Abstract
Purpose
Given the bone tropism of prostate cancer, conventional imaging modalities poorly identify or quantify metastatic disease. 89Zr-huJ591 positron emission tomography (PET) imaging was performed in patients with metastatic prostate cancer to analyze and validate this as an imaging biomarker for metastatic disease. The purpose of this initial study was to assess safety, biodistribution, normal organ dosimetry, and optimal imaging time post-injection for lesion detection.
Methods
Ten patients with metastatic prostate cancer received 5 mCi of 89Zr-huJ591. Four whole-body scans with multiple whole-body count rate measurements and serum activity concentration measurements were obtained in all patients. Biodistribution, clearance, and lesion uptake by 89Zr-huJ591 immuno-PET imaging was analyzed and dosimetry was estimated using MIRD techniques. Initial assessment of lesion targeting of 89Zr-huJ591 was done. Optimal time for imaging post-injection was determined.
Results
The dose was well tolerated with mild chills and rigors seen in two patients. The clearance of 89Zr-huJ591 from serum was bi-exponential with biological half-lives of 7 ± 4.5 h (range 1.1–14 h) and 62 ± 13 h (range 51–89 h) for initial rapid and later slow phase. Whole-body biological clearance was 219 ± 48 h (range 153–317 h). The mean whole-body and liver residence time was 78.7 and 25.6 h, respectively. Dosimetric estimates to critical organs included liver 7.7 ± 1.5 cGy/mCi, renal cortex 3.5 ± 0.4 cGy/mCi, and bone marrow 1.2 ± 0.2 cGy/mCi. Optimal time for patient imaging after injection was 7 ± 1 days. Lesion targeting of bone or soft tissue was seen in all patients. Biopsies were performed in 8 patients for a total 12 lesions, all of which were histologically confirmed as metastatic prostate cancer. One biopsy-proven lesion was not positive on 89Zr-huJ591, while the remaining 11 lesions were 89Zr-huJ591 positive. Two biopsy-positive nodal lesions were noted only on 89Zr-huJ591 study, while the conventional imaging modality was negative.
Conclusion
89Zr-huJ591 PET imaging of prostate-specific membrane antigen expression is safe and shows good localization of disease in prostate cancer patients. Liver is the critical organ for dosimetry, and 7 ± 1 days is the optimal imaging time. A larger study is underway to determine lesion detection in an expanded cohort of patients with metastatic prostate cancer.





Similar content being viewed by others
References
Kiess AP, Cho SY, Pomper MG. Translational molecular imaging of prostate cancer. Curr Radiol Rep 2013;1(3):216–26.
Morris MJ, Autio KA, Basch EM, Danila DC, Larson S, Scher HI. Monitoring the clinical outcomes in advanced prostate cancer: what imaging modalities and other markers are reliable? Semin Oncol 2013;40(3):375–92.
Haseebuddin M, Dehdashti F, Siegel BA, Liu J, Roth EB, Nepple KG, et al. 11C-acetate PET/CT before radical prostatectomy: nodal staging and treatment failure prediction. J Nucl Med 2013;54(5):699–706.
Schuster DM, Nieh PT, Jani AB, Amzat R, Bowman FD, Halkar RK, et al. Anti-3-[(18)F]FACBC positron emission tomography-computerized tomography and (111)In-capromab pendetide single photon emission computerized tomography-computerized tomography for recurrent prostate carcinoma: results of a prospective clinical trial. J Urol 2014;191(5):1446–53.
Schroeder RP, van Weerden WM, Krenning EP, Bangma CH, Bemdsen S, Grievink-de Ligt CH, et al. Gastrin-releasing peptide receptor-based targeting using bombesin analogues is superior to metabolism-based targeting using choline for in vivo imaging of human prostate cancer xenografts. Eur J Nucl Med Mol Imaging 2011;38(7):1257–66.
Nanda PK, Pandey U, Bottenus BN, Rold TL, Sieckman GL, Szczodroski AF, et al. Bombesin analogues for gastrin-releasing peptide receptor imaging. Nucl Med Biol 2012;39(4):461–71.
Eder M, Eisenhut M, Babich J, Haberkorn U. PSMA as a target for radiolabelled small molecules. Eur J Nucl Med Mol Imaging 2013;40(6):819–23.
Carlucci G, Ananias HJ, Yu Z, Hoving HD, Helfrich W, Diercks RA, et al. Preclinical evaluation of a novel (111)In-labeled bombesin homodimer for improved imaging of GRPR-positive prostate cancer. Mol Pharm 2013;10(5):1716–24.
Pan D, Xu YP, Yang RH, Wang L, Chen F, Luo S, et al. A new (68)Ga-labeled BBN peptide with a hydrophilic linker for GRPR-targeted tumor imaging. Amino Acids 2014;46:1481–9.
Murphy GP, Elgamal AA, Su SL, Bostwick DG, Holmes EH. Current evaluation of the tissue localization and diagnostic utility of prostate specific membrane antigen. Cancer 1998;83(11):2259–69.
Bostwick DG, Pacelli A, Blute M, Roche P, Murphy GP. Prostate specific membrane antigen expression in prostatic intraepithelial neoplasia and adenocarcinoma: a study of 184 cases. Cancer 1998;82(11):2256–61.
Haffner MC, Kronberger IE, Ross JS, Sheehan CE, Zitt M, Mühlmann G, et al. Prostate-specific membrane antigen expression in the neovasculature of gastric and colorectal cancers. Hum Pathol 2009;40(12):1754–61.
Bander NH, Trabulsi EJ, Kostakoglu L, Yao D, Vallabhajosula S, Smith-Jones P, et al. Targeting metastatic prostate cancer with radiolabeled monoclonal antibody J591 to the extracellular domain of prostate specific membrane antigen. J Urol 2003;170(5):1717–21.
Bander NH, Nanus DM, Milowsky MI, Kostakoglu L, Vallabahajosula S, Goldsmith SJ. Targeted systemic therapy of prostate cancer with a monoclonal antibody to prostate-specific membrane antigen. Semin Oncol 2003;30(5):667–77.
Liu H, Rajasekaran AK, Moy P, Xia Y, Kim S, Navarro V, et al. Constitutive and antibody-induced internalization of prostate-specific membrane antigen. Cancer Res 1998;58(18):4055–60.
Pandit-Taskar N, O’Donoghue JA, Morris MJ, Wills EA, Schwartz LH, Gonen M, et al. Antibody mass escalation study in patients with castration-resistant prostate cancer using (111)In-J591: lesion detectability and dosimetric projections for (90)Y radioimmunotherapy. J Nucl Med 2008;49(7):1066–74.
Morris MJ, Pandit-Taskar N, Divgi CR, Bender S, O’Donoghue JA, Nacca A, et al. Phase I evaluation of J591 as a vascular targeting agent in progressive solid tumors. Clin Cancer Res 2007;13(9):2707–13.
Morris MJ, Divgi CR, Pandit-Taskar N, Batraki M, Warren N, Nacca A, et al. Pilot trial of unlabeled and indium-111-labeled anti-prostate-specific membrane antigen antibody J591 for castrate metastatic prostate cancer. Clin Cancer Res 2005;11(20):7454–61.
Milowsky MI, Nanus DM, Kostakoglu L, Vallabhajosula S, Goldsmith SJ, Bander NH. Phase I trial of yttrium-90-labeled anti-prostate-specific membrane antigen monoclonal antibody J591 for androgen-independent prostate cancer. J Clin Oncol 2004;22(13):2522–31.
Trabulsi EJ, Yao D, Joyce MA, et al. Phase I radioimmunotherapy (RIT) trials of monoclonal antibody (mAb) J591 to the extracellular domain of prostate specific membrane antigen (PSMA(ext)) radiolabeled with (90)yttrium (Y-90) or (177)lutetium (Lu-177) in advanced prostate cancer (Pca). J Urol 2003;169(4):396–7.
Nanus DM, Milowsky MI, Kostakoglu L, Smith-Jones PM, Vallabahajosula S, Goldsmith SJ, et al. Clinical use of monoclonal antibody HuJ591 therapy: targeting prostate specific membrane antigen. J Urol 2003;170(6):S84–8.
Holland JP, Sheh Y, Lewis JS. Standardized methods for the production of high specific-activity zirconium-89. Nucl Med Biol 2009;36(7):729–39.
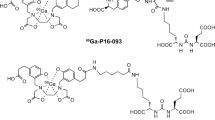
Vosjan MJ, Perk LR, Visser GW, Budde M, Jurek P, Kiefer GE, et al. Conjugation and radiolabeling of monoclonal antibodies with zirconium-89 for PET imaging using the bifunctional chelate p-isothiocyanatobenzyl-desferrioxamine. Nat Protoc 2010;5(4):739–43.
Holland JP, Divilov V, Bander NH, Smith-Jones PM, Larson SM, Lewis JS. 89Zr-DFO-J591 for immunoPET of prostate-specific membrane antigen expression in vivo. J Nucl Med 2010;51(8):1293–300.
Lindmo T, Boven E, Cuttitta F, Fedorko J, Bunn Jr PA. Determination of the immunoreactive fraction of radiolabeled monoclonal antibodies by linear extrapolation to binding at infinite antigen excess. J Immunol Methods 1984;72(1):77–89.
Morris MJ, Pandit-Taskar N, Carrasquillo JA, O’Donoghue JA, Humm J, Serge K, et al. Phase I trial of zirconium 89 (Zr89) radiolabeled J591 in metastatic castration-resistant prostate cancer (mCRPC). J Clin Oncol 2013;31(Suppl 6; abstract 31).
Pandit-Taskar N, O’Donoghue J, et al. 89Zr J591 immunoPET imaging in patients with prostate cancer. J Nucl Med 2013;54(Suppl 2):287.
Lutje S, Boerman OC, van Rij CM, Sedelaar M, Helfrich W, Oyen WJ, et al. Prospects in radionuclide imaging of prostate cancer. Prostate 2012;72(11):1262–72.
Yu Z, Carlucci G, Ananias HJ, Dierckx RA, Liu S, Helfrich W, et al. Evaluation of a technetium-99m labeled bombesin homodimer for GRPR imaging in prostate cancer. Amino Acids 2013;44(2):543–53.
Castellucci P, Picchio M. 11C-choline PET/CT and PSA kinetics. Eur J Nucl Med Mol Imaging 2013;40 Suppl 1:S36–40.
Ceci F, Castellucci P, Mamede M, Schiavina R, Rubello D, Fuccio C, et al. (11)C-Choline PET/CT in patients with hormone-resistant prostate cancer showing biochemical relapse after radical prostatectomy. Eur J Nucl Med Mol Imaging 2013;40(2):149–55.
Ceci F, Schiavina R, Castellucci P, Brunocilla E, Fuccio C, Colletti PM, et al. 11C-choline PET/CT scan in patients with prostate cancer treated with intermittent ADT: a sequential PET/CT study. Clin Nucl Med 2013;38(7):e279–82.
Nanni C, Schiavina R, Brunocilla E, Borghesi M, Ambrosini V, Zanoni L, et al. 18F-FACBC compared with 11C-choline PET/CT in patients with biochemical relapse after radical prostatectomy: a prospective study in 28 patients. Clin Genitourin Cancer 2014;12(2):106–10.
Turkbey B, Mena E, Shih J, Pinto PA, Merino MJ, Lindenberg ML, et al. Localized prostate cancer detection with 18F FACBC PET/CT: comparison with MR imaging and histopathologic analysis. Radiology 2014;270(3):849–56.
Nye JA, Schuster DM, Yu W, Camp VM, Goodman MM, Votaw JR. Biodistribution and radiation dosimetry of the synthetic nonmetabolized amino acid analogue anti-18F-FACBC in humans. J Nucl Med 2007;48(6):1017–20.
Cho SY, Gage KL, Mease RC, Senthamizhchelvan S, Holt DP, Jeffrey-Kwanisai A, et al. Biodistribution, tumor detection, and radiation dosimetry of 18F-DCFBC, a low-molecular-weight inhibitor of prostate-specific membrane antigen, in patients with metastatic prostate cancer. J Nucl Med 2012;53(12):1883–91.
Wieser G, Mansi R, Grosu AL, Schultze-Seemann W, Dumont-Walter RA, Meyer PT, et al. Positron emission tomography (PET) imaging of prostate cancer with a gastrin releasing peptide receptor antagonist–from mice to men. Theranostics 2014;4(4):412–9.
Dijkgraaf I, Franssen GM, McBride WJ, D’Souza CA, Laverman P, Smith CJ, et al. PET of tumors expressing gastrin-releasing peptide receptor with an 18F-labeled bombesin analog. J Nucl Med 2012;53(6):947–52.
Abiraj K, Mansi R, Tamma ML, Fani M, Forrer F, Nicolas G, et al. Bombesin antagonist-based radioligands for translational nuclear imaging of gastrin-releasing peptide receptor-positive tumors. J Nucl Med 2011;52(12):1970–8.
Afshar-Oromieh A, Zechmann CM, Malcher A, Eder M, Eisenhut M, Linhart HG, et al. Comparison of PET imaging with a (68)Ga-labelled PSMA ligand and (18)F-choline-based PET/CT for the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging 2014;41(1):11–20.
Zechmann CM, Afshar-Oromieh A, Armor T, Stubbs JB, Mier W, Hadaschik B, et al. Radiation dosimetry and first therapy results with a (124)I/(131)I-labeled small molecule (MIP-1095) targeting PSMA for prostate cancer therapy. Eur J Nucl Med Mol Imaging 2014;41:1280–92.
Hillier SM, Kern AM, Maresca KP, Marquis JC, Eckelman WC, Joyal JL, et al. 123I-MIP-1072, a small-molecule inhibitor of prostate-specific membrane antigen, is effective at monitoring tumor response to taxane therapy. J Nucl Med 2011;52(7):1087–93.
Barrett JA, Coleman RE, Goldsmith SJ, Vallabhajosula S, Petry NA, Cho S, et al. First-in-man evaluation of 2 high-affinity PSMA-avid small molecules for imaging prostate cancer. J Nucl Med 2013;54(3):380–7.
Barrett PH, Bell BM, Cobelli C, Golde H, Schumitzky A, Vicini P, et al. SAAM II: simulation, analysis, and modeling software for tracer and pharmacokinetic studies. Metabolism 1998;47(4):484–92.
Stabin MG, Sparks RB, Crowe E. OLINDA/EXM: the second-generation personal computer software for internal dose assessment in nuclear medicine. J Nucl Med 2005;46(6):1023–7.
Sgouros G, Stabin M, Erdi Y, Akabani G, Kwok C, Brill AB, et al. Red marrow dosimetry for radiolabeled antibodies that bind to marrow, bone, or blood components. Med Phys 2000;27(9):2150–64.
Acknowledgments
Starr Cancer Consortium, Prostate cancer program of MSKCC and Center for Targeted Radioimmunotherapy and Diagnosis of the Ludwig Center for Cancer Immunotherapy, David H. Koch Foundation, R21 CA153177-03. RMPIC core is supported in part by NIH P30CA008748, the Landy Research Fund, and Hascoe Charitable Foundation.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Neeta Pandit-Taskar and Joseph A. O’Donoghue are co-first authors
Michael J. Morris and Steven M. Larson are co-last authors
Rights and permissions
About this article
Cite this article
Pandit-Taskar, N., O’Donoghue, J.A., Beylergil, V. et al. 89Zr-huJ591 immuno-PET imaging in patients with advanced metastatic prostate cancer. Eur J Nucl Med Mol Imaging 41, 2093–2105 (2014). https://doi.org/10.1007/s00259-014-2830-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-014-2830-7