Abstract
Purpose
Prostate-specific membrane antigen (PSMA) is a transmembrane protein overexpressed in prostate cancer and is therefore being explored as a biomarker for diagnosing and staging of the disease. Here we report preclinical data on BAY 1075553 (a 9:1 mixture of (2S,4S)- and (2R,4S)-2-[18F]fluoro-4-phosphonomethyl-pentanedioic acid), a novel 18F-labelled small molecule inhibitor of PSMA enzymatic activity, which can be efficiently synthesized from a direct radiolabelling precursor.
Methods
The 18F-radiolabelled stereoisomers of 2-[18F]fluoro-4-(phosphonomethyl)-pentanedioic acid were synthesized from their respective isomerically pure precursors dimethyl 2-{[bis(benzyloxy)phosphoryl]methyl}-4-(tosyloxy)pentanedioate. In vivo positron emission tomography (PET) imaging and biodistribution studies were conducted in mice bearing LNCaP, 22Rv1 and PC-3 tumours. Pharmacokinetic parameters and dosimetry estimates were calculated based on biodistribution studies in rodents. For non-clinical safety assessment (safety pharmacology, toxicology) to support a single-dose human microdose study, off-target effects in vitro, effects on vital organ functions (cardiovascular in dogs, nervous system in rats), mutagenicity screens and an extended single-dose study in rats were conducted with the non-radioactive racemic analogue of BAY 1075553.
Results
BAY 1075553 showed high tumour accumulation specific to PSMA-positive tumour-bearing mice and was superior to other stereoisomers tested. Fast clearance of BAY 1075553 resulted overall in low background signals in other organs except for high uptake into kidney and bladder which was mainly caused by renal elimination of BAY 1075553. A modest uptake into bone was observed which decreased over time indicating organ-specific uptake as opposed to defluorination of BAY 1075553 in vivo. Biodistribution studies found highest organ doses for kidneys and the urinary bladder wall resulting in a projected effective dose (ED) in humans of 0.0219 mSv/MBq. Non-clinical safety studies did not show off-target activity, effects on vital organs function or dose-dependent adverse effects.
Conclusion
BAY 1075553 was identified as a promising PET tracer for PSMA-positive prostate tumours in preclinical studies. BAY 1075553 can be produced using a robust, direct radiosynthesis procedure. Pharmacokinetic, toxicology and safety pharmacology studies support the application of BAY 1075553 in a first-in-man microdose study with single i.v. administration.







Similar content being viewed by others
References
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300.
Rinnab L, Simon J, Hautmann RE, Cronauer MV, Hohl K, Buck AK, et al. [(11)C]choline PET/CT in prostate cancer patients with biochemical recurrence after radical prostatectomy. World J Urol. 2009;27:619–25.
Beheshti M, Vali R, Waldenberger P, Fitz F, Nader M, Loidl W, et al. Detection of bone metastases in patients with prostate cancer by 18F fluorocholine and 18F fluoride PET-CT: a comparative study. Eur J Nucl Med Mol Imaging. 2008;35:1766–74.
Kotzerke J, Volkmer BG, Glatting G, van den Hoff J, Gschwend JE, Messer P, et al. Intraindividual comparison of [11C]acetate and [11C]choline PET for detection of metastases of prostate cancer. Nuklearmedizin. 2003;42:25–30.
Castellucci P, Fuccio C, Nanni C, Santi I, Rizzello A, Lodi F, et al. Influence of trigger PSA and PSA kinetics on 11C-choline PET/CT detection rate in patients with biochemical relapse after radical prostatectomy. J Nucl Med. 2009;50:1394–400.
Iason. IASOcholine 1,0 GBq/ml, Injektionslösung, Fachinformation Deutschland. [http://www.iason.eu/fileadmin/user_upload/SPC/iasocholine%20germany.pdf].
Gambhir SS, Czernin J, Schwimmer J, Silverman DH, Coleman RE, Phelps ME. A tabulated summary of the FDG PET literature. J Nucl Med. 2001;42:1S–93.
Oyama N, Akino H, Suzuki Y, Kanamaru H, Sadato N, Yonekura Y, et al. The increased accumulation of [18F]fluorodeoxyglucose in untreated prostate cancer. Jpn J Clin Oncol. 1999;29:623–9.
Schwarzenbock S, Souvatzoglou M, Krause BJ. Choline PET and PET/CT in primary diagnosis and staging of prostate cancer. Theranostics. 2012;2:318–30.
Sutinen E, Nurmi M, Roivainen A, Varpula M, Tolvanen T, Lehikoinen P, et al. Kinetics of [(11)C]choline uptake in prostate cancer: a PET study. Eur J Nucl Med Mol Imaging. 2004;31:317–24.
Li Y, Cozzi PJ, Russell PJ. Promising tumor-associated antigens for future prostate cancer therapy. Med Res Rev. 2010;30:67–101.
Horoszewicz JS, Kawinski E, Murphy GP. Monoclonal antibodies to a new antigenic marker in epithelial prostatic cells and serum of prostatic cancer patients. Anticancer Res. 1987;7:927–35.
Wright Jr GL, Haley C, Beckett ML, Schellhammer PF. Expression of prostate-specific membrane antigen in normal, benign, and malignant prostate tissues. Urol Oncol. 1995;1:18–28.
Silver DA, Pellicer I, Fair WR, Heston WD, Cordon-Cardo C. Prostate-specific membrane antigen expression in normal and malignant human tissues. Clin Cancer Res. 1997;3:81–5.
Sweat SD, Pacelli A, Murphy GP, Bostwick DG. Prostate-specific membrane antigen expression is greatest in prostate adenocarcinoma and lymph node metastases. Urology. 1998;52:637–40.
Bostwick DG, Pacelli A, Blute M, Roche P, Murphy GP. Prostate specific membrane antigen expression in prostatic intraepithelial neoplasia and adenocarcinoma: a study of 184 cases. Cancer. 1998;82:2256–61.
Wright Jr GL, Grob BM, Haley C, Grossman K, Newhall K, Petrylak D, et al. Upregulation of prostate-specific membrane antigen after androgen-deprivation therapy. Urology. 1996;48:326–34.
Chang SS, Gaudin PB, Reuter VE, Heston WD. Prostate-specific membrane antigen: present and future applications. Urology. 2000;55:622–9.
Ananias HJ, van den Heuvel MC, Helfrich W, de Jong IJ. Expression of the gastrin-releasing peptide receptor, the prostate stem cell antigen and the prostate-specific membrane antigen in lymph node and bone metastases of prostate cancer. Prostate. 2009;69:1101–8.
Mannweiler S, Amersdorfer P, Trajanoski S, Terrett JA, King D, Mehes G. Heterogeneity of prostate-specific membrane antigen (PSMA) expression in prostate carcinoma with distant metastasis. Pathol Oncol Res. 2009;15:167–72.
Mhawech-Fauceglia P, Zhang S, Terracciano L, Sauter G, Chadhuri A, Herrmann FR, et al. Prostate-specific membrane antigen (PSMA) protein expression in normal and neoplastic tissues and its sensitivity and specificity in prostate adenocarcinoma: an immunohistochemical study using mutiple tumour tissue microarray technique. Histopathology. 2007;50:472–83.
Mease RC. Radionuclide based imaging of prostate cancer. Curr Top Med Chem. 2010;10:1600–16.
Tagawa ST, Milowsky MI, Morris MJ, Vallabhajosula S, Christos PJ, Akhtar NH, et al. Phase II study of lutetium-177 labeled anti-prostate-specific membrane antigen (PSMA) monoclonal antibody J591 for metastatic castration-resistant prostate cancer. Clin Cancer Res. 2013.
Holland JP, Divilov V, Bander NH, Smith-Jones PM, Larson SM, Lewis JS. 89Zr-DFO-J591 for immunoPET of prostate-specific membrane antigen expression in vivo. J Nucl Med. 2010;51:1293–300.
Robinson MB, Blakely RD, Couto R, Coyle JT. Hydrolysis of the brain dipeptide N-acetyl-L-aspartyl-L-glutamate. Identification and characterization of a novel N-acetylated alpha-linked acidic dipeptidase activity from rat brain. J Biol Chem. 1987;262:14498–506.
Slusher BS, Vornov JJ, Thomas AG, Hurn PD, Harukuni I, Bhardwaj A, et al. Selective inhibition of NAALADase, which converts NAAG to glutamate, reduces ischemic brain injury. Nat Med. 1999;5:1396–402.
Banerjee SR, Pullambhatla M, Byun Y, Nimmagadda S, Green G, Fox JJ, et al. 68Ga-labeled inhibitors of prostate-specific membrane antigen (PSMA) for imaging prostate cancer. J Med Chem. 2010;53:5333–41.
Chen Y, Foss CA, Byun Y, Nimmagadda S, Pullambhatla M, Fox JJ, et al. Radiohalogenated prostate-specific membrane antigen (PSMA)-based ureas as imaging agents for prostate cancer. J Med Chem. 2008;51:7933–43.
Lapi SE, Wahnishe H, Pham D, Wu LY, Nedrow-Byers JR, Liu T, et al. Assessment of an 18F-labeled phosphoramidate peptidomimetic as a new prostate-specific membrane antigen-targeted imaging agent for prostate cancer. J Nucl Med. 2009;50:2042–8.
Maresca KP, Hillier SM, Femia FJ, Keith D, Barone C, Joyal JL, et al. A series of halogenated heterodimeric inhibitors of prostate specific membrane antigen (PSMA) as radiolabeled probes for targeting prostate cancer. J Med Chem. 2009;52:347–57.
Mease RC, Dusich CL, Foss CA, Ravert HT, Dannals RF, Seidel J, et al. N-[N-[(S)-1,3-Dicarboxypropyl]carbamoyl]-4-[18F]fluorobenzyl-L-cysteine, [18F]DCFBC: a new imaging probe for prostate cancer. Clin Cancer Res. 2008;14:3036–43.
Barrett JA, Coleman RE, Goldsmith SJ, Vallabhajosula S, Petry NA, Cho S, et al. First-in-man evaluation of 2 high-affinity PSMA-avid small molecules for imaging prostate cancer. J Nucl Med. 2013;54:380–7.
Cho SY, Gage KL, Mease RC, Senthamizhchelvan S, Holt DP, Jeffrey-Kwanisai A, et al. Biodistribution, tumor detection, and radiation dosimetry of 18F-DCFBC, a low-molecular-weight inhibitor of prostate-specific membrane antigen, in patients with metastatic prostate cancer. J Nucl Med. 2012;53:1883–91.
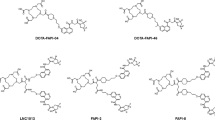
Graham K, Lesche R, Gromov AV, Böhnke N, Schäfer M, Hassfeld J, et al. Radiofluorinated derivatives of 2-(phosphonomethyl)pentanedioic acid as inhibitors of prostate specific membrane antigen (PSMA) for the imaging of prostate cancer. J Med Chem. 2012;55:9510–20.
Graham K, Lesche R, Gromov AV, Böhnke N, Hassfeld J, Kettschau G. Prostate specific membrane antigen inhibitors. Patent WO 2011/073286, 2011.
Graham K, Ede S. Derivatization of radiopharmaceuticals. Patent WO2012/104225, 2012.
Graham K, Kettschau G, Gromov A, Dinkelborg L. Development of a fast robust derivatization method of an extremely polar PET radiopharmaceutical; a critical aspect for starting a clinical trial. Tetrahedron Lett. 2013;54:2583–6.
Stabin MG, Siegel JA. Physical models and dose factors for use in internal dose assessment. Health Phys. 2003;85:294–310.
Stabin MG, da Luz LC. Decay data for internal and external dose assessment. Health Phys. 2002;83:471–5.
Himmel HM. Suitability of commonly used excipients for electrophysiological in-vitro safety pharmacology assessment of effects on hERG potassium current and on rabbit Purkinje fiber action potential. J Pharmacol Toxicol Methods. 2007;56:145–58.
Hamon J, Whitebread S, Techer-Etienne V, Le Coq H, Azzaoui K, Urban L. In vitro safety pharmacology profiling: what else beyond hERG? Future Med Chem. 2009;1:645–65.
Himmel HM, Hoffmann M. QTc shortening with a new investigational cancer drug: a brief case study. J Pharmacol Toxicol Methods. 2010;62:72–81.
Tsai G, Slusher BS, Sim L, Coyle JT. Immunocytochemical distribution of N-acetylaspartylglutamate in the rat forebrain and glutamatergic pathways. J Chem Neuroanat. 1993;6:277–92.
Hillier SM, Kern AM, Maresca KP, Marquis JC, Eckelman WC, Joyal JL, et al. 123I-MIP-1072, a small-molecule inhibitor of prostate-specific membrane antigen, is effective at monitoring tumor response to taxane therapy. J Nucl Med. 2011;52:1087–93.
Ghosh A, Wang X, Klein E, Heston WD. Novel role of prostate-specific membrane antigen in suppressing prostate cancer invasiveness. Cancer Res. 2005;65:727–31.
Radiation dose to patients from radiopharmaceuticals (addendum 2 to ICRP publication 53). Ann ICRP. 1998;28:1–126.
Foss CA, Mease RC, Fan H, Wang Y, Ravert HT, Dannals RF, et al. Radiolabeled small-molecule ligands for prostate-specific membrane antigen: in vivo imaging in experimental models of prostate cancer. Clin Cancer Res. 2005;11:4022–8.
Misra P, Humblet V, Pannier N, Maison W, Frangioni JV. Production of multimeric prostate-specific membrane antigen small-molecule radiotracers using a solid-phase 99mTc preloading strategy. J Nucl Med. 2007;48:1379–89.
Banerjee SR, Foss CA, Castanares M, Mease RC, Byun Y, Fox JJ, et al. Synthesis and evaluation of technetium-99m- and rhenium-labeled inhibitors of the prostate-specific membrane antigen (PSMA). J Med Chem. 2008;51:4504–17.
Hamacher K. Synthesis of N.C.A. cis- and trans-4-[18F]fluoro-l-proline, radiotracers for PET-investigation of disordered matrix protein synthesis. J Labelled Comp Radiopharm. 1999;42:1135–44.
Krasikova RN, Kuznetsova OF, Fedorova OS, Belokon YN, Maleev VI, Mu L, et al. 4-[18F]fluoroglutamic acid (BAY 85–8050), a new amino acid radiotracer for PET imaging of tumors: synthesis and in vitro characterization. J Med Chem. 2011;54:406–10.
Zengerling F, Schrader AJ, Schrader M, Jentzmik F. Diagnostic relevance of choline-PET/CT in patients with prostate cancer. Aktuelle Urol. 2012;43:49–54.
EMEA. Guidance on non-clinical safety studies for the conduct of human clinical trials and marketing authorization for pharmaceuticals, CPMP/ICH/286/95. 2009.
Langsteger W, Kunit T, Haim S, Nader M, Valencia R, Lesche R, et al. BAY 1075553 PET/CT in the assessment of prostate cancer: safety, tolerability and biodistribution—phase I first in human study results. J Nucl Med. 2012;53(Suppl 1):1125.
Beheshti M, Langsteger W, Sommerhuber A, Steinmair M, Wolf I, Valencia R, et al. BAY 1075553 PET/CT in staging and re-staging of prostate cancer patients—phase I study and comparison to 18F-FCH. J Nucl Med. 2012;53(Suppl 1):272.
Acknowledgments
We would like to acknowledge the excellent technical support of Selahattin Ede, Marion Zerna, Mario Mandau, Oliver Schenk, Uwe Rettig, Yvonne Duchstein, Eva-Maria Bickel, Jörg Jannsen, Herbert Himmel, and Michael Hoffmann. This work was conducted at and financially supported by Bayer Healthcare.
Conflicts of interest
All authors are or were employees of Bayer Healthcare.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Figure 1
(DOC 120 kb)
Supplementary Figure 2
(DOC 91 kb)
Supplementary Figure 3
(DOC 104 kb)
Supplementary Table 1
(DOC 44 kb)
Supplementary Table 2
(DOC 90 kb)
Supplementary Table 3
(DOC 31 kb)
Supplementary Table 4
(DOC 29 kb)
Rights and permissions
About this article
Cite this article
Lesche, R., Kettschau, G., Gromov, A.V. et al. Preclinical evaluation of BAY 1075553, a novel 18F-labelled inhibitor of prostate-specific membrane antigen for PET imaging of prostate cancer. Eur J Nucl Med Mol Imaging 41, 89–101 (2014). https://doi.org/10.1007/s00259-013-2527-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-013-2527-3