCB-H as a novel PET tracer for synaptic vesicle protein 2A in the brain. J Nucl Med. 2014;55:1336–41. https://doi.org/10.2967/jnumed.113.136143.
Elferink LA, Scheller RH. Synaptic vesicle proteins and regulated exocytosis. Prog Brain Res. 1995;105:79–85.
Robinson JL, Molina-Porcel L, Corrada MM, Raible K, Lee EB, Lee VM, et al. Perforant path synaptic loss correlates with cognitive impairment and Alzheimer’s disease in the oldest-old. Brain. 2014;137:2578–87. https://doi.org/10.1093/brain/awu190.
Chen M, Mecca AP, Naganawa M, et al. Assessing synaptic density in alzheimer disease with synaptic vesicle glycoprotein 2a positron emission tomographic imaging. JAMA Neurol. 2018. https://doi.org/10.1001/jamaneurol.2018.1836.
Mormino EC, Jagust WJ. A new tool for clinical neuroscience—synaptic imaging. JAMA Neurol. 2018. https://doi.org/10.1001/jamaneurol.2018.1643.
Becker G, Warnier C, Serrano ME, Bahri MA, Mercier J, Lemaire C, et al. Pharmacokinetic characterization of [(18)F]UCB-H PET radiopharmaceutical in the rat brain. Mol Pharm. 2017;14:2719–25. https://doi.org/10.1021/acs.molpharmaceut.7b00235.
Bretin F, Bahri MA, Bernard C, Warnock G, Aerts J, Mestdagh N, et al. Biodistribution and radiation dosimetry for the novel SV2A radiotracer [(18)F]UCB-H: first-in-human study. Mol Imaging Biol. 2015;17:557–64. https://doi.org/10.1007/s11307-014-0820-6.
Bahri MA, Plenevaux A, Aerts J, Bastin C, Becker G, Mercier J, et al. Measuring brain synaptic vesicle protein 2A with positron emission tomography and [(18)F]UCB-H. Alzheimers Dement (N Y). 2017;3:481–6. https://doi.org/10.1016/j.trci.2017.08.004.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270–9. https://doi.org/10.1016/j.jalz.2011.03.008.
Jack CR Jr, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14:535–62. https://doi.org/10.1016/j.jalz.2018.02.018.
Didic M, Ranjeva JP, Barbeau E, Confort-Gouny S, Fur YL, Felician O, et al. Impaired visual recognition memory in amnestic mild cognitive impairment is associated with mesiotemporal metabolic changes on magnetic resonance spectroscopic imaging. J Alzheimers Dis. 2010;22:1269–79. https://doi.org/10.3233/JAD-2010-101257.
Migliorelli R, Teson A, Sabe L, Petracca G, Petracchi M, Leiguarda R, et al. Anosognosia in Alzheimer’s disease: a study of associated factors. J Neuropsychiatry Clin Neurosci. 1995;7:338–44.
Clare L, Wilson BA, Carter G, Roth I, Hodges JR. Assessing awareness in early-stage Alzheimer’s disease: development and piloting of the memory awareness rating scale. Neuropsychol Rehabil. 2002;12:341–62.
Cacciamani F, Tandetnik C, Gagliardi G, Bertin H, Habert MO, Hampel H, et al. Low cognitive awareness, but not complaint, is a good marker of preclinical Alzheimer’s disease. J Alzheimers Dis. 2017;59:753–62. https://doi.org/10.3233/JAD-170399.
Warnier C, Lemaire C, Becker G, Zaragoza G, Giacomelli F, Aerts J, et al. Enabling efficient positron emission tomography (PET) imaging of synaptic vesicle glycoprotein 2A (SV2A) with a robust and one-step radiosynthesis of a highly potent 18F-labeled ligand ([18F]UCB-H). J Med Chem. 2016;59:8955–66. https://doi.org/10.1021/acs.jmedchem.6b00905.
Draganski B, Ashburner J, Hutton C, Kherif F, Frackowiak RS, Helms G, et al. Regional specificity of MRI contrast parameter changes in normal ageing revealed by voxel-based quantification (VBQ). Neuroimage. 2011;55:1423–34. https://doi.org/10.1016/j.neuroimage.2011.01.052.
Ashburner J, Friston KJ. Unified segmentation. Neuroimage. 2005;26:839–51. https://doi.org/10.1016/j.neuroimage.2005.02.018.
Erlandsson K, Buvat I, Pretorius PH, Thomas BA, Hutton BF. A review of partial volume correction techniques for emission tomography and their applications in neurology, cardiology and oncology. Phys Med Biol. 2012;57:R119–R59. https://doi.org/10.1088/0031-9155/57/21/r119.
Thomas BA, Cuplov V, Bousse A, Mendes A, Thielemans K, Hutton BF, et al. PETPVC: a toolbox for performing partial volume correction techniques in positron emission tomography. Phys Med Biol. 2016;61:7975–93. https://doi.org/10.1088/0031-9155/61/22/7975.
Salinas CA, Searle GE, Gunn RN. The simplified reference tissue model: model assumption violations and their impact on binding potential. J Cereb Blood Flow Metab. 2015;35:304–11. https://doi.org/10.1038/jcbfm.2014.202.
Wahlund LO, Barkhof F, Fazekas F, Bronge L, Augustin M, Sjogren M, et al. A new rating scale for age-related white matter changes applicable to MRI and CT. Stroke. 2001;32:1318–22.
Schain M, Benjaminsson S, Varnäs K, Forsberg A, Halldin C, Lansner A, et al. Arterial input function derived from pairwise correlations between PET-image voxels. J Cereb Blood Flow Metab. 2013;33:1058–65. https://doi.org/10.1038/jcbfm.2013.47.
Rousset OG, Ma Y, Evans AC. Correction for partial volume effects in PET: principle and validation. J Nucl Med. 1998;39:904–11.
Krauth A, Blanc R, Poveda A, Jeanmonod D, Morel A, Székely G. A mean three-dimensional atlas of the human thalamus: generation from multiple histological data. Neuroimage. 2010;49:2053–62. https://doi.org/10.1016/j.neuroimage.2009.10.042.
Zaborszky L, Hoemke L, Mohlberg H, Schleicher A, Amunts K, Zilles K. Stereotaxic probabilistic maps of the magnocellular cell groups in human basal forebrain. Neuroimage. 2008;42:1127–41. https://doi.org/10.1016/j.neuroimage.2008.05.055.
Garibotto V, Tettamanti M, Marcone A, Florea I, Panzacchi A, Moresco R, et al. Cholinergic activity correlates with reserve proxies in Alzheimer’s disease. Neurobiol Aging. 2013;34:2694 e13–8. https://doi.org/10.1016/j.neurobiolaging.2013.05.020.
Thomas BA, Erlandsson K, Modat M, Thurfjell L, Vandenberghe R, Ourselin S, et al. The importance of appropriate partial volume correction for PET quantification in Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2011;38:1104–19. https://doi.org/10.1007/s00259-011-1745-9.
Kepe V, Barrio JR, Huang SC, Ercoli L, Siddarth P, Shoghi-Jadid K, et al. Serotonin 1A receptors in the living brain of Alzheimer’s disease patients. Proc Natl Acad Sci U S A. 2006;103:702–7. https://doi.org/10.1073/pnas.0510237103.
Liu AK, Chang RC, Pearce RK, Gentleman SM. Nucleus basalis of Meynert revisited: anatomy, history and differential involvement in Alzheimer’s and Parkinson’s disease. Acta Neuropathol. 2015;129:527–40. https://doi.org/10.1007/s00401-015-1392-5.
Aggleton JP. Multiple anatomical systems embedded within the primate medial temporal lobe: implications for hippocampal function. Neurosci Biobehav Rev. 2012;36:1579–96. https://doi.org/10.1016/j.neubiorev.2011.09.005.
Johansen-Berg H, Behrens TE, Sillery E, Ciccarelli O, Thompson AJ, Smith SM, et al. Functional-anatomical validation and individual variation of diffusion tractography-based segmentation of the human thalamus. Cereb Cortex. 2005;15:31–9. https://doi.org/10.1093/cercor/bhh105.
Morris RG, Mograbi DC. Anosognosia, autobiographical memory and self knowledge in Alzheimer’s disease. Cortex. 2013;49:1553–65.
Leech R, Sharp DJ. The role of the posterior cingulate cortex in cognition and disease. Brain. 2014;137:12–32. https://doi.org/10.1093/brain/awt162.
Funding
This work was supported by grants from Belgian Interuniversity Attraction Pole (IUAP 7/11), ULiege Research Concerted Action (ARC 12/17-01), Special Research Funds classical grant 2016 (Faculty of Medicine, University of Liege, Belgium), FRS-FNRS. Patient selection was supported by an Investigator Sponsored Study (ISS290) from GE Healthcare for [18F]flutemetamol delivery, and the Walloon Region Public Private Partnership NeuroCom, with the ULiege and UCB Pharma as partners. A. Plenevaux is a research director and C. Bastin is a research associate at the FRS-FNRS Belgium. We thank Nicolas Antoine for providing [18F]flutemetamol data, Lola Danet for help with localization of thalamic nuclei in Morel’s atlas and Roland Hustinx and Claire Bernard (Liege University Hospital) for providing [18F]FDG-PET images.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (Ethics Committee of the Liege University Hospital, reference number EudraCT 2014–000286-50) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurology
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Bastin, C., Bahri, M.A., Meyer, F. et al. In vivo imaging of synaptic loss in Alzheimer’s disease with [18F]UCB-H positron emission tomography. Eur J Nucl Med Mol Imaging 47, 390–402 (2020). https://doi.org/10.1007/s00259-019-04461-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-04461-x