Abstract
Purpose
Renal radiation during peptide receptor radionuclide therapy (PRRT) may result in glomerular damage, a potential reduction of glomerular filtration rate (GFR) and ultimately lead to renal failure. While reported PRRT nephrotoxicity is limited to data derived from serum creatinine—allowing only approximate estimates of GFR—the aim of this study is to accurately determine PRRT-induced long-term changes of renal function and associated risk factors according to state-of-the-art GFR measurement.
Methods
Nephrotoxicity was analysed using 99mTc-diethylenetriaminepentaacetic acid (DTPA) clearance data of 74 consecutive patients with gastroenteropancreatic neuroendocrine tumours (GEP NET) undergoing PRRT with 177Lu-octreotate. The mean follow-up period was 21 months (range 12–50) with a median of five GFR measurements per patient. The change of GFR was analysed by linear curve fit. Potential risk factors including diabetes mellitus, arterial hypertension, previous chemotherapy, renal impairment at baseline and cumulative administered activity were analysed regarding potential impact on renal function loss. In addition, Common Terminology Criteria for Adverse Events (CTCAE) v3.0 were used to compare nephrotoxicity determined by 99mTc-DTPA clearance versus serum creatinine.
Results
The alteration in GFR differed widely among the patients (mean −2.1 ± 13.1 ml/min/m2 per year, relative yearly reduction −1.8 ± 18.9 %). Fifteen patients (21 %) experienced a mild (2–10 ml/min/m2 per year) and 16 patients (22 %) a significant (>10 ml/min/m2 per year) decline of GFR following PRRT. However, 11 patients (15 %) showed an increase of >10 ml/min/m2 per year. Relevant nephrotoxicity according to CTCAE (grade ≥3) was observed in one patient (1.3 %) with arterial hypertension and history of chemotherapy. Nephrotoxicity according to serum creatinine was discordant to that defined by GFR in 15 % of the assessments and led to underestimation in 12 % of patients. None of the investigated factors including cumulative administered activity contributed to the decline of renal function.
Conclusion
Serious nephrotoxicity after PRRT with 177Lu-octreotate is rare (1.3 %). However, slight renal impairment (GFR loss >2 ml/min/m2 per year) can frequently (43 %) be detected by 99mTc-DTPA clearance assessments. Cumulative administered activity of 177Lu-octreotate is not a major determinant of renal impairment in our study.
Similar content being viewed by others
Introduction
Peptide receptor radionuclide therapy (PRRT) with radiolabelled somatostatin analogues is a highly effective systemic treatment in patients with metastatic gastroenteropancreatic neuroendocrine tumours (GEP NET) [1–9]. Kidneys are often the dose-limiting organs and the relatively high radiation dose during PRRT can lead to renal impairment and even end-stage renal disease, particularly after PRRT with 90Y-labelled peptides [10–15].
Renal irradiation arises from the proximal tubular reabsorption of the radiopeptide and the resulting retention in the cortex. Radiation nephropathy after PRRT is mainly due to prominent changes in arteriolar–glomerular area, rather than the tubular epithelium, leading to glomerular sclerosis [16, 17]. PRRT delivers continuous radiation at a relatively low dose rate. It is, therefore, important to observe renal function over a long period of time after PRRT as renal impairment may become clinically evident months after the treatment [13, 16, 18–20]. However, standard measurements such as serum creatinine and creatinine clearance allow only an approximate estimation of the glomerular filtration rate (GFR) and inchoate alterations can only be demonstrated with more sensitive methods such as 99mTc-diethylenetriaminepentaacetic acid (DTPA) or 51Cr-ethylenediaminetetraacetic acid (EDTA) clearance tests [21].
Several strategies to reduce nephrotoxicity in PRRT have been investigated. The coinfusion of positively charged amino acids such as L-lysine and/or L-arginine as competitive inhibitors of proximal tubular reabsorption is currently the established renoprotective regimen in clinical PRRT which may reduce the renal dose ranging from 9 to 53 % [10, 11, 20]. The characteristics of the therapeutic radionuclide may also influence the risk of nephrotoxicity. Due to the lower energy characteristics and the shorter tissue penetration of beta particles, PRRT with 177Lu-labelled peptides may result in a lower radiation dose to the radiosensitive glomeruli and a lower nephrotoxicity compared to that of 90Y-labelled peptides [2, 22–26].
There are only limited data regarding nephrotoxicity after PRRT with 177Lu-octreotate and contributing risk factors. The aim of this study was an accurate assessment of long-term changes in GFR after treatment with 177Lu-octreotate using the 99mTc-DTPA clearance. The impact of potential risk factors, including diabetes mellitus (DM), arterial hypertension (HTN), previous chemotherapy, decreased renal function at baseline, age and cumulative administered activity was of particular interest.
Materials and methods
This retrospective analysis included 74 consecutive patients treated with 177Lu-octreotate at our institution (45 men, 29 women; age range 36–88 years; mean age 61 years). A minimum follow-up of 12 months was required for patient inclusion. Inclusion criteria for treatment with PRRT were histologically confirmed, unresectable, metastatic NET, sufficient tumour uptake, i.e. ≥ liver uptake on baseline receptor imaging, GFR of >30 ml/min/1.73 m2, WBC count ≥2,000/mm3, haemoglobin ≥8 g/dl and platelets ≥75,000/mm3. Twenty-six patients had pancreatic NET (PNET) and 48 patients non-pancreatic GEP NET. The study was performed in accordance with the Declaration of Helsinki and with national regulations. Patients had provided informed consent for the scientific analysis of their data. Approval by the Institutional Review Board is not required for retrospective studies on non-experimental interventions at the authors’ institution. However, explicit approval from the local Ethics Committee was obtained for the prospective and retrospective assessment of outcome of NET patients throughout follow-up in our institution, including this retrospective investigation.
PRRT was performed with a mean of 7.9 GBq (213 mCi) [177Lu-DOTA0,Tyr3]octreotate (177Lu-octreotate) per treatment cycle, aimed at four courses and standard intervals of 3 months (10–14 weeks). The 177Lu (IDB Holland, Baarle-Nassau, The Netherlands) had a specific activity in the approximate range of 100–160 GBq/μmol at the time of administration. The peptide labelling [27, 28] was performed such that an apparent specific activity of about 54 GBq/μmol (ratio of activity to the total amount of peptide) was obtained.
GFR using 99mTc-DTPA clearance test as well as serum creatinine were measured prior to each treatment course, 8–12 weeks after the last course of PRRT and at 3-month intervals in the further follow-up with a median of five measurements per patient. 99mTc-DTPA clearance assessment was performed with a single injection technique after standardized oral hydration using a two-point sampling approach at 1 and 3 h post-injection according to the method of Russell et al. [29]. Toxicity was recorded using the Common Terminology Criteria for Adverse Events v3.0 (CTCAE).
The annual GFR change was analysed by a linear curve fit model. The impact of baseline characteristics of the study population and cumulative administered activity on the renal function loss was examined applying non-parametric tests for independent samples and regression analysis. In addition, multiple logistic regression analysis was performed to identify risk factors for a GFR decrease of >10 ml/min/m2 per year. The statistical software package SPSS (version 20.0, SPSS Inc., Chicago, IL, USA) was used to analyse the data.
Results
The 74 patients underwent 268 PRRT courses with cumulative activities of 177Lu-octreotate ranging between 14.8 and 37.8 GBq. The baseline GFR (pretreatment) was 80 ± 23 ml/min/1.73 m2. The median follow-up period was 21 months (95 % confidence interval 12–50). Significant (≥ grade 3) renal toxicity according to CTCAE was observed in only one patient (79 years old, CTCAE grade 3) with a baseline GFR of 40 ml/min/1.73 m2, history of chemotherapy and arterial HTN almost 13 months after the start of PRRT. The patient had received a total of 21.8 GBq (589 mCi). No grade 4 or 5 renal toxicity was observed in our cohort.
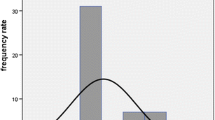
The mean long-term change of the body surface-corrected GFR was −2.1 ± 13.1 ml/min/m2 per year (median −1.0 ml/min/m2 per year), corresponding to a relative yearly GFR reduction of −1.8 ± 18.9 %. Following PRRT, 15 patients (21 %) experienced a mild (2–10 ml/min/m2 per year) and 16 patients (22 %) a moderate to significant (>10 ml/min/m2 per year) decline in GFR. However, 11 patients (15 %) showed an increase of >10 ml/min/m2 per year.
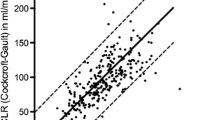
Of the entire cohort, 54 patients (73 %) and 13 of the 16 patients (81 %) with significant yearly loss of GFR had at least one risk factor for development of radiation-induced kidney disease (Table 1). However, statistical analysis revealed no significant relationship between the decline of GFR and the baseline characteristics (i.e. age ≥70 years, GFR <60 ml/min/1.73 m2, DM, HTN, previous chemotherapy) of the patients (Fig. 1). Also, none of these factors were associated with a GFR reduction of >10 ml/min/m2 per year, applying logistic regression analysis (p > 0.1 for all included variables). Interestingly, even the administration of higher cumulative activities of 177Lu-octreotate was not associated with more pronounced reductions of GFR (Fig. 2, p = 0.1). To determine how balanced other risk factors were over the total activities given, Table 2 lists respective patient characteristics according to the cumulative administered activities (<29.6 GBq vs >29.6 GBq).
Nephrotoxicity (CTCAE) graded according to serum creatinine was different from that based on accurate determination by GFR in 49 of 326 assessments (15 %). Overall, it resulted in underestimation of the maximum observed renal toxicity grade by serum creatinine in nine patients (12 %).
Discussion
This retrospective study on 74 patients provides the first accurate long-term follow-up assessment of renal function after PRRT with 177Lu-octreotate and demonstrates the renal safety of this treatment even after high cumulative activities. However, minor renal impairment (GFR loss >2 ml/min/m2 per year) could be detected in 43 % of patients. This prevalent slight reduction of GFR over time was captured by the accurate assessment applying serial 99mTc-DTPA clearance measurements revealing the general underestimation of kidney function loss by classical serum creatinine-based approaches.
To the best of our knowledge, this is the first study assessing the influence of cumulative activity on long-term renal function. Although previous studies have described the degree of kidney toxicity in patient cohorts receiving <27.0–29.6 GBq 177Lu-octreotate [30, 31], there are no data available on renal toxicity after higher cumulative activities or on potential activity-toxicity relations. The results of our study show that there is no significant correlation but only a trend towards more pronounced reductions of GFR over time (Fig. 2) after higher activities. In those patients receiving >29.6 GBq of 177Lu-octreotate (n = 37, 50 % of all patients), no significant increase of renal toxicity or yearly reduction of GFR was observed (Table 1, Fig. 1). This unexpected observation was probably not due to patient selection alone as the presence of potential risk factors was relatively well balanced between the two total-dose subgroups (Table 2). This may provide an argument against dose reduction protocols intended to avoid renal toxicity in 177Lu-based PRRT.
While for 90Y-based PRRT there is some evidence of the influence of potential risk factors such as arterial HTN, DM and age on developing renal toxicity [25, 32], no comparable data are available for 177Lu-based regimens, probably due to the long follow-up GFR assessments needed to trace these slighter reductions of renal function. By implementing the state-of-the-art blood clearance-based assessment of GFR, we were able to provide a first risk factor analysis for time-related renal function loss after 177Lu-based PRRT. In agreement with previous studies the majority of our patients with significant yearly loss of GFR (81 %) had at least one risk factor for development of radiation-induced kidney disease [30]. Interestingly, however, none of the previously suggested and commonly considered risk factors for PRRT-induced nephrotoxicity including age >70 years, DM and HTN were associated with a significant time-dependent GFR reduction (Table 1, Fig. 1); history of previous systemic chemotherapy and a baseline GFR of less than 60 ml/min/1.73 m2 were also not predictive of significant renal toxicity. However, these findings are not in contradiction to any reported data on 177Lu-based PRRT as the above-mentioned risk factors are derived from 90Y-associated renal events [2, 30, 33]. Our findings support the widely practised approach of including patients with renal risk factors for 177Lu-based PRRT. Accordingly, there is no current recommendation regarding dose reduction or withholding treatment in such patients for 177Lu-based PRRT [1]. Our institutional cut-off GFR for patient inclusion is as low as ≥30 ml/min/1.73 m2 and none of the mentioned potential risk factors serves as a relative contraindication for PRRT with 177Lu-octreotate.
Reported overall renal toxicities (grade 3–4), observed with 90Y-labelled somatostatin analogues vary between 1.6 and 9.2 % [6, 7, 13, 25, 32] and a recent paper on 1,109 patients states an incidence of 9.2 % for this significant renal impairment [34]. For 177Lu-labelled somatostatin analogues these rates are less than 3 % [23, 32, 33, 35], and accordingly in our study only one patient (1.4 %) had significant renal impairment after PRRT, which was a CTCAE grade 3 event. No grade 4 renal toxicities were observed. This confirms the renal safety of 177Lu-based PRRT.
In the study by Gupta et al. [31] a significant decrease of baseline GFR from 86.8 ± 15.4 to 66.1 ± 14.5 ml/min/1.73 m2 was observed 6 weeks after PRRT with 177Lu-octreotate. This very short follow-up period of the study, however, hampers a reliable estimation of radiation-induced nephrotoxicity. Extrapolation of long-term renal function loss from these data would lead to high rates of anticipated renal insufficiency which contradicts cumulative experience, especially the largest reported series from the Rotterdam group (2 cases of renal insufficiency in 504 patients) [2]. Also, the deduction of renal function alterations from only two GFR measurements per patient (pretreatment and 6 weeks post-treatment) further weakens the accuracy of the quantified renal function loss. In our study, repeated time-point measurements modelled by a linear curve fit may add accuracy to the individual GFR course and will probably better reflect the true long-term reduction of glomerular function.
However, our study also suffers from inaccuracies regarding true long-term renal function loss. One major issue is the inherent limitation of GFR measurement by means of 99mTc-DTPA as it is an operator-dependent technique and also depends on height and weight of the patient. Second, GFR impairment is a late event in the development of kidney damage after PRRT, whereas the primary targets of the irradiation are the proximal tubule, which reabsorbs the radiopeptide, and the interstitium, which subsequently retains the radioactivity. Thus, measurement of renal function using tracers with tubular extraction, like orthoiodohippurate (OIH) or mercaptoacetyltriglycine (MAG3), may provide more information about radiation nephropathy in early stages. Furthermore, renal dosimetry data were, unfortunately, not available to be included in this clinical observational study. It would be definitely interesting to compare absorbed renal doses to observed loss of renal function, which might be the subject of further studies.
Conclusion
This study implementing a state-of-the-art monitoring method of long-term renal function surveillance supports renal safety of 177Lu-octreotate, although a slight reduction of GFR over time (> 2 ml/min/m2 per year) is frequently detected. The lack of a significant association between higher cumulative activities and loss of GFR or other assumed renal risk factors disputes the need for dose reduction or strict patient selection based on kidney function in 177Lu-based PRRT.
References
Kwekkeboom DJ, de Herder WW, van Eijck CH, Kam BL, van Essen M, Teunissen JJ, et al. Peptide receptor radionuclide therapy in patients with gastroenteropancreatic neuroendocrine tumors. Semin Nucl Med 2010;40(2):78–88. doi:10.1053/j.semnuclmed.2009.10.004.
Kwekkeboom DJ, de Herder WW, Kam BL, van Eijck CH, van Essen M, Kooij PP, et al. Treatment with the radiolabeled somatostatin analog [177 Lu-DOTA 0, Tyr3]octreotate: toxicity, efficacy, and survival. J Clin Oncol 2008;26(13):2124–30. doi:10.1200/JCO.2007.15.2553.
Kwekkeboom DJ, de Herder WW, Krenning EP. Somatostatin receptor-targeted radionuclide therapy in patients with gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin North Am 2011;40(1):173–85, ix. doi:10.1016/j.ecl.2010.12.003.
Buscombe JR, Caplin ME, Hilson AJ. Long-term efficacy of high-activity 111in-pentetreotide therapy in patients with disseminated neuroendocrine tumors. J Nucl Med 2003;44(1):1–6.
Delpassand ES, Samarghandi A, Mourtada JS, Zamanian S, Espenan GD, Sharif R, et al. Long-term survival, toxicity profile, and role of F-18 FDG PET/CT scan in patients with progressive neuroendocrine tumors following peptide receptor radionuclide therapy with high activity In-111 pentetreotide. Theranostics 2012;2(5):472–80. doi:10.7150/thno.3739.
Waldherr C, Pless M, Maecke HR, Haldemann A, Mueller-Brand J. The clinical value of [90Y-DOTA]-D-Phe1-Tyr3-octreotide (90Y-DOTATOC) in the treatment of neuroendocrine tumours: a clinical phase II study. Ann Oncol 2001;12(7):941–5.
Waldherr C, Pless M, Maecke HR, Schumacher T, Crazzolara A, Nitzsche EU, et al. Tumor response and clinical benefit in neuroendocrine tumors after 7.4 GBq (90)Y-DOTATOC. J Nucl Med 2002;43(5):610–6.
Ezziddin S, Sabet A, Heinemann F, Yong-Hing CJ, Ahmadzadehfar H, Guhlke S, et al. Response and long-term control of bone metastases after peptide receptor radionuclide therapy with (177)Lu-octreotate. J Nucl Med 2011;52(8):1197–203. doi:10.2967/jnumed.111.090373.
Ezziddin S, Opitz M, Attassi M, Biermann K, Sabet A, Guhlke S, et al. Impact of the Ki-67 proliferation index on response to peptide receptor radionuclide therapy. Eur J Nucl Med Mol Imaging 2011;38(3):459–66. doi:10.1007/s00259-010-1610-2.
Bernard BF, Krenning EP, Breeman WA, Rolleman EJ, Bakker WH, Visser TJ, et al. D-lysine reduction of indium-111 octreotide and yttrium-90 octreotide renal uptake. J Nucl Med 1997;38(12):1929–33.
de Jong M, Krenning E. New advances in peptide receptor radionuclide therapy. J Nucl Med 2002;43(5):617–20.
Paganelli G, Zoboli S, Cremonesi M, Bodei L, Ferrari M, Grana C, et al. Receptor-mediated radiotherapy with 90Y-DOTA-D-Phe1-Tyr3-octreotide. Eur J Nucl Med 2001;28(4):426–34.
Otte A, Herrmann R, Heppeler A, Behe M, Jermann E, Powell P, et al. Yttrium-90 DOTATOC: first clinical results. Eur J Nucl Med 1999;26(11):1439–47.
Cybulla M, Weiner SM, Otte A. End-stage renal disease after treatment with 90Y-DOTATOC. Eur J Nucl Med 2001;28(10):1552–4. doi:10.1007/s002590100599.
Cwikla JB, Sankowski A, Seklecka N, Buscombe JR, Nasierowska-Guttmejer A, Jeziorski KG, et al. Efficacy of radionuclide treatment DOTATATE Y-90 in patients with progressive metastatic gastroenteropancreatic neuroendocrine carcinomas (GEP-NETs): a phase II study. Ann Oncol 2010;21(4):787–94. doi:10.1093/annonc/mdp372.
Moll S, Nickeleit V, Mueller-Brand J, Brunner FP, Maecke HR, Mihatsch MJ. A new cause of renal thrombotic microangiopathy: yttrium 90-DOTATOC internal radiotherapy. Am J Kidney Dis 2001;37(4):847–51.
Stoffel MP, Pollok M, Fries J, Baldamus CA. Radiation nephropathy after radiotherapy in metastatic medullary thyroid carcinoma. Nephrol Dial Transplant 2001;16(5):1082–3.
Behr TM, Behe MP. Cholecystokinin-B/gastrin receptor-targeting peptides for staging and therapy of medullary thyroid cancer and other cholecystokinin-B receptor-expressing malignancies. Semin Nucl Med 2002;32(2):97–109. doi:10.1053/snuc.2002.31028.
Forrer F, Rolleman E, Bijster M, Melis M, Bernard B, Krenning EP, et al. From outside to inside? Dose-dependent renal tubular damage after high-dose peptide receptor radionuclide therapy in rats measured with in vivo (99m)Tc-DMSA-SPECT and molecular imaging. Cancer Biother Radiopharm 2007;22(1):40–9. doi:10.1089/cbr.2006.353.
Rolleman EJ, Krenning EP, Bernard BF, de Visser M, Bijster M, Visser TJ, et al. Long-term toxicity of [(177)Lu-DOTA (0), Tyr (3)]octreotate in rats. Eur J Nucl Med Mol Imaging 2007;34(2):219–27. doi:10.1007/s00259-006-0232-1.
Pöge U, Gerhardt T, Palmedo H, Klehr HU, Sauerbruch T, Woitas RP. MDRD equations for estimation of GFR in renal transplant recipients. Am J Transplant 2005;5(6):1306–11. doi:10.1111/j.1600-6143.2005.00861.x.
Kwekkeboom DJ, Bakker WH, Kooij PP, Konijnenberg MW, Srinivasan A, Erion JL, et al. [177Lu-DOTAOTyr3]octreotate: comparison with [111In-DTPAo]octreotide in patients. Eur J Nucl Med 2001;28(9):1319–25.
Forrer F, Uusijärvi H, Storch D, Maecke HR, Mueller-Brand J. Treatment with 177Lu-DOTATOC of patients with relapse of neuroendocrine tumors after treatment with 90Y-DOTATOC. J Nucl Med 2005;46(8):1310–6.
Kwekkeboom DJ, Bakker WH, Kam BL, Teunissen JJ, Kooij PP, de Herder WW, et al. Treatment of patients with gastro-entero-pancreatic (GEP) tumours with the novel radiolabelled somatostatin analogue [177Lu-DOTA(0), Tyr3]octreotate. Eur J Nucl Med Mol Imaging 2003;30(3):417–22. doi:10.1007/s00259-002-1050-8.
Bodei L, Cremonesi M, Ferrari M, Pacifici M, Grana CM, Bartolomei M, et al. Long-term evaluation of renal toxicity after peptide receptor radionuclide therapy with 90Y-DOTATOC and 177Lu-DOTATATE: the role of associated risk factors. Eur J Nucl Med Mol Imaging 2008;35(10):1847–56. doi:10.1007/s00259-008-0778-1.
Flynn AA, Pedley RB, Green AJ, Dearling JL, El-Emir E, Boxer GM, et al. The nonuniformity of antibody distribution in the kidney and its influence on dosimetry. Radiat Res 2003;159(2):182–9.
Breeman WA, De Jong M, Visser TJ, Erion JL, Krenning EP. Optimising conditions for radiolabelling of DOTA-peptides with 90Y, 111In and 177Lu at high specific activities. Eur J Nucl Med Mol Imaging 2003;30(6):917–20. doi:10.1007/s00259-003-1142-0.
Breeman WA, van der Wansem K, Bernard BF, van Gameren A, Erion JL, Visser TJ, et al. The addition of DTPA to [177Lu-DOTA0, Tyr3]octreotate prior to administration reduces rat skeleton uptake of radioactivity. Eur J Nucl Med Mol Imaging 2003;30(2):312–5. doi:10.1007/s00259-002-1054-4.
Russell CD, Bischoff PG, Kontzen FN, Rowell KL, Yester MV, Lloyd LK, et al. Measurement of glomerular filtration rate: single injection plasma clearance method without urine collection. J Nucl Med 1985;26(11):1243–7.
Bodei L, Cremonesi M, Grana CM, Fazio N, Iodice S, Baio SM, et al. Peptide receptor radionuclide therapy with (177)Lu-DOTATATE: the IEO phase I–II study. Eur J Nucl Med Mol Imaging 2011;38(12):2125–35. doi:10.1007/s00259-011-1902-1.
Gupta SK, Singla S, Bal C. Renal and hematological toxicity in patients of neuroendocrine tumors after peptide receptor radionuclide therapy with 177Lu-DOTATATE. Cancer Biother Radiopharm 2012;27(9):593–9. doi:10.1089/cbr.2012.1195.
Valkema R, Pauwels SA, Kvols LK, Kwekkeboom DJ, Jamar F, de Jong M, et al. Long-term follow-up of renal function after peptide receptor radiation therapy with (90)Y-DOTA(0), Tyr(3)-octreotide and (177)Lu-DOTA(0), Tyr(3)-octreotate. J Nucl Med 2005;46 Suppl 1:83S–91S.
Kwekkeboom DJ, Teunissen JJ, Bakker WH, Kooij PP, de Herder WW, Feelders RA, et al. Radiolabeled somatostatin analog [177Lu-DOTA0, Tyr3]octreotate in patients with endocrine gastroenteropancreatic tumors. J Clin Oncol 2005;23(12):2754–62. doi:10.1200/JCO.2005.08.066.
Imhof A, Brunner P, Marincek N, Briel M, Schindler C, Rasch H, et al. Response, survival, and long-term toxicity after therapy with the radiolabeled somatostatin analogue [90Y-DOTA]-TOC in metastasized neuroendocrine cancers. J Clin Oncol 2011;29(17):2416–23. doi:10.1200/JCO.2010.33.7873.
Frilling A, Weber F, Saner F, Bockisch A, Hofmann M, Mueller-Brand J, et al. Treatment with (90)Y- and (177)Lu-DOTATOC in patients with metastatic neuroendocrine tumors. Surgery 2006;140(6):968–76. doi:10.1016/j.surg.2006.07.030. discussion 76–77.
Acknowledgments
The authors are grateful to Professor Eric Krenning, Professor Dik Kwekkeboom and Professor Wouter A. P. Breeman (Erasmus Medical Center, Rotterdam, Netherlands) for sharing their experience in the receptor targeting field and making somatostatin receptor-mediated treatment in our institution possible. Also, we thank Professor Richard P. Baum (Department of Nuclear Medicine and PET Center, Zentralklinik Bad Berka, Germany) for his critical and constructive input in this field. The authors also are thankful to the personnel of the Nuclear Medicine Department and especially the nursing staff of the therapy ward.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sabet, A., Ezziddin, K., Pape, UF. et al. Accurate assessment of long-term nephrotoxicity after peptide receptor radionuclide therapy with 177Lu-octreotate. Eur J Nucl Med Mol Imaging 41, 505–510 (2014). https://doi.org/10.1007/s00259-013-2601-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-013-2601-x