Abstract
Purpose
68Ga-labelled HBED-CC-PSMA is a highly promising tracer for imaging recurrent prostate cancer (PCa). The intention of this study was to evaluate the feasibility of PET/MRI with this tracer.
Methods
Twenty patients underwent PET/CT 1 h after injection of the 68Ga-PSMA ligand followed by PET/MRI 3 h after injection. Data from the two investigations were first analysed separately and then compared with respect to tumour detection rate and radiotracer uptake in various tissues. To evaluate the quantification accuracy of the PET/MRI system, differences in SUVs between PET/CT and corresponding PET/MRI were compared with differences in SUVs between PET/CT 1 h and 3 h after injection in another patient cohort. This cohort was investigated using the same PET/CT system.
Results
With PET/MRI, different diagnostic sequences, higher contrast of lesions and higher resolution of MRI enabled a subjectively easier evaluation of the images. In addition, four unclear findings on PET/CT could be clarified as characteristic of PCa metastases by PET/MRI. However, in PET images of the PET/MRI, a reduced signal was observed at the level of the kidneys (in 11 patients) and around the urinary bladder (in 15 patients). This led to reduced SUVs in six lesions. SUVmean values provided by the PET/MRI system were different in muscles, blood pool, liver and spleen.
Conclusion
PCa was detected more easily and more accurately with Ga-PSMA PET/MRI than with PET/CT and with lower radiation exposure. Consequently, this new technique could clarify unclear findings on PET/CT. However, scatter correction was challenging when the specific 68Ga-PSMA ligand was used. Moreover, direct comparison of SUVs from PET/CT and PET/MR needs to be conducted carefully.






Similar content being viewed by others
References
Jemal A, Bray F, Centre MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Kosuri S, Akhtar NH, Smith M, Osborne JR, Tagawa ST. Review of salvage therapy for biochemically recurrent prostate cancer: the role of imaging and rationale for systemic salvage targeted anti-prostate-specific membrane antigen radioimmunotherapy. Adv Urol. 2012;2012:921674.
Kularatne SA, Zhou Z, Yang J, Post CB, Low PS. Design, synthesis, and preclinical evaluation of prostate-specific membrane antigen targeted (99m)Tc-radioimaging agents. Mol Pharm. 2009;6:790–800.
Chen Y, Pullambhatla M, Byun Y, Foss CA, Nimmagadda S, Senthamizhchelvan S, et al. 2-(3-{1-Carboxy-5-[(6-[18F]fluoro-pyridine-3-carbonyl)-amino]-pentyl}-ureido)-pentanedioic acid, [18F]DCFPyL, a PSMA-based PET imaging agent for prostate cancer. Clin Cancer Res. 2011;17:7645–53.
Hillier SM, Kern AM, Maresca KP, Marquis JC, Eckelman WC, Joyal JL, et al. 123I-MIP-1072, a small-molecule inhibitor of prostate-specific membrane antigen, is effective at monitoring tumor response to taxane therapy. J Nucl Med. 2011;52:1087–93.
Hillier S, Rubino K, Maresca K, Marquis J, Tesson M, Zimmerman C, et al. [131I]MIP-1466, a small molecule prostate-specific membrane antigen (PSMA) inhibitor for targeted radiotherapy of prostate cancer (PCAa). J Nucl Med. 2012;53 Suppl 1:170.
Eder M, Eisenhut M, Babich J, Haberkorn U. PSMA as a target for radiolabelled small molecules. Eur J Nucl Med Mol Imaging. 2013;40:819–23.
Afshar-Oromieh A, Haberkorn U, Eder M, Eisenhut M, Zechmann C. [68Ga]Gallium-labelled PSMA-ligand as superior PET tracer for the diagnosis of prostate cancer: comparison with 18F-FECH. Eur J Nucl Med Mol Imaging. 2012;39:1085–6.
Afshar-Oromieh A, Malcher A, Eder M, Eisenhut M, Linhart HG, Hadaschik BA, et al. PET imaging with a [68Ga]gallium-labelled PSMA ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur J Nucl Med Mol Imaging. 2013;40:486–95.
Afshar-Oromieh A, Haberkorn U, Hadaschik B, Habl G, Eder M, Eisenhut M, et al. PET/MRI with a 68Ga-PSMA ligand for the detection of prostate cancer. Eur J Nucl Med Mol Imaging. 2013;40:1629–30.
Afshar-Oromieh A, Zechmann CM, Malcher A, Eder M, Eisenhut M, Linhart HG et al. Comparison of PET imaging with a 68Ga-labelled PSMA-ligand and 18F-Choline based PET/CT for the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2014;41:11–20.
Lord M, Ratib O, Vallée JP. 18F-Fluorocholine integrated PET/MRI for the initial staging of prostate cancer. Eur J Nucl Med Mol Imaging. 2011;38(12):2288.
Park H, Wood D, Hussain H, Meyer CR, Shah RB, Johnson TD, et al. Introducing parametric fusion PET/MRI of primary prostate cancer. J Nucl Med. 2012;53(4):546–51.
Jambor I, Borra R, Kemppainen J, Lepomäki V, Parkkola R, Dean K, et al. Improved detection of localized prostate cancer using co-registered MRI and 11C-acetate PET/CT. Eur J Radiol. 2012;81(11):2966–72.
Arce-Calisaya P, Souvatzoglou M, Eiber M, Beer A, Scheidhauer K, Geinitz H, et al. Sensitivity of PET/MRI to detect recurrence of prostate cancer. Eur J Nucl Med Mol Imaging. 2013;40(5):799.
Wetter A, Lipponer C, Nensa F, Beiderwellen K, Olbricht T, Rübben H, et al. Simultaneous 18F choline positron emission tomography/magnetic resonance imaging of the prostate: initial results. Invest Radiol. 2013;48(5):256–62.
Heinisch M, Dirisamer A, Loidl W, Stoiber F, Gruy B, Haim S, et al. Positron emission tomography/computed tomography with F-18-fluorocholine for restaging of prostate cancer patients: meaningful at PSA < 5 ng/ml? Mol Imaging Biol. 2006;8:43–8.
Cimitan M, Bortolus R, Morassut S, Canzonieri V, Garbeglio A, Baresic T, et al. 18F-Fluorocholine PET/CT imaging for the detection of recurrent prostate cancer at PSA relapse: experience in 100 consecutive patients. Eur J Nucl Med Mol Imaging. 2006;33:1387–98.
Vees H, Buchegger F, Albrecht S, Khan H, Husarik D, Zaidi H, et al. 18F-Choline and/or 11C-acetate positron emission tomography: detection of residual or progressive subclinical disease at very low prostate-specific antigen values (<1 ng/ml) after radical prostatectomy. BJU Int. 2007;99:1415–20.
Pelosi E, Arena V, Skanjeti A, Pirro V, Douroukas A, Pupi A, et al. Role of whole-body 18F-choline PET/CT in disease detection in patients with biochemical relapse after radical treatment for prostate cancer. Radiol Med. 2008;113:895–904.
Steiner C, Vees H, Zaidi H, Wissmeyer M, Berrebi O, Kossovsky MP, et al. Three-phase 18F-fluorocholine PET/CT in the evaluation of prostate cancer recurrence. Nuklearmedizin. 2009;48:1–9.
Eder M, Schäfer M, Bauder-Wüst U, Hull WE, Wängler C, Mier W, et al. (68)Ga-complex lipophilicity and the targeting property of a urea-based PSMA inhibitor for PET imaging. Bioconjug Chem. 2012;23:688–97.
Schäfer M, Bauder-Wüst U, Leotta K, Zoller F, Mier W, Haberkorn U, et al. A dimerized urea-based inhibitor of the prostate-specific membrane antigen for 68Ga-PET imaging of prostate cancer. EJNMMI Res. 2012;2:23.
Schwenzer NF, Schraml C, Müller M, Brendle C, Sauter A, Spengler W, et al. Pulmonary lesion assessment: comparison of whole-body hybrid MR/PET and PET/CT imaging – pilot study. Radiology. 2012;264(2):551–8.
Gaertner FC, Beer AJ, Souvatzoglou M, Eiber M, Fürst S, Ziegler SI, et al. Evaluation of feasibility and image quality of 68Ga-DOTATOC positron emission tomography/magnetic resonance in comparison with positron emission tomography/computed tomography in patients with neuroendocrine tumors. Invest Radiol. 2013;48(5):263–72.
Acknowledgments
We wish to express our gratitude to the members of staff Regula Gnirs and Cora Weyrich, and also especially Dr. Henrik Hetzheim and Dr. Clemens Kratochwil.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Fig. 1
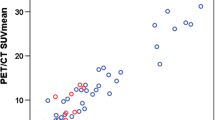
The reliability of SUVs provided by the PET/MRI system was evaluated In a previous study [9] mean SUVs of several tissues were measured using a Siemens Biograph 6 PET/CT system 1 h and 3 h p.i. In the present study, SUVs 1 h p.i. were also measured using the Siemens Biograph 6. The patients were then transferred to a Siemens Biograph mMR PET/MRI system to measure SUV values at 3 h p.i. Differences in the mean SUVs between 1 h and 3 h in the first patient cohort (orange column) were compared to the same values from the patient cohort in the present study (blue column). The results of this analysis are shown in Fig. 5. (JPEG 34 kb)
Fig. 2
PET images with scatter correction (b, e) compared to attenuation-corrected PET images without scatter correction (c, f) in the only patient (patient 8) who showed visually less bright lesions around the urinary bladder. All other patients demonstrated brighter PSMA-positive tissues/lesions on PET images with scatter correction. a Fusion of PET and CT images, d PET image from the PET/CT system, b fusion of PET and MRI (T1 native) images corrected for scatter and attenuation, e MIP image corrected for scatter and attenuation, c fusion of attenuation-corrected PET image without scatter correction and MRI (T1 native) image, f attenuation-corrected MIP image without scatter correction. (JPEG 40 kb)
Fig. 3
Images in patient 8 with a significant halo around the urinary bladder which is clearly visible using extreme windowing in PET images with attenuation and scatter correction (d). Within the halo, SUVs are underestimated as demonstrated by VOIs in muscle inside and outside the halo (d). Extreme windowing can help detect suspicious lesions such as the suspicious lymph node (white arrows). This suspicious lymph node would not have been detected using the automatic windowing. a MR image (T1 with contrast medium and fat saturation) and b PET/MRI fusion image with attenuation and scatter correction as automatically produced by the PET/MRI system; c MR image (T1 with contrast medium and fat saturation) and d PET/MRI fusion image with attenuation and scatter correction with extreme windowing of the PET image. (JPEG 53 kb)
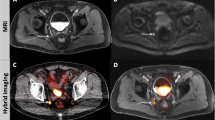
Fig. 4
68Ga-PSMA PET/CT images (a, b) and PET/MRI (c, d) in patient 8. This is another example of the benefits of late PET imaging (improved tracer uptake) compared to MRI (improved anatomical correlation; white arrows lymph node). a CT image without contrast medium, b PET/CT fusion image, c MR image (T1 with contrast medium and fat saturation), d PET/MRI fusion image. (JPEG 54 kb)
Rights and permissions
About this article
Cite this article
Afshar-Oromieh, A., Haberkorn, U., Schlemmer, H.P. et al. Comparison of PET/CT and PET/MRI hybrid systems using a 68Ga-labelled PSMA ligand for the diagnosis of recurrent prostate cancer: initial experience. Eur J Nucl Med Mol Imaging 41, 887–897 (2014). https://doi.org/10.1007/s00259-013-2660-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-013-2660-z