Abstract
6-Fluoro-(18F)-L-3,4-dihydroxyphenylalanine (FDOPA) is an amino acid analogue for positron emission tomography (PET) imaging which has been registered since 2006 in several European Union (EU) countries and by several pharmaceutical firms. Neuroendocrine tumour (NET) imaging is part of its registered indications. NET functional imaging is a very competitive niche, competitors of FDOPA being two well-established radiopharmaceuticals for scintigraphy, 123I-metaiodobenzylguanidine (MIBG) and 111In-pentetreotide, and even more radiopharmaceuticals for PET, including fluorodeoxyglucose (FDG) and somatostatin analogues. Nevertheless, there is no universal single photon emission computed tomography (SPECT) or PET tracer for NET imaging, at least for the moment. FDOPA, as the other PET tracers, is superior in diagnostic performance in a limited number of precise NET types which are currently medullary thyroid cancer, catecholamine-producing tumours with a low aggressiveness and well-differentiated carcinoid tumours of the midgut, and in cases of congenital hyperinsulinism. This article reports on diagnostic performance and impact on management of FDOPA according to the NET type, emphasising the results of comparative studies with other radiopharmaceuticals. By pooling the results of the published studies with a defined standard of truth, patient-based sensitivity to detect recurrent medullary thyroid cancer was 70 % [95 % confidence interval (CI) 62.1–77.6] for FDOPA vs 44 % (95 % CI 35–53.4) for FDG; patient-based sensitivity to detect phaeochromocytoma/paraganglioma was 94 % (95 % CI 91.4–97.1) for FDOPA vs 69 % (95 % CI 60.2–77.1) for 123I-MIBG; and patient-based sensitivity to detect midgut NET was 89 % (95 % CI 80.3–95.3) for FDOPA vs 80 % (95 % CI 69.2–88.4) for somatostatin receptor scintigraphy with a larger gap in lesion-based sensitivity (97 vs 49 %). Previously unpublished FDOPA results from our team are reported in some rare NET, such as small cell prostate cancer, or in emerging indications, such as metastatic NET of unknown primary (CUP-NET) or adrenocorticotropic hormone (ACTH) ectopic production. An evidence-based strategy in NET functional imaging is as yet affected by a low number of comparative studies. Then the suggested diagnostic trees, being a consequence of the analysis of present data, could be modified, for some indications, by a wider experience mainly involving face-to-face studies comparing FDOPA and 68Ga-labelled peptides.
Similar content being viewed by others
Neuroendocrine tumours (NET) are derived from endocrine cells; they usually contain secretory granules and have the capacity to produce biogenic amines and polypeptide hormones. These tumours often pose a difficult diagnostic challenge because of their small size and multiplicity. Nevertheless, an accurate staging of NET is important for the determination of resectability and of the prognosis. In 156 NET patients with the gastroenteropancreatic (GEP) type, the 5-year survival rate was lower (50 %) in 20 patients with extrahepatic secondary lesions than in 61 patients with only hepatic metastases (73 %) or 18 patients with nodal involvement (77 %) or in those with only local disease (96 %) [1]. The presence of extrahepatic sites of disease, bone metastases in particular, has been suggested to be a marker of a subgroup of patients with a worse prognosis and shorter survival [2] who would benefit more from aggressive therapeutic approaches.
Somatostatin receptor scintigraphy (SRS) with single photon emission computed tomography (SPECT), using 111In-pentetreotide or another somatostatin analogue labelled with 99mTc, detects the presence of somatostatin receptors, mainly the subtype 2. SRS is still currently the reference nuclear medicine investigation in NET. Being a whole-body examination, it is convenient for staging, with drawbacks linked to its biodistribution: a high activity in the liver, the spleen and delayed gut activity due to biliary excretion. SRS also has a clear limitation due to its poor spatial resolution to characterise suspicious lesions smaller than 10 mm on anatomic imaging modalities or to discover unsuspected small-sized lesions. Another cause of false-negative results is a lack of somatostatin receptor subtype 2 on the tumour tissue. In contrast, it has the advantage, when positive, to predict response to somatostatin analogue treatment [3].
An alternative to SRS is metaiodobenzylguanidine (MIBG) scintigraphy and SPECT, which is almost exclusively used in NET for imaging phaeochromocytomas, chemodectomas and rarely some NET of the ileum or medullary thyroid cancer (MTC). 123I or 131I have been both used for MIBG scintigraphy, but 123I-MIBG yields images with better resolution and a better signal for SPECT(/CT) and is currently the most widely reported for diagnostic application.
To take advantage of the superior resolution and the accurate uptake quantification offered by positron emission tomography (PET), several tracers have been proposed for a more effective functional imaging of NET. Currently, the only one that obtained a marketing authorisation (MA) in the European Union (EU) explicitly mentioning NET is 6-fluoro-(18F)-L-3,4-dihydroxyphenylalanine (FDOPA). Other “specific” NET tracers such as 6-fluoro-(18)-fluorodopamine (FDA) or the serotonin precursor 5-hydroxytryptophan (5-HTP) labelled with 11C have been proposed as well as several somatostatin analogues labelled with positron-emitting radionuclides, 68Ga in most cases (SRPET or SRPET/CT on hybrid PET/CT machines).
Importantly, poorly differentiated neuroendocrine cancers with little or no hormone production and a high proliferative activity usually take up 18F-fluorodeoxyglucose (FDG) as do most “common” cancers [4, 5], while sensitivity of NET tracers is poor.
FDOPA vs other radiopharmaceuticals
FDOPA has been used for PET imaging in humans for more than two decades, initially for studying the physiology and physiopathology of dihydroxyphenylalanine (DOPA) biodistribution in the human brain, in particular Parkinson’s syndrome, and then in oncology for NET or brain tumours. The pathophysiological rationale for PET imaging of NET with FDOPA is that several types of NET tumours are able to take up, decarboxylate and store amino acids, such as DOPA, and their biogenic amines [6, 7]. MA was granted for a commercial preparation of FDOPA in France in 2006, and others since then; and this radiopharmaceutical is commercially available.
Of the radiopharmaceuticals which are authorised by the French medicines agency for use in this context in our department, the least expensive is 18F-FDG, followed by 123I-MIBG, then 68Ga-edotreotide (68Ga-DOTATOC) and 111In-pentetreotide, 18F-FDOPA being the most expensive. This is due to a complicated process of 18F-FDOPA labelling which requires 18F2 gas instead of 18F-fluoride ion and has a low yield. However, the cost of the whole imaging examination integrates many other factors such as the time spent by the radiopharmacist and the technologist for the on-site preparation of the injection, the longest for DOTATOC, and the duration of the image acquisition, far longer with SPECT than with PET, impacting on the cost of the personnel and the workflow of the machine. The cost of the multiple transportations of the patient for the multiple scans which are recommended with MIBG or SRS should be taken into account. All those factors clearly reduce the gap in cost between FDOPA PET/CT, a rapid procedure, and SPECT/CT.
Furthermore, in the benefit-cost ratio, the benefit is not equal for all those radiopharmaceuticals. As will be further discussed in this article, the diagnostic performance of all those radiopharmaceuticals differs according to the type of the NET. A patient-based analysis of diagnostic performance is important, in particular for the detection of residual tumour after a radical treatment, but a lesion- or site-based analysis is also important as evaluating the real extension of the disease is a key element for tumour resectability and surgical procedure with curative intent. The benefit, evaluated by the impact on patient management, also depends on the potential use of internal radiotherapy revealed by the imaging modality. MIBG uptake by NET tumours may pave the way to 131I-MIBG internal radiotherapy which had been granted MA for several years to target NETs as well as neuroblastoma, and similarly a positive somatostatin analogue imaging opens the option of internal radiotherapy with 90Y- or 177Lu-labelled ligands of somatostatin receptors [8]. There is no such direct link with FDOPA or FDG imaging. But actually a radiopharmaceutical with a different functional approach is an advantage for indicating and monitoring internal radiotherapy: by comparing images of FDOPA PET/CT and MIBG SPECT or SRPET, tumours only taking up FDOPA can be delineated which are less likely to respond to the planned radiotherapy or have resisted to a past attempt, while the receptor-bearing tumours could have responded, leading to false-negative results when monitoring with the corresponding radiopharmaceutical.
FDOPA PET and PET/CT
The practice for FDOPA PET imaging in NET is not fully standardised at the moment. A 4-h fast is recommended by all teams, but sugar intake may be authorised in particular in hypoglycaemic patients. The oral premedication with the decarboxylase inhibitor carbidopa, which was introduced to block the aromatic amino acid decarboxylase enzyme, is less common than for brain FDOPA imaging. Eriksson et al. [9] reported that this administration led to a sixfold decrease in renal excretion while the tumour uptake increased threefold. Concordantly, Timmers et al. [10] reported that, compared with baseline FDOPA PET, carbidopa pretreatment resulted in the detection of 3 additional lesions in 3 of 11 patients with phaeochromocytoma or extra-adrenal paraganglioma. In contrast, in one infant in the series of Ribeiro et al. [11] the diffuse uptake of FDOPA in the pancreas completely disappeared under carbidopa treatment, while the kidney activity was still present: the patient had histologically proven diffuse abnormal pancreatic cells scattered in the whole pancreas. Similar findings were reported by Kauhanen et al. in 2008 in two of three adults with insulinoma. These findings do not favour the use of carbidopa in patients with pancreatic tumours since pancreatic physiological uptake disappears, and tumour uptake could not also disappear along with this [12].
The range of injected activity is 2–4 MBq/kg of body mass according to the MA, typically 150–400 MBq, reflecting the rapid evolution of PET machines, from 2-D acquisition to 3-D and then time-of-flight acquisition, allowing a reduction in injected activity. According to International Commission on Radiological Protection (ICRP) 106 (2008 vol. 38), the effective dose after IV injection of 18-FDOPA is 0.025 mSv/MBq in adults and 0.10 mSv/MBq in a 1-year-old child.
The FDOPA uptake by most organs and target lesions has been described as a plateau between 30 and 90 min post-injection [10]; there was no advantage of the 90-min scan over the 30-min scan, visually or with determination of standardized uptake value (SUV), in a series of 23 patients with various NET [13]. Thus, the starting time of whole-body image acquisition usually ranges between 45 and 65 min post-injection. However, early image acquisition 15–20 min after injection is useful in some indications, in particular MTC [14] or phaeochromocytoma [15].
In cases of metastatic NET, FDOPA is taken up not only by the soft tissue lesions but also by the bone metastases. In a series of 23 patients with advanced stage NET, FDOPA accurately detected skeletal lesions (sensitivity of 100 % and specificity of 91 %), even in 40 % of patients with a negative CT scan [13].
FDOPA PET is now performed on hybrid machines which provide PET/CT fusion and increase diagnostic performance. In a study comparing FDOPA PET/CT, PET or CT alone in MTC [16], PET identified all 18 lesions as positive, but was unable to definitively localise 4 lesions (22 %); CT could localise all 18 lesions, but could not definitively diagnose or exclude MTC in 6 lesions (33 %); only FDOPA PET/CT accurately characterised and localised all 18 lesions. Similar results demonstrating the superiority of FDOPA PET/CT over FDOPA PET and CT alone have been reported in phaeochromocytoma [17], midgut carcinoid tumours or pancreatic islet cell tumours [18].
False-positive results in inflammatory lesions that are frequent with FDG PET seem to be very rare with FDOPA PET. There is in fact one single report in oncology published as an abstract [19]: on FDOPA PET performed during treatment evaluation of a small cell neuroendocrine laryngeal carcinoma, a mediastinal hot spot corresponded to sarcoidosis. Nevertheless, the possibility of an inflammatory lesion should be kept in mind when an unexpected FDOPA focus is detected. The physiological diffuse uptake in the pancreas, and in the gallbladder leading to gut activity, may cause some problems in the interpretation.
As our team previously demonstrated by comparing the uptake of several tracers, NET does not constitute a biologically and metabolically homogeneous group of tumours [20, 21]. We will thus report on the utility of FDOPA by distinguishing the major types of NET and emphasising recent comparative studies with other radiopharmaceuticals. An evidence-based strategy in NET functional imaging is as yet affected by a low number of comparative studies. Then the suggested diagnostic trees, being a consequence of the analysis of present data, could be modified, for some indications, by a wider experience mainly involving face-to-face studies comparing FDOPA and 68-labelled peptides.
Medullary thyroid cancer
The initial study by Hoegerle et al. [22] compared, in 11 MTC patients, FDOPA PET with the established functional and morphological imaging methods, including FDG PET. A recent meta-analysis of eight studies on suspected recurrent MTC found the patient-based detection rate for FDOPA PET(/CT) to be 66 and 71 % for lesion-based analysis, which is an operational result in cases of occult recurrent disease [23]. All published studies have confirmed the superiority of FDOPA over all other radiopharmaceuticals [16, 22, 24–32] (Table 1), in particular in the detection of metastatic lymph nodes [22, 32] (Fig. 1). When compared to morphological imaging, FDOPA has a clear advantage for specificity [22, 29]. Pooling the results of three studies [26, 32, 33], the impact of FDOPA PET(/CT) estimated by the rate of changes in patient management is 20/59 =34 %. The performance of FDOPA varies according to the serum levels of the two biochemical markers, calcitonin (CTN) and carcinoembryonic antigen (CEA).
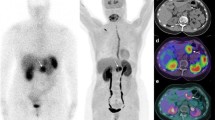
MTC treated by total thyroidectomy and lymph node dissection. a–b The patient presented with an occult biochemical recurrence 1.5 years later [serum calcitonin (CTN)=1,130 ng/l, carcinoembryonic antigen (CEA) =46 μg/l] and was referred to FDOPA PET/CT. On the early images after injection (a), a clear focus was visible, corresponding on CT to a left lymph node in the left upper mediastinum, with smaller and less intense contralateral foci. But the foci were no longer visible 1 h later on the whole-body acquisition (b) and the examination was considered as doubtful. c–e Another 1.5 years later, the markers were still rising (CTN=2,400 ng/ml, CEA =59 μg/l) and the patient was referred for FDG and FDOPA PET/CT prior to surgical exploration. On FDG PET/CT, 1 h after injection, a faint uptake (SUVmax =1.8) was visible by the left mediastinal lymph node (the most intense FDOPA uptake 1.5 years before) (c) but no other lesion (d). On FDOPA PET/CT (e), the left mediastinal focus took up FDOPA (SUVmax =2.9) together with several other foci: one left supraclavicular focus and one upper thoracic focus on the left side and two foci in the right upper mediastinum. Their intensity decreased after 1 h. The dissection and histological examination of the left supraclavicular region found two metastatic lymph nodes, 8 and 5 mm in size. CTN levels dropped to 1,600 ng/l. f Nineteen months later, another FDOPA PET was performed for restaging prior to surgery. With the exception of the left supraclavicular focus which had been resected, all other foci were viable, and their uptake at 1 h was now as intense as on the early images. This observation illustrates the importance of early image acquisition after FDOPA injection for early detection of metastatic MTC and the better performance of FDOPA as compared to FDG in a slow-growing form of MTC
In the comparative study by Koopmans et al. [27], FDOPA was the most sensitive imaging modality, but of eight patients with CTN <500 ng/l FDOPA was positive in only one (CTN=86 ng/l, CEA=1.1 μg/l) and FDG in another one (CTN =73 ng/l, CEA =1.2 μg/l). In the study of Luster et al. [16], no true-positive FDOPA PET/CT case was found in patients with basal CTN <60 ng/l, and conversely, no true-negative PET/CT case was found in patients with basal CTN >120 ng/l. FDOPA PET/CT had 100 % sensitivity and specificity when CTN at the time of scanning was >150 ng/l.
FDG may detect lesions missed by FDOPA. In the series of Marzola et al., FDOPA was positive alone in 5/18 patients, but FDG was positive alone in 1 patient and showed more lesions in 2 others [28]. In the series of Kauhanen et al., for a CEA doubling time of less than 24 months, FDG PET/CT correctly detected metastases in 80 % of patients and FDOPA PET/CT in 60 % [29]. An efficacy of FDG in cases of short doubling time of serum CTN and CEA levels has been confirmed by Verbeek et al. [30], FDG PET positivity being an indicator for poor survival, while FDOPA PET detected significantly more lesions (56/75=75 %) than did FDG PET (35/75=47 %) in 21 patients. This relation between FDG uptake, short CTN doubling time and progression of metastatic MTC had already been noted: of 11 patients with positive FDG PET, 6 died from metastatic disease and 4 had disease progression; of 12 patients with negative FDG PET, 1 had recurrent disease, and 11 had no evidence of clinical disease [31].
In 10 of the 18 patients of the Italian co-operative comparative study, FDOPA PET/CT identified significantly more lesions than FDG PET/CT and SRPET/CT, whereas in one patient FDG PET/CT revealed multiple liver lesions missed by both FDOPA PET/CT and SRPET/CT as well as two additional locoregional lymph nodes [32]. No additional lesions were identified by SRPET/CT.
The results of another study comparing FDG and SRPET in 18 patients with recurrent MTC are concordant: SRPET/CT achieved disease detection in 13 of 18 patients (72 %) and FDG PET/CT in 14 of 18 (78 %) patients; FDG revealed a total of 28 metastatic MTC regions and SRPET 23 regions [34]. Of eight patients with occult biochemical recurrence of MTC, FDG negative and FDOPA not performed, reported by Pałyga et al., SRPET/CT localised in two cases the recurrent cervical lymph nodes which were confirmed after resection [35]. The same proportion (one of four) was observed by another Polish team [36].
FDG showed a superior diagnostic performance when compared to all SPECT radiopharmaceuticals: 123I-MIBG [37, 38], pentavalent 99mTc-dimercaptosuccinic acid [4, 37, 39], 99m Tc-sestamibi [37] or somatostatin analogues for SRS [37, 39–41], with the exception of the earliest study [22]. SRS appeared to be less sensitive than conventional imaging at detecting the full extent of metastatic disease in 11 children and adolescents with hereditary MTC [42].
In conclusion, data have been obtained mostly in cases of rising tumour marker levels after thyroidectomy. In this context, imaging is recommended if CTN is >150 ng/ml [43]. FDOPA is the best tracer; an early image acquisition starting during the first 15 min is advised [14] (Fig. 1). In negative cases, FDG should be the next PET tracer, in particular if CEA levels are elevated or rapidly rising [27, 29–32], and SRPET when neither FDOPA nor FDG PET are contributive [34–36].
Merkel cell carcinoma
Merkel cell carcinoma (MCC) is a rare and aggressive NET derived from cells located in the basal layers of the epidermis. Its clinical behaviour is characterised by aggressive regional nodal invasion, distant metastases and a high rate of recurrence, appearing in the majority of cases within the first 6–12 months after initial diagnosis.
Whole-body imaging is useful to stage and restage the tumour as well as sentinel lymph node detection for resection. The functional imaging modalities proposed for the detection of distant lesions of MCC were, like in most NET, 131I-MIBG SPECT [44], SRS [45] and FDG PET [46].
MCC shares similarities with both cutaneous melanoma and small cell carcinoma of the lung, which both evidenced uptake of FDOPA. Our team [47] observed that FDOPA was taken up in two MCC cases and true-negative in one suspected recurrence on SRS. However, the contrast of the images was lower with FDOPA than with FDG. The team in Vienna obtained similar results on 5 FDOPA PETs vs 24 FDG PETs [48]. In further series, the elective radiopharmaceutical was FDG, with a clear utility to detect nodal basin involvement (sensitivity=83 %, specificity=95 % for FDG vs 0 and 86 % for MRI, respectively) [49], as well as distant metastases [50], performing better than SRS [51], but with some false-negative results [52] probably in less aggressive forms.
In conclusion, FDG should be the first-line functional examination in MCC. When negative, it could be completed with SRPET.
Small cell lung cancer
Being a whole-body technique, PET can play a major role for a rapid staging of small cell lung cancer (SCLC) needed by the urgent therapeutic decision: FDG PET has been proposed for this purpose [53]. Since SCLC shares metabolic characteristics with NET, we speculated that FDOPA could be useful, being more specific than FDG and able to detect brain metastases. FDOPA and FDG PET were performed in four patients with newly diagnosed SCLC [54]. FDOPA PET appeared less sensitive than FDG PET and standard imaging procedures in the staging of SCLC. The utility of FDG PET for SCLC imaging has been confirmed in larger series [55].
In conclusion, FDG and not FDOPA is the reference tracer in SCLC.
Bronchial carcinoids
Bronchial carcinoids (BC) are histologically classified into typical (ca. 90 %) or atypical, with consequences on management. To the best of our knowledge, only a few cases have been reported using FDOPA PET: one was positive only on early images [56], and, by pooling the results of two comparative studies [56, 57] in a total of 8 patients, the FDOPA patient-based detection rate was 4/8 =50 % vs 7/8 =88 % for SRPET which showed more foci than FDOPA in 2/4 cases.
SRPET/CT was performed in 11 patients to stage BC; the detection rate was 9/11 =82 %, leading to a change in management of 3 of these 9 patients [58]. FDG uptake by the primary BC lesion is also frequent: by pooling the results of 4 studies, it was 36/42 =86 % [59–62]. However, no metastatic BC was included in those series.
Very concordant results can be derived from two comparative studies of SRPET/CT and FDG PET/CT [63, 64], in a total of 24 typical and 9 atypical BC: typical BC showed higher and more selective uptake on SRPET/CT than on FDG PET/CT, while the reverse was observed for atypical BC and higher grades of lung NET. Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia showed no uptake either on SRPET/CT or on FDG PET/CT. These results are in accordance with the classification of BC into the “foregut” group [65], with good overall results for SRS or SRPET in cases of well-differentiated NET.
In conclusion, if BC staging is found clinically useful, SRPET could be recommended, except in cases of atypical BC where FDG could be recommended as first line.
Paraganglioma, phaeochromocytoma and glomus tumour
Paragangliomas (PG) derive from the sympathetic or the parasympathetic systems, which comprise phaeochromocytomas derived from chromaffin cells in the adrenal gland, extra-adrenal sympathetic PG and parasympathetic PG, in particular glomus tumours and chemodectomas. The current reference radiopharmaceutical for scintigraphy is MIBG that traces expression of tumour-specific catecholamine transport and storage mechanisms by phaeochromocytoma/PG cells, even though SRS might be considered to supplement 123I-MIBG in suspicious metastatic phaeochromocytomas [66].
Several PET radiopharmaceuticals have been proposed, tracing the catecholamine pathway: FDOPA, its metabolite FDA [67], and 11C-hydroxyephedrine [68, 69]. FDOPA PET imaging of phaeochromocytoma was proposed by Hoegerle et al. in 2002 [70]. FDOPA PET, 123I-MIBG scintigraphy and MRI were performed in 14 consecutive patients suspected of having phaeochromocytomas [5 sporadic and 9 with von Hippel-Lindau (VHL) syndrome]. Both FDOPA PET and MRI detected 17 phaeochromocytomas (11 solitary, 3 bifocal; 14 adrenal, 3 extra-adrenal). Sensitivity was 100 % for FDOPA PET vs 71 % for 123I-MIBG scintigraphy, and specificity was 100 % for both procedures.
Since then, several studies have been published [17, 70–87] (Table 2) and also European Association of Nuclear Medicine (EANM) guidelines [80]. A recent meta-analysis of 11 studies comprising 275 patients with suspected PG [81] found that pooled sensitivity of FDOPA PET(/CT) in detecting PG was 91 % (patient based) and 79 % (lesion based). The pooled specificity of FDOPA PET(/CT) was 95 % for both patient-based and lesion-based analyses. FDOPA PET(/CT) seems to be accurate in both adrenal [17, 70–72] or extra-adrenal [73, 75–77], sympathetic [70–72, 74] or parasympathetic [73, 75–77], functioning [74] or non-functioning [71, 73, 76] and metastatic or non-metastatic PG [75, 79, 82] or VHL [70, 83, 84] PG.
When compared to 123I-MIBG [74, 77, 79], SRS [76], MRI [73, 74] or CT [74], FDOPA had the best diagnostic performance. In particular FDOPA is very sensitive for detecting head and neck PG, usually derived from parasympathetic ganglia [73, 76]. In contrast, no MIBG uptake is detected when expression of vesicular monoamine transporter 1 is lacking [77].
In the series of Charrier et al. [76], FDOPA PET detected significantly more cervical than abdominal lesions (97 vs 67 %); in two patients with the succinate dehydrogenase subunit D (SDHD) mutation, FDOPA PET missed five abdominal PG lesions, which were detected by the combination of SRS, 131I-MIBG and FDG. In other studies, SDHD mutation was associated with good FDOPA patient-based detection rate: eight of ten [73], five of six [77], seven of seven [78], eight of eight [84] and four of four [82], overall 91 %.
The comparison with FDG or FDA should be performed according to PG aggressiveness (Fig. 2) and genetic mutations. In 2009 Timmers et al. published a comparative study of 52 patients [82] using FDOPA PET, 123I-MIBG scintigraphy, FDA PET/CT and FDG PET/CT. It should be noted that FDOPA imaging was performed with a PET only machine of a former generation than PET/CT used for the two other PET tracers. In 15 patients with succinate dehydrogenase subunit B (SDHB) mutation, FDA and FDG had a higher overall lesion-based sensitivity (82 and 83 %) than 123I-MIBG (57 %) and FDOPA (20 %). In 13 patients without SDHB mutation, including 4 patients with SDHD mutation, FDOPA had the best lesion-based sensitivity (93 %), followed by FDA (76 %), 123I-MIBG (59 %) and FDG (62 %).
Right block of images FDOPA PET/CT: anterior and left lateral maximum intensity projection, transverse slice. Left block corresponding FDG PET/CT images. FDOPA PET/CT was performed for characterising a left adrenal tumour (dashed arrow) discovered incidentally on FDG PET/CT performed for staging a squamous cell carcinoma of the anal canal (full arrow) in an asymptomatic patient. As the adrenal tumour took up both FDOPA and FDG, it was interpreted as an aggressive phaeochromocytoma. This was confirmed on histological examination. This observation illustrates the increase in specificity brought by FDOPA for characterising NET
As somatostatin receptors are expressed by 73 % of phaeochromocytomas and 93 % of PG [85], SRS is an alternative. In the limited comparative studies, its sensitivity was less than that of FDOPA but greater than that of 123I-MIBG, in particular in head and neck PG [76, 78] or to detect metastatic sites of malignant phaeochromocytoma [66]. Concordantly, the superiority of SRPET over 123I-MIBG SPECT to pick up head and neck PG lesions and bone metastases has been confirmed recently in a series of 15 patients [86]. For the moment, there is no comparative study between FDOPA and SRPET(/CT) in this context.
Concerning the impact of FDOPA PET on the management of PG patients, the rate of change in patient management was, in our series, 3/24 (12 %) overall and 3/15 (20 %) in proven phaeochromocytoma, leading to pertinent decisions [87]. In the prospective study by Fiebrich et al., FDOPA PET influenced treatment decisions in 14/48 patients (29 %) [74].
In conclusion, a strategy of examinations in the diagnostic workup of PG/phaeochromocytoma could be to perform FDOPA PET/CT as first-line examination, except in patients with clinically aggressive forms or with SDHB mutation in whom FDG (or FDA if available) should be preferred.
Well-differentiated carcinoid tumours of the digestive tract of a midgut origin
Endocrine tumours of the gastrointestinal tract are characterised by a great heterogeneity. The midgut carcinoid, originating from enterochromaffin Kulchitsky cells in the crypts of Lieberkühn in the small intestine, has a relatively high tendency to metastasise via local lymph nodes to the liver; in this context, most patients present with carcinoid syndrome, including symptoms of flushing, diarrhoea, bronchoconstriction and right-sided heart failure caused by overproduction of substances such as serotonin and tachykinins. Serotonin is produced by the carcinoid tumour cells. Concerning the performance of SPECT radiopharmaceuticals, by pooling the results of two comparative series, the patient-based detection rate was 64/71 =90 % for SRS vs 48/71 =68 % for MIBG [62, 88]. In one series aggregating the results of carcinoid tumours of various origins, the detection rate was also better for SRS: 67 vs 50 % for 123I-MIBG [89].
The initial case with FDOPA imaging in a NET reported by Hoegerle et al. in 1999 [90] was a patient with metastasising carcinoid in whom various imaging procedures were not successful in detecting the primary tumour. Due to the importance of primary tumour proof for potential curative surgical therapy, FDOPA PET was performed that enabled localisation of a potential primary tumour in the ileum. Moreover, in addition to the known abdominal lymph node and liver metastases, it detected a mediastinal lymph node metastasis and a pulmonary metastasis.
Hoegerle et al. [91] subsequently demonstrated, in 16 patients with gastrointestinal carcinoid tumours, that lesion-based sensitivity was 65 % for FDOPA PET, better than 57 % for SRS and 29 % for FDG PET; however, the midgut origin of all tumours was not ascertained.
Possible detection of metastatic lesions with FDG was reported in 8/11 patients with NET of midgut or unknown origin [92]; SRS detected NET in 10/11 patients. The detection rate of FDG PET was less in another series [93]: metastatic NET of the small intestine was visible in only one of four cases.
In 24 patients with abdominal carcinoid tumours and biochemical proof of increased serotonin metabolism, per-patient analysis showed sensitivities of 100 % for 5-HTP, 96 % for FDOPA, 86 % for SRS and 96 % for CT [18]. Per-lesion analysis revealed sensitivities of 78 % for 5-HTP PET, 89 % for 5-HTP PET/CT, 87 % for FDOPA PET, 98 % for FDOPA PET/CT, 49 % for SRS, 73 % for SRS SPECT/CT and 63 % for CT alone. FDOPA detected significantly more lesions than SRS and than 5-HTP.
This very elective FDOPA uptake by midgut NET made it possible, in three patients, to differentiate on PET between metastases of NET and a second primary malignancy, an FDG-positive adenocarcinoma [94]. Metachronous cancers frequently develop in patients with small intestine carcinoid tumours (29 % according to Amin et al. [95]) and deserve full staging and treatment. A similar case is reported on in Fig. 3.
a–b In a haemodialysed patient candidate for renal grafting, systematic CT discovered a tumour of the terminal ileum evocative of a carcinoid origin with mesenteric locoregional adenopathies, the largest being 35 mm in size. Biopsy of a right iliac adenopathy confirmed a metastatic well-differentiated NET (Ki-67<1 %). FDOPA PET/CT performed for staging showed the primary carcinoid tumour in the terminal ileum (a dotted arrow) and large lymphadenopathy with two satellite lymph nodes (a black arrows), but also a focus in the upper left abdomen, SUVmax =4.7 (a, b green arrow) corresponding on CT to a dense content in a renal cyst. c FDG PET/CT was performed to better characterise the renal anomaly that took up FDG (c green arrow on the transverse slice) with a somewhat lower intensity than FDOPA (SUVmax = 3.9). As expected, the metastatic carcinoid tumour in the right abdomen did not take up FDG (c). Thus the renal cystic lesion was probably not of a carcinoid origin. A CT-guided biopsy of the renal lesion was performed and histology revealed a renal carcinoma. This observation illustrates the ability of FDOPA to detect carcinoid tumours with low aggressiveness, but also renal carcinomas, and the synergy between FDOPA and FDG PET/CT
In a series of 77 patients with digestive NET [96], the large majority (82 %) being of midgut origin, FDOPA uptake on PET reflected tumour load. Patient whole-body metabolic tumour burden determined on FDOPA PET/CT was correlated with urinary serotonin, urinary and plasma 5-hydroxyindoleacetic acid (5-HIAA), urinary norepinephrine, epinephrine, dopamine and plasma dopamine, but not with serum chromogranin A (CgA).
Comparison with SRPET is currently only available in a few cases. In the series of Ambrosini et al., PET/CT results were concordant in two cases with multiple lymph node and/or liver lesions [57], FDOPA showing more lesions in one case and SRPET in the other one. In the series of Haug et al., four NET in patients with serotonin levels >700 ng/ml originated from the ileum, and all were FDOPA positive and SRPET positive [97]. An interim analysis of the on-site readings of a prospective study that we are currently performing demonstrated that, in 14 patients with a carcinoid tumour of the ileum, the patient-based sensitivity was 100 % for both FDOPA PET/CT and SRPET/CT but FDOPA showed more uptake foci in 8/14=44 % of patients [98]. In summary, in all 20 patients, both tracers were able to detect lesions of midgut carcinoid NET, FDOPA showing more lesions in 9/20= 45 % of patients and SRPET in 1/20= 5 % of patients.
The rate of change in management was 50 % in our series of 22 patients with histologically documented carcinoid tumour of the ileum, relevant in all cases according to follow-up data [21]. In the series of 16 digestive carcinoid tumours of Hoegerle et al. [91], FDOPA PET resulted in modification or even complete change in therapeutic strategy in 31 % of cases.
In conclusion, using FDOPA PET/CT as the first-line functional imaging modality for the management of digestive NET originating from midgut allows small lesions to be detected and corresponds to its MA [18, 20, 91, 99] (Table 3). FDOPA imaging induced relevant changes in patient management [21, 91]. Its superiority over SRS has been confirmed by several teams. SRPET appears to be a competitor, although it showed less foci in some patients; dedicated comparative studies are currently lacking. With FDG PET, very limited results have been reported in midgut NET [91–93]; FDG is able to show some metastatic lesions of intestinal NET, but a significant FDG uptake in this context should also be a warning sign of a metachronous “common” cancer [94].
Neuroendocrine tumours of the digestive tract of hindgut origin (transverse and left colon and rectum)
Hindgut carcinoids metastasise in about 3–5 % of cases and rarely present hormonal symptoms or elevation of urinary-5-HIAA despite the content of peptides and hormones. Globally, these NET are more aggressive and more often poorly differentiated than NET originating from midgut [100].
To the best of our knowledge, no study with FDOPA has been reported in this NET; only two FDOPA-positive SRS-positive cases were reported in the series of Hogerle et al. [90] and three FDOPA-negative SRPET-positive cases in patients with serotonin levels <200 ng/ml in the series of Haug et al. [97]. The patient-based detection rate was 5/6 for FDG vs 4/6 with SRS in the study of Binderup et al. [62] and 5/6 with SRS in the study of Ezziddin et al. [88], MIBG being ineffective in both series (2/12=17 %). Case reports describe FDG imaging and treatment monitoring in aggressive metastatic NET, also referred to as small cell colorectal cancer [101, 102].
In conclusion, in cases of NET tumours of the rectum or the transverse and left colon, FDG and/or SRPET are able to localise the lesions, even if evidence is currently limited about the impact of the examination.
Endocrine pancreatic tumours (except hyperinsulinism in infants), NET of the stomach or the duodenum
Endocrine pancreatic tumours (EPT) are part of foregut NET and include insulinomas, gastrinomas, VIPomas, glucagonomas, somatostatinomas and non-functioning NET. In malignant tumours, mixed syndromes are common due to multiple hormone production from the tumours. In about one third of EPT, the patients present no hormonal symptoms, bearing a non-functioning NET. EPT can also be part of type I multiple endocrine neoplasia (MEN-I) syndrome, in which multiple pancreatic tumours are almost always found. Concerning the performance of SPECT radiopharmaceuticals, by pooling the results of 3 comparative series, the patient-based detection rate was 47/52 =90 % for SRS vs 17/52 =33 % for MIBG [62, 88, 89].
Only 11/22=50 % of the EPT could be detected with 11C-L-DOPA; in 2 additional patients, CT enabled detection of tumours not detected on PET [103]. We reported concordant results with FDOPA in 10 EPT [20]: poor patient-based sensitivity of 2/8=25 %, contrasting with a better sensitivity of SRS: 6/8=75 %. Concerning other radiopharmaceuticals for SPECT, by pooling the results of 3 comparative series in EPT, MIBG had a low patient-based detection rate of 11/52= 21 % vs 47/52 =90 % for SRS [62, 88, 89]. 111In-glucagon-like peptide 1 (GLP-1) receptor scintigraphy has been proposed specifically for insulinoma [104].
The article of Koopmans et al. in 2008 [18] included 23 patients with pancreatic islet cell tumours; 39 % of patients had biochemical proof of increased serotonin metabolism. Patient-based sensitivity was 100 % for 5-HTP PET, 89 % for FDOPA PET, 78 % for SRS and 87 % for CT. Per-lesion analysis revealed sensitivities of 67 % for 5-HTP PET, 96 % for 5-HTP PET/CT, 41 % for FDOPA PET, 80 % for FDOPA PET/CT, 46 % for SRS, 77 % for SRS SPECT/CT and 68 % for CT alone. Although 5-HTP PET/CT was superior to FDOPA PET/CT in islet cell tumours, 11C-5-HTP cannot be produced and delivered for routine use as easily as FDOPA. In contrast with our results, FDOPA PET/CT had better sensitivity than SRS, even performed with SPECT/CT fusion.
Insulinoma may constitute an indication for FDOPA, as the sensitivity of SRS has been reported to be limited. Currently, only small series have been reported. The detection rate was 9/10=90 % in the series of Kauhanen et al. [105], but another preliminary study reported a poor detection rate [106]: in 5 adults with hyperinsulinism, no tumour was detected with FDOPA while CT was positive in 4 cases; the only FDOPA detection occurred in 1 child with multiple NET MEN-I.
FDOPA PET was compared with SRPET in very small series. Its performance was equal to that of 68Ga-DOTATOC in four EPTs reported by Putzer et al. [107]. In the series of Ambrosini et al., the per-patient detection rate was 5/8 for FDOPA vs 8/8 for 68Ga-DOTANOC [57] which showed more foci in 4 of the 5 FDOPA-positive patients. In another series of five EPTs, FDOPA was positive in three cases whereas SRPET was positive in all cases [97]. Since FDOPA has a limited sensitivity for most types of EPT and a good one for midgut digestive NET, in series mixing several types of NET, its overall sensitivity and the result of comparison with SRPET depend on the relative proportions of those different types of NET.
No series have been identified concerning stomach or duodenal NET, also part of foregut digestive NETs, and only a few cases in larger series: patient-based sensitivity of 1/4=25 % for FDOPA vs 3/5=75 % for SRS [20] or of 2/4=50 % for FDOPA vs 3/4=75 % with SRPET (pooling results of studies [57], [97] and [107]), SR-based imaging usually showing more foci.
In the case of an aggressive form of well-differentiated NET with Ki-67 >10 %, the first-line tracer should be FDG: in 18 patients (15 with foregut NET), FDG patient-based sensitivity was 100 % vs 83 % for SRS, and FDG PET detected more lesions than SRS in 78 % of cases [108]. When no selection was made on Ki-67 value, the detection rate in 29 patients was 79 % for FDG and less than 90 % for SRS [62].
In conclusion, in cases of differentiated EPT, SRPET is the first-line examination, except if Ki-67 >10 % favours FDG PET. If negative, FDOPA can be useful, in particular in gastric or duodenal NET as well as in some cases of positive SRPET or FDG PET when there is a doubt about the nature of a positive focus: FDOPA is more tumour specific than the somatostatin analogues or FDG which are taken up by leucocytes in inflammatory lesions.
Congenital hyperinsulinism in infants
Although insulinoma, a digestive NET generally of a benign nature, induces hyperinsulinism, congenital hyperinsulinism (CHI) is a specific clinical setting, as clustered beta-cell hyperplasia is found in the resectable cases, rather than a definite tumour. Although this indication does not strictly belong to oncology, the excellent performance of FDOPA will be briefly summarised.
In infants with CHI, which results in life-threatening hypoglycaemia, the aim of imaging is to localise focal hyperplasia of beta cells in the pancreas: hyperinsulinism with focal lesion(s) can revert by selective surgical resection, in contrast to the diffuse form, which requires subtotal pancreatectomy when resistant to medical treatment.
In the initial study by Ribeiro et al. on 15 CHI children (aged 1–14 months) [11], FDOPA PET showed an abnormal focal pancreatic uptake in 5 patients who then underwent a limited pancreatic resection that was followed by a complete clinical remission. A diffuse pancreatic uptake was observed in ten patients, four of whom underwent surgical resection that confirmed FDOPA PET results: the abnormal beta cells were gathered in small clusters, scattered in the whole pancreas. In contrast, MRI performed in six infants showed no anomaly.
These very promising results were confirmed in larger series by the same team and by many others [109–114] (Fig. 4). In a recent German study [114], FDOPA PET/CT with multiphase contrast media protocols was performed in 135 CHI patients. All the foci were excised on the basis of FDOPA PET/CT images and 87–91 % of the operated patients could be completely healed.
FDOPA PET/CT: maximum intensity projection, transverse slice and coronal slice. Search for focal hyperplasia of pancreatic beta cells in an infant with hyperinsulinism. FDOPA PET/CT localised a focus in the tail of the pancreas which was resected. Histological examination confirmed clustered beta-cell hyperplasia and the infant became euglycaemic
Two meta-analyses have been recently published. An Italian team concluded that the pooled sensitivity and specificity of FDOPA PET(/CT) in differentiating between focal and diffuse CHI were 89 and 98 %, respectively [115]. An American team aimed to compare the diagnostic performance of FDOPA PET, pancreatic venous sampling (PVS) and selective pancreatic arterial calcium stimulation with hepatic venous sampling (ASVS) in diagnosing and localising focal CHI [116]. FDOPA PET was superior in distinguishing focal from diffuse CHI [summary diagnostic odds ratio (SDOR)= 73.2], compared to PVS (SDOR= 23.5) and ASVS (SDOR= 4.3). Furthermore, it localised focal CHI in the pancreas more accurately than PVS and ASVS (pooled accuracy 82 vs 76 and 64 %, respectively).
In conclusion, the results of recently published large series are in accordance with the initial ones: FDOPA PET(/CT) is of major utility to select those infants for surgery and shortens the intervention by guiding the surgical exploration of the pancreas.
“Carcinoids” or “endocrine small cell” or “oat cell” tumours of other organs
Carcinoid tumours can be observed in several others organs. Probably due to the urinary excretion of radiopharmaceuticals, their use seems limited in NET of the kidney or the urinary bladder to detection and treatment follow-up of metastases, as reported by Iagaru et al. using FDG PET [117]. The published case reports with nuclear imaging are focused on two sites, thymus and prostate, but none reported the use of FDOPA.
In summary, thymic NETs are aggressive and diagnosed at an advanced stage. FDG was able to accurately stage one patient with lymph node and bone metastases, which were not visible either on MIBG or on bone scintigraphies [118], and to restage a recurrent thymic NET with multiple bone metastases which were not visible on bone scintigraphy [119]. In contrast, SRPET did not show any thymic NET in the four cases of another series [120]. These preliminary results seem somewhat discrepant with a foregut origin currently accepted for thymus NET.
Small cell carcinoma of the prostate (SCCP) is very aggressive, metastasises early and does not respond to most chemotherapy regimens. In approximately 50 % of cases of prostate cancer, tumours are a combination of small cell carcinoma and androgen-sensitive adenocarcinoma. Our team performed FDOPA PET in four patients that did not show the NET contingent of the prostate cancer which was either demonstrated at histological examination (one case taking up FDG) or suspected on high serum levels of CgA. In 2002, Spieth et al. [121] reported in one SCCP patient that SRS was more sensitive than bone scintigraphy to detect metastatic foci. More recently, the use of FDG PET has been reported in case reports for detecting SCCP [122–124] and monitoring therapy [125].
In conclusion, in those aggressive NETs, FDG PET/CT seems to be the best first-line examination.
Detection of unknown primary NET: NET metastases of unknown origin, ectopic hormone secretion, or suspicion of NET or of MEN
Concerning NET metastases of unknown origin (“CUP-NET”), the localisation of the primary tumour is important to optimise patient management [126]. The choice of the best tracer depends on the most probable primary tumour and on its aggressiveness. As FDG was superior to SRS to detect metastatic NET, in correlation with Ki-67 [127], FDG could be tried first in CUP-NET if Ki-67 is >10 %. High levels of a biochemical marker may provide guidance: serotonin or urinary 5-HIAA or catecholamine derivates or calcitonin favour using FDOPA [96, 97]. Immunohistochemistry may also help. The presence of CDX-2 in metastases had a specificity of 100 % and a sensitivity of 40 % for a midgut primary NET, favouring FDOPA imaging [128]. The presence of Islet 1 in metastases had a specificity of 100 % and a sensitivity of 78 % for a primary EPT [128]. PDX-1 was positive in five of five cases of metastatic pancreatic NET and two of two cases of metastatic duodenal NET [129] and TTF-1 was expressed almost only in bronchopulmonary NET [128, 129]. Thus, the presence of those markers favours SRPET. Other markers for immunochemistry of NET have already been described and more will come in future.
As early as 1999, Hoegerle et al. reported a CUP-NET case and the successful delineation of the primary carcinoid tumour with FDOPA PET [90]. Our team reported detection of the primary tumour with FDOPA in 6 of 16 CUP-NET (38 %); in 5 other patients, FDOPA PET upstaged the disease but did not reveal a subsequently confirmed primary NET [21].
Series have also been reported using SRPET. The detection rate of primary tumour was 5/14 [36], 4/4 [97], 3/4 [130], 35/59 [131] and 12/20 [132], overall 59/101=58 %. SRPET could be compared with FDOPA in 4 such patients reported by Haug et al. in 2009 [97]: in 2/4 patients, “FDOPA PET allowed better delineation of the primary tumour, and gave evidence of more metastases, mainly due to higher tumour/non-tumour contrast, which was especially seen in the liver”.
Concerning ectopic hormone secretion, PET has been reported in cases of adrenocorticotropic hormone (ACTH) production, which is generally due to lung or carcinoid tumours. In one case, FDOPA successfully detected a BC [56] and in another case a carcinoid of the appendix [133]. In another case, CT demonstrated prominent lymph nodes in the left lung hilum and hyperplastic adrenals but no primary tumour, SRPET/CT was non-contributive, but FDOPA PET/CT localised the metastatic BC [134].
In our centre, eight FDOPA PET/CTs were performed in this setting and two were positive; surgery was performed in one of them, in view of concordance with positive FDG PET/CT, and a thoracic NET was confirmed.
Other cases have been reported using either FDG, the primary NET being a recurrent thymic carcinoid tumour [135], an atypical thymic carcinoid tumour [136] or a hepatic carcinoid tumour [137], or 5-HTP, the primary NET being BC [138], or SRPET that detected a NET of the ileum [139] and a NET in the right sphenoidal sinus [140].
One series of 41 patients has been reported by Zemskova et al. but several imaging modalities were used, not in all patients, with intervals of several months, PET being performed as a second-line examination when others were not conclusive; so, performance of modalities cannot be compared [141]. Patient-based sensitivity was overall 6/13=46 % for FDOPA PET and 7/14=50 % for FDG PET; an important point was the remarkable specificity of FDOPA, in contrast to CT, MRI, SRS and FDG, leading to a very high positive predictive value (PPV). FDOPA PET improved PPV of CT/MRI, while FDG PET did not.
Concerning the localisation of parathyroid adenoma in the case of high serum levels of parathyroid hormone, FDOPA PET was negative in all eight patients reported by Lange-Nolde et al. [142] and could not compete with ultrasonography or with 99mTc-sestamibi scintigraphy. We share the same experience and parathyroid adenomas did not take up FDOPA when present in patients with MEN1.
MEN1 consists of benign or malignant tumours derived from at least two of the following cell types: parathyroid cells, gastrin cells or prolactin-producing pituitary cells. The same negative result was reported with SRPET/CT: of three parathyroid gland adenomas, two were detected by CT only and one remained totally undetected by hybrid imaging [143]. However, in this study, SRPET/CT was able to detect other tumours in 19 patients referred for a MEN1 syndrome, lesion-based sensitivity was 92 % and specificity 93.5 %. Not only 60 NET lesions were detected but also 31 benign MEN-associated lesions. A change in management was induced in 9/19=47 % of patients.
MEN2 associates as the main NET tumours MTC and phaeochromocytoma the detection of which has already been discussed above. FDA [144] or FDOPA could be favoured, as FDG is of little help. In a series, FDG PET could not identify MTC foci within the thyroid in 14 MEN2A patients, but identified 2 true-positive and 1 false-positive lymph node metastases [145]. In another series, none of the six patients with MEN2A syndrome had a positive FDG PET/CT for MTC [146].
Concerning the detection of NET when only suspected, some data are available in cases of evocative clinical symptoms, or of biological suspicion based on tumour marker levels or of a suspected NET on imaging.
In a comparative study of FDOPA PET/CT and SRS in 61 patients, FDOPA PET/CT correctly identified 32 of 36 patients who actually had a NET, with a sensitivity of 91 %, significantly greater than that of SRS (59 %), and a specificity of 96 vs 86 % for SRS [147]. In 16/61=26 % of the patients, the management was altered as a result of new findings on FDOPA PET/CT.
In a subgroup of 13 patients with suspected NET from a larger series, SRPET had a sensitivity of 4/4=100 % vs. 2/4=50 % for SRS, the specificity being 8/9=89 % for both modalities [148]. In a larger series, 70 patients were examined by SRPET/CT primarily because of the clinical suspicion of NET on the basis of symptoms such as persistent diarrhoea or flushing, 49 patients because of elevated levels of tumour markers and 53 patients because of a mass suggestive of NET [149]. Only one third of the patients included in the study group proved to have a NET, the most frequent localisation of which was the small bowel (10/36=28 %); patient-based sensitivity was 81 % and specificity 90 %. No conclusion can be drawn from the somewhat better sensitivity of FDOPA PET/CT (91 %) [147] vs SRPET/CT (81 %) [149] as those two studies, of a similar sample size, were not comparative; the relatively high frequency of small bowel NET in this setting is concordant with a good performance of FDOPA.
An interesting point is the high proportion of unconfirmed suspicion of NET in the three studies (overall 102/178=57 %). This can be explained by the lack of specificity of the clinical signs or of the aspect of the tumour on conventional imaging; but a selection based on chromogranin-A or on neuron-specific enolase (NSE) serum levels was not more effective: NET was confirmed only in 16/49=33 % of such cases in the series of Haug et al. [149] . Of the 43 patients with elevated levels of chromogranin-A, just 12 (29 %) had histologically proven NET and the diagnostic performance of SRPET was not better in this subgroup of patients. According to our experience, patients are too frequently referred for a sophisticated imaging examination due to a non-specific rise in chromogranin-A levels in relation to proton pump inhibitor treatment [150]. Short-term proton pump inhibitor use (7 days only) results in a significant increase of chromogranin-A levels; proton pump inhibitors need to be discontinued for 2 weeks to fully eliminate their effect on chromogranin-A levels [151]. A simpler alternative is to assay markers which are not affected by this very frequent treatment in patients with digestive disorders; pancreastatin has recently been proposed [152]. Concerning NSE, not all clinicians are aware of the importance of processing the blood sample: haemolysis or conservation at room temperature result in meaningless high results [153].
In conclusion, FDOPA, FDG and SRPET/CT can detect the primary NET in a significant number of patients with metastatic NET. The sequence of those examinations will be guided by physical signs, serum markers, immunochemistry and also the availability of the tracers at the PET centre. FDOPA and SRPET/CT can detect suspected primary NET, serum markers being useful to choose the first-line examination when both are available, associated infection or inflammation favouring FDOPA. Causes of a non-specific rise in tumour marker serum levels should be considered and ruled out.
References
Panzuto F, Nasoni S, Falconi M, Corleto VD, Capurso G, Cassetta S, et al. Prognostic factors and survival in endocrine tumor patients: comparison between gastrointestinal and pancreatic localization. Endocr Relat Cancer 2005;12:1083–92.
Lebtahi R, Cadiot G, Delahaye N, Genin R, Daou D, Peker MC, et al. Detection of bone metastases in patients with endocrine gastroenteropancreatic tumors: bone scintigraphy compared with somatostatin receptor scintigraphy. J Nucl Med 1999;40(10):1602–8.
Janson ET, Westlin JE, Eriksson B, Ahlström H, Nilsson S, Öberg K. [111In-DTPA-D-Phe1]octreotide scintigraphy in patients with carcinoid tumours: the predictive value for somatostatin analogue treatment. Eur J Endocrinol 1994;131(6):577–81.
Adams S, Baum R, Rink T, Schumm-Dräger PM, Usadel KH, Hör G. Limited value of fluorine-18 fluorodeoxyglucose positron emission tomography for the imaging of neuroendocrine tumours. Eur J Nucl Med 1998;25(1):79–83.
Pasquali C, Rubello D, Sperti C, Gasparoni P, Liessi G, Chierichetti F, et al. Neuroendocrine tumour imaging: can 18F-fluorodeoxyglucose positron emission tomography detect tumors with poor prognosis and aggressive behavior. World J Surg 1998;22:588–92.
Pearse AG. The cytochemistry and ultrastructure of polypeptide hormone-producing cells of the APUD series and the embryologic, physiologic and pathologic implications of the concept. J Histochem Cytochem 1969;17(5):303–8.
Bergström M, Eriksson B, Öberg K, Sundin A, Ahlström H, Lindner KJ, et al. In vivo demonstration of enzyme activity in endocrine pancreatic tumors: decarboxylation of carbon-11-DOPA to carbon-11-dopamine. J Nucl Med 1996;37(1):32–7.
Bomanji JB, Papathanasiou ND. 111In-DTPA0-octreotide (Octreoscan), 131I-MIBG and other agents for radionuclide therapy of NETs. Eur J Nucl Med Mol Imaging 2012;39 Suppl 1:S113–25.
Eriksson B, Örlefors H, Oberg K, Sundin A, Bergström M, Långström B. Developments in PET for the detection of endocrine tumours. Best Pract Res Clin Endocrinol Metab 2005;19(2):311–24.
Timmers HJ, Hadi M, Carrasquillo JA, Chen CC, Martiniova L, Whatley M, et al. The effects of carbidopa on uptake of 6-18F-fluoro-L-DOPA in PET of pheochromocytoma and extraadrenal abdominal paraganglioma. J Nucl Med 2007;48:1599–606.
Ribeiro MJ, De Lonlay P, Delzescaux T, Boddaert N, Jaubert F, Bourgeois S, et al. Characterization of hyperinsulinism in infancy assessed with PET and 18-fluoro-L-DOPA. J Nucl Med 2005;46:560–6.
Kauhanen S, Seppänen M, Nuutila P. Premedication with carbidopa masks positive finding of insulinoma and beta-cell hyperplasia in [(18)F]-dihydroxy-phenyl-alanine positron emission tomography. J Clin Oncol 2008;26:5307–8.
Becherer A, Szabó M, Karanikas G, Wunderbaldinger P, Angelberger P, Raderer M, et al. Imaging of advanced neuroendocrine tumors with (18)F-FDOPA PET. J Nucl Med 2004;45:1161–7.
Soussan M, Nataf V, Kerrou K, Grahek D, Pascal O, Talbot JN, et al. Added value of early 18F-FDOPA PET/CT acquisition time in medullary thyroid cancer. Nucl Med Commun 2012;33(7):775–9.
Hentschel M, Rottenburger C, Boedeker CC, Neumann HP, Brink I. Is there an optimal scan time for 6-[F-18]fluoro-L-DOPA PET in pheochromocytomas and paragangliomas? Clin Nucl Med 2012;37(2):e24–9.
Luster M, Karges W, Zeich K, Pauls S, Verburg FA, Dralle H, et al. Clinical value of 18-fluorine-fluorodihydroxyphenylalanine positron emission tomography/computed tomography in the follow-up of medullary thyroid carcinoma. Thyroid 2010;20(5):527–33.
Luster M, Karges W, Zeich K, Pauls S, Verburg FA, Dralle H, et al. Clinical value of 18F-fluorodihydroxyphenylalanine positron emission tomography/computed tomography (18F-DOPA PET/CT) for detecting pheochromocytoma. Eur J Nucl Med Mol Imaging 2010;37(3):484–93.
Koopmans KP, Neels OC, Kema IP, Elsinga PH, Sluiter WJ, Vanghillewe K, et al. Improved staging of patients with carcinoid and islet cell tumors with 18F-dihydroxy-phenyl-alanine and 11C-5-hydroxy-tryptophan positron emission tomography. J Clin Oncol 2008;26(9):1489–95.
Becherer A, Novotny C, Leitha T. An unusual pitfall in 18F-FDOPA-PET. Nuklearmedizin 2005;44:A197. n°23.
Montravers F, Grahek D, Kerrou K, Ruszniewski P, de Beco V, Aide N, et al. Can fluorodihydroxyphenylalanine PET replace somatostatin receptor scintigraphy in patients with digestive endocrine tumors? J Nucl Med 2006;47(9):1455–62.
Montravers F, Kerrou K, Nataf V, Huchet V, Lotz JP, Ruszniewski P, et al. Impact of fluorodihydroxyphenylalanine-18F positron emission tomography on management of adult patients with documented or occult digestive endocrine tumors. J Clin Endocrinol Metab 2009;94(4):1295–301.
Hoegerle S, Altehofer C, Ghanem N, Brink I, Moser E, Nitzsche E. 18F-DOPA positron emission tomography for tumour detection in patients with medullary thyroid carcinoma and elevated calcitonin levels. Eur J Nucl Med 2001;28:64–71.
Treglia G, Cocciolillo F, Di Nardo F, Poscia A, de Waure C, Giordano A, et al. Detection rate of recurrent medullary thyroid carcinoma using fluorine-18 dihydroxyphenylalanine positron emission tomography: a meta-analysis. Acad Radiol 2012;19(10):1290–9.
Langsteger W, Heinisch M, Fogelman I. The role of fluorodeoxyglucose, 18Fdihydroxyphenylalanine, 18F-choline, and 18F-fluoride in bone imaging with emphasis on prostate and breast. Semin Nucl Med 2006;36:73–92.
Beuthien-Baumann B, Strumpf A, Zessin J, Bredow J, Kotzerke J. Diagnostic impact of PET with 18F-FDG, 18F-DOPA and 3-O-methyl-6-[18F]fluoro-DOPA in recurrent or metastatic medullary thyroid carcinoma. Eur J Nucl Med Mol Imaging 2007;34(10):1604–9.
Beheshti M, Pöcher S, Vali R, Waldenberger P, Broinger G, Nader M, et al. The value of 18F-DOPA PET-CT in patients with medullary thyroid carcinoma: comparison with 18F-FDG PET-CT. Eur Radiol 2009;19:1425–34.
Koopmans KP, de Groot JWB, Plukke JTM, de Vries EG, Kema IP, Sluiter WJ, et al. 18F-dihydroxyphenylalanine PET in patients with biochemical evidence of medullary thyroid cancer: relation to tumor differentiation. J Nucl Med 2008;49:524–31.
Marzola MC, Pelizzo MR, Ferdeghini M, Toniato A, Massaro A, Ambrosini V, et al. Dual PET/CT with (18)F-DOPA and (18)F-FDG in metastatic medullary thyroid carcinoma and rapidly increasing calcitonin levels: comparison with conventional imaging. Eur J Surg Oncol 2010;36(4):414–21.
Kauhanen S, Schalin-Jäntti C, Seppänen M, Kajander S, Virtanen S, Schildt J, et al. Complementary roles of 18F-DOPA PET/CT and 18F-FDG PET/CT in medullary thyroid cancer. J Nucl Med 2011;52(12):1855–63.
Verbeek HH, Plukker JT, Koopmans KP, de Groot JW, Hofstra RM, Muller Kobold AC, et al. Clinical relevance of 18F-FDG PET and 18F-DOPA PET in recurrent medullary thyroid carcinoma. J Nucl Med 2012;53(12):1863–71.
Bogsrud TV, Karantanis D, Nathan MA, Mullan BP, Wiseman GA, Kasperbauer JL, et al. The prognostic value of 2-deoxy-2-[18F]fluoro-D-glucose positron emission tomography in patients with suspected residual or recurrent medullary thyroid carcinoma. Mol Imaging Biol 2010;12(5):547–53.
Treglia G, Castaldi P, Villani MF, Perotti G, de Waure C, Filice A, et al. Comparison of 18F-DOPA, 18F-FDG and 68Ga-somatostatin analogue PET/CT in patients with recurrent medullary thyroid carcinoma. Eur J Nucl Med Mol Imaging 2012;39(4):569–80.
Montravers F, Grahek D, Kerrou K, Gutman F, Leverger G, Talbot J. Impact de la TEP à la fluoro-(18F)-dihydroxyphénylalanine (FDOPA) sur l’attitude thérapeutique en cas de tumeur endocrine: tumeur digestive, cancer médullaire de la thyroïde ou phéochromocytome. Med Nucl 2006;30(7):383–9.
Conry BG, Papathanasiou ND, Prakash V, Kayani I, Caplin M, Mahmood S, et al. Comparison of (68)Ga-DOTATATE and (18)F-fluorodeoxyglucose PET/CT in the detection of recurrent medullary thyroid carcinoma. Eur J Nucl Med Mol Imaging 2010;37(1):49–57.
Pałyga I, Kowalska A, Gąsior-Perczak D, Tarnawska-Pierścińska M, Słuszniak J, Sygut J, et al. The role of PET-CT scan with somatostatin analogue labelled with gallium-68 (68Ga-DOTA-TATE PET-CT) in diagnosing patients with disseminated medullary thyroid carcinoma (MTC). Endokrynol Pol 2010;61(5):507–11.
Łapińska G, Bryszewska M, Fijołek-Warszewska A, Kozłowicz-Gudzińska I, Ochman P, Sackiewicz-Słaby A. The diagnostic role of 68Ga-DOTATATE PET/CT in the detection of neuroendocrine tumours. Nucl Med Rev Cent East Eur 2011;14(1):16–20.
Diehl M, Risse JH, Brandt-Mainz K, Dietlein M, Bohuslavizki KH, Matheja P, et al. Fluorine-18 fluorodeoxyglucose positron emission tomography in medullary thyroid cancer: results of a multicentre study. Eur J Nucl Med 2001;28(11):1671–6.
Szakáll Jr S, Esik O, Bajzik G, Repa I, Dabasi G, Sinkovics I, et al. 18F-FDG PET detection of lymph node metastases in medullary thyroid carcinoma. J Nucl Med 2002;43(1):66–71.
De Groot JW, Links TP, Jager PL, Kahraman T, Plukker JT. Impact of 18F-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) in patients with biochemical evidence of recurrent or residual medullary thyroid cancer. Ann Surg Oncol 2004;11(8):786–94.
Gotthardt M, Battmann A, Höffken H, Schurrat T, Pollum H, Beuter D, et al. 18F-FDG PET, somatostatin receptor scintigraphy, and CT in metastatic medullary thyroid carcinoma: a clinical study and an analysis of the literature. Nucl Med Commun 2004;25(5):439–43.
Rubello D, Rampin L, Nanni C, Banti E, Ferdeghini M, Fanti S, et al. The role of 18F-FDG PET/CT in detecting metastatic deposits of recurrent medullary thyroid carcinoma: a prospective study. Eur J Surg Oncol 2008;34(5):581–6.
Lodish M, Dagalakis U, Chen CC, Sinaii N, Whitcomb P, Aikin A, et al. (111)In-octreotide scintigraphy for identification of metastatic medullary thyroid carcinoma in children and adolescents. J Clin Endocrinol Metab 2012;97(2):E207–12.
American Thyroid Association Guidelines Task Force, Kloos RT, Eng C, Evans DB, Francis GL, Gagel RF, Gharib H, et al. Medullary thyroid cancer: management guidelines of the American Thyroid Association. Thyroid 2009;19(6):565–612.
Castagnoli A, Biti G, De Cristofaro MT, Ferri P, Magrini SM, Papi MG, et al. Merkel cell carcinoma and iodine-131 metaiodobenzylguanidine scan. Eur J Nucl Med 1992;19(10):913–6.
Kwekkeboom DJ, Hof AM, Lamberts SWJ, Oei HY, Krenning EP. Somatostatin receptor scintigraphy. A simple and sensitive method for the in vivo visualization of Merkel cell tumors and their metastases. Arch Dermatol 1992;128:818–21.
Wong CO, Pham AN, Dworkin HJ. F-18 FDG accumulation in an octreotide negative Merkel cell tumor. Clin Positron Imaging 2000;3:71–3.
Talbot JN, Kerrou K, Missoum F, Grahek D, Aide N, Lumbroso J, et al. 6-[F-18]Fluoro-L-DOPA positron emission tomography in the imaging of Merkel cell carcinoma: preliminary report of three cases with 2-deoxy-2-[F-18]fluoro-D-glucose positron emission tomography or pentetreotide-(111In) SPECT data. Mol Imaging Biol 2005;7(4):257–61.
Peloschek P, Novotny C, Mueller-Mang C, Weber M, Sailer J, Dawid M, et al. Diagnostic imaging in Merkel cell carcinoma: lessons to learn from 16 cases with correlation of sonography, CT, MRI and PET. Eur J Radiol 2010;73(2):317–23.
Colgan MB, Tarantola TI, Weaver AL, Wiseman GA, Roenigk RK, Brewer JD, et al. The predictive value of imaging studies in evaluating regional lymph node involvement in Merkel cell carcinoma. J Am Acad Dermatol 2012;67(6):1250–6.
Golan H, Volkov O, Linchinsky O, Melloul M. FDG-PET imaging in Merkel cell carcinoma - value of head-to-toe scan. Nucl Med Rev Cent East Eur 2005;8(2):135–6.
Lu Y, Fleming SE, Fields RC, Coit DG, Carrasquillo JA. Comparison of 18F-FDG PET/CT and 111In pentetreotide scan for detection of Merkel cell carcinoma. Clin Nucl Med 2012;37(8):759–62.
Belhocine T, Pierard GE, Frühling J, Letesson G, Bolle S, Hustinx R, et al. Clinical added-value of 18FDG PET in neuroendocrine-Merkel cell carcinoma. Oncol Rep 2006;16(2):347–52.
Hauber HP, Bohuslaviki KH, Lund CH, Fritscher-Ravens A, Meyer A, Pforte A. Positron emission tomography in the staging of small-cell lung cancer: a preliminary study. Chest 2001;119(3):950–4.
Jacob T, Grahek D, Younsi N, Kerrou K, Aide N, Montravers F, et al. Positron emission tomography with [(18)F]FDOPA and [(18)F]FDG in the imaging of small cell lung carcinoma: preliminary results. Eur J Nucl Med Mol Imaging 2003;30:1266–9.
Brink I, Schumacher T, Mix M, Ruhland S, Stoelben E, Digel W, et al. Impact of [18F]FDG-PET on the primary staging of small-cell lung cancer. Eur J Nucl Med Mol Imaging 2004;31:1614–20.
Dubois S, Morel O, Rodien P, Illouz F, Girault S, Cahouet A, et al. A pulmonary adrenocorticotropin-secreting carcinoid tumor localized by 6-fluoro-[18F]L-dihydroxyphenylalanine positron emission/computed tomography imaging in a patient with Cushing’s syndrome. J Clin Endocrinol Metab 2007;92:4512–3.
Ambrosini V, Tomassetti P, Castellucci P, Campana D, Montini G, Rubello D, et al. Comparison between 68Ga-DOTA-NOC and 18F-DOPA PET for the detection of gastro-entero-pancreatic and lung neuro-endocrine tumours. Eur J Nucl Med Mol Imaging 2008;35(8):1431–8.
Ambrosini V, Castellucci P, Rubello D, Nanni C, Musto A, Allegri V, et al. 68Ga-DOTA-NOC: a new PET tracer for evaluating patients with bronchial carcinoid. Nucl Med Commun 2009;30(4):281–6.
Erasmus JJ, McAdams HP, Patz Jr EF, Coleman RE, Ahuja V, Goodman PC. Evaluation of primary pulmonary carcinoid tumors using FDG PET. AJR Am J Roentgenol 1998;170:1369–73.
Krüger S, Buck AK, Blumstein NM, Pauls S, Schelzig H, Kropf C, et al. Use of integrated FDG PET/CT imaging in pulmonary carcinoid tumours. J Intern Med 2006;260(6):545–50.
Daniels CE, Lowe VJ, Aubry MC, Allen MS, Jett JR. The utility of fluorodeoxyglucose emission tomography in the evaluation of carcinoid tumors presenting as pulmonary nodules. Chest 2007;131(1):255–60.
Binderup T, Knigge U, Loft A, Mortensen J, Pfeifer A, Federspiel B, et al. Functional imaging of neuroendocrine tumors: a head-to-head comparison of somatostatin receptor scintigraphy, 123I-MIBG scintigraphy, and 18F-FDG PET. J Nucl Med 2010;51(5):704–12.
Kayani I, Conry BG, Groves AM, Win T, Dickson J, Caplin M, et al. A comparison of 68Ga-DOTATATE and 18F-FDG PET/CT in pulmonary neuroendocrine tumors. J Nucl Med 2009;50(12):1927–32.
Jindal T, Kumar A, Venkitaraman B, Meena M, Kumar R, Malhotra A, et al. Evaluation of the role of [18F]FDG-PET/CT and [68Ga]DOTATOC-PET/CT in differentiating typical and atypical pulmonary carcinoids. Cancer Imaging 2011;11:70–5.
Williams ED, Sandler M. The classification of carcinoid tumours. Lancet 1963;i:238–9.
van der Harst E, de Herder WW, Bruining HA, Bonjer HJ, de Krijger RR, Lamberts SW, et al. [(123)I]metaiodobenzylguanidine and [(111)In]octreotide uptake in benign and malignant pheochromocytomas. J Clin Endocrinol Metab 2001;86:685–93.
Pacak K, Eisenhofer G, Carrasquillo JA, Chen CC, Li ST, Goldstein DS. 6-[18F]fluorodopamine positron emission tomographic (PET) scanning for diagnostic localization of pheochromocytoma. Hypertension 2001;38:6–8.
Franzius C, Hermann K, Weckesser M, Kopka K, Juergens KU, Vormoor J, et al. Whole-body PET/CT with 11C-meta-hydroxyephedrine in tumors of the sympathetic nervous system: feasibility study and comparison with 123I-MIBG SPECT/CT. J Nucl Med 2006;47(10):1635–42.
Yamamoto S, Hellman P, Wassberg C, Sundin A. 11C-Hydroxyephedrine positron emission tomography imaging of pheochromocytoma: a single center experience over 11 years. J Clin Endocrinol Metab 2012;97(7):2423–32.
Hoegerle S, Nitzsche E, Altehoefer C, Ghanem N, Manz T, Brink I, et al. Pheochromocytomas: detection with 18F DOPA whole body PET—initial results. Radiology 2002;222:507–12.
Imani F, Agopian VG, Auerbach MS, Walter MA, Imani F, Benz MR, et al. 18F-FDOPA PET and PET/CT accurately localize pheochromocytomas. J Nucl Med 2009;50:513–9.
Kauhanen S, Seppänen M, Ovaska J, Minn H, Bergman J, Korsoff P, et al. The clinical value of [18F]fluoro-dihydroxyphenylalanine positron emission tomography in primary diagnosis, staging, and restaging of neuroendocrine tumors. Endocr Relat Cancer 2009;16:255–65.
Hoegerle S, Ghanem N, Altehoefer C, Schipper J, Brink I, Moser E, et al. 18F-DOPA positron emission tomography for the detection of glomus tumours. Eur J Nucl Med Mol Imaging 2003;30:689–94.
Fiebrich HB, Brouwers AH, Kerstens MN, Pijl ME, Kema IP, de Jong JR, et al. 6-[F-18]Fluoro-L-dihydroxyphenylalanine positron emission tomography is superior to conventional imaging with (123)I-metaiodobenzylguanidine scintigraphy, computer tomography, and magnetic resonance imaging in localizing tumors causing catecholamine excess. J Clin Endocrinol Metab 2009;94(10):3922–30.
Taïeb D, Tessonnier L, Sebag F, Niccoli-Sire P, Morange I, Colavolpe C, et al. The role of 18F-FDOPA and 18F-FDG-PET in the management of malignant and multifocal phaeochromocytomas. Clin Endocrinol (Oxf) 2008;69(4):580–6.
Charrier N, Deveze A, Fakhry N, Sebag F, Morange I, Gaborit B, et al. Comparison of [111In]pentetreotide-SPECT and [18F]FDOPA-PET in the localization of extra-adrenal paragangliomas: the case for a patient-tailored use of nuclear imaging modalities. Clin Endocrinol (Oxf) 2011;74(1):21–9.
Fottner C, Helisch A, Anlauf M, Rossmann H, Musholt TJ, Kreft A, et al. 6-18F-fluoro-L-dihydroxyphenylalanine positron emission tomography is superior to 123I-metaiodobenzyl-guanidine scintigraphy in the detection of extraadrenal and hereditary pheochromocytomas and paragangliomas: correlation with vesicular monoamine transporter expression. J Clin Endocrinol Metab 2010;95(6):2800–10.
King KS, Chen CC, Alexopoulos DK, Whatley MA, Reynolds JC, Patronas N, et al. Functional imaging of SDHx-related head and neck paragangliomas: comparison of 18F-fluorodihydroxyphenylalanine, 18F-fluorodopamine, 18F-fluoro-2-deoxy-D-glucose PET, 123I-metaiodobenzylguanidine scintigraphy, and 111In-pentetreotide scintigraphy. J Clin Endocrinol Metab 2011;96(9):2779–85.
Rufini V, Treglia G, Castaldi P, Perotti G, Calcagni ML, Corsello SM, et al. Comparison of 123I-MIBG SPECT-CT and 18F-DOPA PET-CT in the evaluation of patients with known or suspected recurrent paraganglioma. Nucl Med Commun 2011;32:575–82.
Taïeb D, Timmers HJ, Hindié E, Guillet BA, Neumann HP, Walz MK, et al. EANM 2012 guidelines for radionuclide imaging of phaeochromocytoma and paraganglioma. Eur J Nucl Med Mol Imaging 2012;39(12):1977–95.
Treglia G, Cocciolillo F, de Waure C, Di Nardo F, Gualano MR, Castaldi P, et al. Diagnostic performance of 18F-dihydroxyphenylalanine positron emission tomography in patients with paraganglioma: a meta-analysis. Eur J Nucl Med Mol Imaging 2012;39(7):1144–53.
Timmers HJ, Chen CC, Carrasquillo JA, Whatley M, Ling A, Havekes B, et al. Comparison of 18F-fluoro-L-DOPA, 18F-fluoro-deoxyglucose, and 18F-fluorodopamine PET and 123I-MIBG scintigraphy in the localization of pheochromocytoma and paraganglioma. J Clin Endocrinol Metab 2009;94(12):4757–67.
Weisbrod AB, Kitano M, Gesuwan K, Millo C, Herscovitch P, Nilubol N, et al. Clinical utility of functional imaging with 18F-FDOPA in Von Hippel-Lindau syndrome. J Clin Endocrinol Metab 2012;97(4):E613–7.
Rischke HC, Benz MR, Wild D, Mix M, Dumont RA, Campbell D, et al. Correlation of the genotype of paragangliomas and pheochromocytomas with their metabolic phenotype on 3,4-dihydroxy-6-18F-fluoro-L-phenylalanin PET. J Nucl Med 2012;53:1352–8.
Reubi JC, Waser B, Khosla S, Kvols L, Goellner JR, Krenning E, et al. In vitro and in vivo detection of somatostatin receptors in pheochromocytomas and paragangliomas. J Clin Endocrinol Metab 1992;74:1082–9.
Maurice JB, Troke R, Win Z, Ramachandran R, Al-Nahhas A, Naji M, et al. A comparison of the performance of 68Ga-DOTATATE PET/CT and 123I-MIBG SPECT in the diagnosis and follow-up of phaeochromocytoma and paraganglioma. Eur J Nucl Med Mol Imaging 2012;39(8):1266–70.
Montravers F, Kerrou K, Huchet V, Nataf V, Talbot JN. Evaluation of the impact of FDOPA-PET on the management of patients referred for pheochromocytoma. J Nucl Med 2008;49(Suppl 1):365.
Ezziddin S, Logvinski T, Yong-Hing C, Ahmadzadehfar H, Fischer HP, Palmedo H, et al. Factors predicting tracer uptake in somatostatin receptor and MIBG scintigraphy of metastatic gastroenteropancreatic neuroendocrine tumors. J Nucl Med 2006;47:223–33.
Kaltsas G, Korbonits M, Heintz E, Mukherjee JJ, Jenkins PJ, Chew SL, et al. Comparison of somatostatin analog and meta-iodobenzylguanidine radionuclides in the diagnosis and localization of advanced neuroendocrine tumors. J Clin Endocrinol Metab 2001;86:895–902.
Hoegerle S, Schneider B, Kraft A, Moser E, Nitzsche EU. Imaging of a metastatic gastrointestinal carcinoid by F-18-DOPA positron emission tomography. Nuklearmedizin 1999;38(4):127–30.
Hoegerle S, Altehoefer C, Ghanem N, Koehler G, Waller CF, Scheruebl H, et al. Whole-body 18F dopa PET for detection of gastrointestinal carcinoid tumors. Radiology 2001;220:373–80.
Le Rest C, Bomanji JB, Costa DC, Townsend CE, Visvikis D, Ell PJ. Functional imaging of malignant paragangliomas and carcinoid tumours. Eur J Nucl Med 2001;28(4):478–82.
Belhocine T, Foidart J, Rigo P, Najjar F, Thiry A, Quatresooz P, et al. Fluorodeoxyglucose positron emission tomography and somatostatin receptor scintigraphy for diagnosing and staging carcinoid tumours: correlations with the pathological indexes p53 and Ki-67. Nucl Med Commun 2002;23:727–34.
Fiebrich HB, Brouwers AH, Koopmans KP, de Vries EG. Combining 6-fluoro-[18F]l-dihydroxyphenylalanine and [18F]fluoro-2-deoxy-d-glucose positron emission tomography for distinction of non-carcinoid malignancies in carcinoid patients. Eur J Cancer 2009;45(13):2312–5.
Amin S, Warner RR, Itzkowitz SH, Kim MK. The risk of metachronous cancers in patients with small-intestinal carcinoid tumors: a US population-based study. Endocr Relat Cancer 2012;19(3):381–7.
Fiebrich HB, de Jong JR, Kema IP, Koopmans KP, Sluiter W, Dierckx RA, et al. Total 18F-dopa PET tumour uptake reflects metabolic endocrine tumour activity in patients with a carcinoid tumour. Eur J Nucl Med Mol Imaging 2011;38(10):1854–61.
Haug A, Auernhammer CJ, Wängler B, Tiling R, Schmidt G, Göke B, et al. Intraindividual comparison of 68Ga-DOTA-TATE and 18F-DOPA PET in patients with well-differentiated metastatic neuroendocrine tumours. Eur J Nucl Med Mol Imaging 2009;36(5):765–70.
Montravers F, Nataf V, Balogova S, Calzada M, Maurel G, Kerrou K, et al. Comparison of FDOPA (18F) and DOTATOC (68Ga) PET/CT for detection of ileal carcinoid tumours. Eur J Nucl Med Mol Imaging 2010;37(S2):S302. abstract OP586.
Yakemchuk VN, Jager PL, Chirakal R, Reid R, Major P, Gulenchyn KY. PET/CT using 18F-FDOPA provides improved staging of carcinoid tumor patients in a Canadian setting. Nucl Med Commun 2012;33(3):322–30.
Dolcetta-Capuzzo A, Villa V, Albarello L, Franchi GM, Gemma M, Scavini M, et al. Gastroenteric neuroendocrine neoplasms classification: comparison of prognostic models. Cancer 2013;119(1):36–44.
Jones K, Subramaniam RM, Durnick DK, Peller PJ. F-18-FDG-PET/CT imaging of small cell carcinoma of the colon. Clin Nucl Med 2008;33(9):645–6.
Power DG, Asmis TR, Tang LH, Brown K, Kemeny NE. High-grade neuroendocrine carcinoma of the colon, long-term survival in advanced disease. Med Oncol 2011;28 Suppl 1:S169–74.
Ahlström H, Eriksson B, Bergström M, Bjurling P, Långström B, Oberg K. Pancreatic neuroendocrine tumors: diagnosis with PET. Radiology 1995;195:333–7.
Wild D, Christ E, Caplin ME, Kurzawinski TR, Forrer F, Brändle M, et al. Glucagon-like peptide-1 versus somatostatin receptor targeting reveals 2 distinct forms of malignant insulinomas. J Nucl Med 2011;52(7):1073–8.
Kauhanen S, Seppänen M, Minn H, Gullichsen R, Salonen A, Alanen K, et al. Fluorine-18-L-dihydroxyphenylalanine (18F-DOPA) positron emission tomography as a tool to localize an insulinoma or β-cell hyperplasia in adult patients. J Clin Endocrinol Metab 2007;92:1237–44.
Tessonnier L, Sebag F, Ghander C, De Micco C, Reynaud R, Palazzo FF, et al. Limited value of 18F-F-DOPA PET to localize pancreatic insulin-secreting tumors in adults with hyperinsulinemic hypoglycemia. J Clin Endocrinol Metab 2010;95(1):303–7.
Putzer D, Gabriel M, Kendler D, Henninger B, Knoflach M, Kroiss A, et al. Comparison of (68)Ga-DOTA-Tyr(3)-octreotide and (18)F-fluoro-L-dihydroxyphenylalanine positron emission tomography in neuroendocrine tumor patients. Q J Nucl Med Mol Imaging 2010;54(1):68–75.
Abgral R, Leboulleux S, Déandreis D, Aupérin A, Lumbroso J, Dromain C, et al. Performance of (18)fluorodeoxyglucose-positron emission tomography and somatostatin receptor scintigraphy for high Ki67 (≥10 %) well-differentiated endocrine carcinoma staging. J Clin Endocrinol Metab 2011;96(3):665–71.
Ribeiro MJ, Boddaert N, Bellanné-Chantelot C, Bourgeois S, Valayannopoulos V, Delzescaux T, et al. The added value of [18F]fluoro-L-DOPA PET in the diagnosis of hyperinsulinism of infancy: a retrospective study involving 49 children. Eur J Nucl Med Mol Imaging 2007;34(12):2120–8.
Otonkoski T, Näntö-Salonen K, Seppänen M, Veijola R, Huopio H, Hussain K, et al. Noninvasive diagnosis of focal hyperinsulinism of infancy with [18F]-DOPA positron emission tomography. Diabetes 2006;55:13–8.
Hardy OT, Hernandez-Pampaloni M, Saffer JR, Sheuermann JS, Ernst LM, Freifelder R, et al. Accuracy of [18F]fluorodopa positron emission tomography for diagnosing and localizing focal congenital hyperinsulinism. J Clin Endocrinol Metab 2007;92:4706–11.
Capito C, Khen-Dunlop N, Ribeiro MJ, Brunelle F, Aigrain Y, Crétolle C, et al. Value of 18F-fluoro-L-dopa PET in the preoperative localization of focal lesions in congenital hyperinsulinism. Radiology 2009;253:216–22.
Zani A, Nah SA, Ron O, Totonelli G, Ismail D, Smith VV, et al. The predictive value of preoperative fluorine-18-L-3,4-dihydroxyphenylalanine positron emission tomography-computed tomography scans in children with congenital hyperinsulinism of infancy. J Pediatr Surg 2011;46(1):204–8.
Mohnike W, Barthlen W, Mohnike K, Blankenstein O. Positron emission tomography/computed tomography diagnostics by means of fluorine-18-L-dihydroxyphenylalanine in congenital hyperinsulinism. Semin Pediatr Surg 2011;20(1):23–7.
Treglia G, Mirk P, Giordano A, Rufini V. Diagnostic performance of fluorine-18-dihydroxyphenylalanine positron emission tomography in diagnosing and localizing the focal form of congenital hyperinsulinism: a meta-analysis. Pediatr Radiol 2012;42(11):1372–9.
Blomberg BA, Moghbel MC, Saboury B, Stanley CA, Alavi A. The value of radiologic interventions and (18)F-DOPA PET in diagnosing and localizing focal congenital hyperinsulinism: systematic review and meta-analysis. Mol Imaging Biol 2013;15:97–105.
Iagaru A, Gamie S, Segall G. F-18 FDG PET imaging of urinary bladder oat cell carcinoma with widespread osseous metastases. Clin Nucl Med 2006;31(8):476–8.
Fujishita T, Kishida M, Taki H, Shinoda C, Miyabayashi K, Fujishita M, et al. Detection of primary and metastatic lesions by [18F]fluoro-2-deoxy-D-glucose PET in a patient with thymic carcinoid. Respirology 2007;12(6):928–30.
Kobashi Y, Shimizu H, Mouri K, Irei T, Oka M. Clinical usefulness of fluoro-2-deoxy-D-glucose PET in a case with multiple bone metastases of carcinoid tumor after ten years. Intern Med 2009;48(21):1919–23.
Dutta R, Kumar A, Julka PK, Mathur SR, Kaushal S, Kumar R, et al. Thymic neuroendocrine tumour (carcinoid): clinicopathological features of four patients with different presentation. Interact Cardiovasc Thorac Surg 2010;11(6):732–6.
Spieth ME, Lin YG, Nguyen TT. Diagnosing and treating small-cell carcinomas of prostatic origin. Clin Nucl Med 2002;27(1):11–7.
Anker CJ, Dechet C, Isaac JC, Akerley W, Shrieve DC. Small-cell carcinoma of the prostate. J Clin Oncol 2008;26:1168–71.
Yilmaz M, Celen Z, Sevinc A, Karakok M. Widespread metastases in small cell carcinoma of the prostate on FDG PET/CT. Clin Nucl Med 2009;34:598–600.
de Carvalho Flamini R, Yamaga L, Mello ME, Wagner J, Livorsi Da Cunha M, Osawa A, et al. F-18 FDG PET/CT imaging in small cell prostate cancer. Clin Nucl Med 2010;35:452–3.
Brammer JE, Lulla P, Lynch GR. Complete remission in a patient with metastatic mixed adenocarcinoma/extrapulmonary small cell carcinoma of the prostate. Int J Clin Oncol 2011;16(6):722–5.
Miljković MD, Girotra M, Abraham RR, Erlich RB. Novel medical therapies of recurrent and metastatic gastroenteropancreatic neuroendocrine tumors. Dig Dis Sci 2012;57(1):9–18.
Garin E, Le Jeune F, Devillers A, Cuggia M, de Lajarte-Thirouard AS, Bouriel C, et al. Predictive value of 18F-FDG PET and somatostatin receptor scintigraphy in patients with metastatic endocrine tumors. J Nucl Med 2009;50(6):858–64.
Schmitt AM, Riniker F, Anlauf M, Schmid S, Soltermann A, Moch H, et al. Islet 1 (Isl1) expression is a reliable marker for pancreatic endocrine tumors and their metastases. Am J Surg Pathol 2008;32(3):420–5.
Chan ES, Alexander J, Swanson PE, Jain D, Yeh MM. PDX-1, CDX-2, TTF-1, and CK7: a reliable immunohistochemical panel for pancreatic neuroendocrine neoplasms. Am J Surg Pathol 2012;36(5):737–43.
Frilling A, Sotiropoulos GC, Radtke A, Malago M, Bockisch A, Kuehl H, et al. The impact of 68Ga-DOTATOC positron emission tomography/computed tomography on the multimodal management of patients with neuroendocrine tumors. Ann Surg 2010;252(5):850–6.
Prasad V, Ambrosini V, Hommann M, Hoersch D, Fanti S, Baum RP. Detection of unknown primary neuroendocrine tumours (CUP-NET) using (68)Ga-DOTA-NOC receptor PET/CT. Eur J Nucl Med Mol Imaging 2010;37(1):67–77.
Naswa N, Sharma P, Kumar A, Soundararajan R, Kumar R, Malhotra A, et al. 68Ga-DOTANOC PET/CT in patients with carcinoma of unknown primary of neuroendocrine origin. Clin Nucl Med 2012;37(3):245–51.
Perakakis N, Laubner K, Keck T, Steffl D, Lausch M, Meyer PT, et al. Ectopic ACTH-syndrome due to a neuroendocrine tumour of the appendix. Exp Clin Endocrinol Diabetes 2011;119(9):525–9.
Schalin-Jäntti C, Ahonen A, Seppänen M. 18F-DOPA PET/CT but not 68Ga-DOTA-TOC PET/CT revealed the underlying cause of ectopic Cushing syndrome. Clin Nucl Med 2012;37(9):904–5.
Markou A, Manning P, Kaya B, Datta SN, Bomanji JB, Conway GS. [18F]fluoro-2-deoxy-D-glucose ([18F]FDG) positron emission tomography imaging of thymic carcinoid tumor presenting with recurrent Cushing’s syndrome. Eur J Endocrinol 2005;152(4):521–5.
Gomard-Mennesson E, Sève P, De La Roche E, Collardeau-Frachon S, Lombard-Bohas C, Broussolle C. Thymic carcinoid tumor revealed by a Cushings’ syndrome: usefulness of positron emission tomography. Rev Med Interne 2008;29(9):751–3.
Shah NA, Urusova IA, D’Agnolo A, Colquhoun SD, Rosenbloom BE, Vener SL, et al. Primary hepatic carcinoid tumor presenting as Cushing’s syndrome. J Endocrinol Invest 2007;30(4):327–33.
Nikolaou A, Thomas D, Kampanellou C, Alexandraki K, Andersson LG, Sundin A, et al. The value of 11C-5-hydroxy-tryptophan positron emission tomography in neuroendocrine tumor diagnosis and management: experience from one center. J Endocrinol Invest 2010;33(11):794–9.
Singer J, Werner F, Koch CA, Bartels M, Aigner T, Lincke T, et al. Ectopic Cushing’s syndrome caused by a well differentiated ACTH-secreting neuroendocrine carcinoma of the ileum. Exp Clin Endocrinol Diabetes 2010;118(8):524–9.
Willhauck MJ, Pöpperl G, Rachinger W, Giese A, Auernhammer CJ, Spitzweg C. An unusual case of ectopic ACTH syndrome. Exp Clin Endocrinol Diabetes 2012;120(2):63–7.
Zemskova MS, Gundabolu B, Sinaii N, Chen CC, Carrasquillo JA, Whatley M, et al. Utility of various functional and anatomic imaging modalities for detection of ectopic adrenocorticotropin-secreting tumors. J Clin Endocrinol Metab 2010;95(3):1207–19.
Lange-Nolde A, Zajic T, Slawik M, Brink I, Reincke M, Moser E, et al. PET with 18F-DOPA in the imaging of parathyroid adenoma in patients with primary hyperparathyroidism. A pilot study. Nuklearmedizin 2006;45(5):193–6.
Froeling V, Elgeti F, Maurer MH, Scheurig-Muenkler C, Beck A, Kroencke TJ, et al. Impact of Ga-68 DOTATOC PET/CT on the diagnosis and treatment of patients with multiple endocrine neoplasia. Ann Nucl Med 2012;26(9):738–43.
Gourgiotis L, Sarlis NJ, Reynolds JC, VanWaes C, Merino MJ, Pacak K. Localization of medullary thyroid carcinoma metastasis in a multiple endocrine neoplasia type 2A patient by 6-[18F]-fluorodopamine positron emission tomography. J Clin Endocrinol Metab 2003;88(2):637–41.
Boér A, Szakáll Jr S, Klein I, Kásler M, Vincze B, Trón L, et al. FDG PET imaging in hereditary thyroid cancer. Eur J Surg Oncol 2003;29(10):922–8.
Skoura E, Rondogianni P, Alevizaki M, Tzanela M, Tsagarakis S, Piaditis G, et al. Role of [(18)F]FDG-PET/CT in the detection of occult recurrent medullary thyroid cancer. Nucl Med Commun 2010;31(6):567–75.
Schiesser M, Veit-Haibach P, Muller MK, Weber M, Bauerfeind P, Hany T, et al. Value of combined 6-[18F]fluorodihydroxyphenylalanine PET/CT for imaging of neuroendocrine tumours. Br J Surg 2010;97(5):691–7.
Gabriel M, Decristoforo C, Kendler D, Dobrozemsky G, Heute D, Uprimny C, et al. 68Ga-DOTA-Tyr3-octreotide PET in neuroendocrine tumors: comparison with somatostatin receptor scintigraphy and CT. J Nucl Med 2007;48(4):508–18.
Haug AR, Cindea-Drimus R, Auernhammer CJ, Reincke M, Wängler B, Uebleis C, et al. The role of 68Ga-DOTATATE PET/CT in suspected neuroendocrine tumors. J Nucl Med 2012;53(11):1686–92.
Sanduleanu S, Stridsberg M, Jonkers D, Hameeteman W, Biemond I, Lundqvist G, et al. Serum gastrin and chromogranin A during medium- and long-term acid suppressive therapy: a case–control study. Aliment Pharmacol Ther 1999;13(2):145–53.
Mosli HH, Dennis A, Kocha W, Asher LJ, Van Uum SH. Effect of short-term proton pump inhibitor treatment and its discontinuation on chromogranin A in healthy subjects. J Clin Endocrinol Metab 2012;97(9):E1731–5.
Raines D, Chester M, Diebold AE, Mamikunian P, Anthony CT, Mamikunian G, et al. A prospective evaluation of the effect of chronic proton pump inhibitor use on plasma biomarker levels in humans. Pancreas 2012;41(4):508–11.
Mercer DW, Virji MA, Barry GE, Piper ML. New solid-phase enzyme immunoassay of neuron-specific enolase in serum: effect of storage temperature, lipemia, icterus, and hemolysis. Clin Chem 1990;36(8 Pt 1):1519.
Acknowledgment
The authors acknowledge the motivation of the team of the Nuclear Medicine Department of Hôpital Tenon for performing FDOPA and 68Ga-DOTATOC PET/CT. They thank Dr. A. Haug for his kind interactivity in commenting on his results. Most of our experience in NET PET has been developed thanks to Clinical Research Projects (PHRC) grants of the French Ministry of Health, Assitance Publique-Hôpitaux de Paris (AP-HP) acting as the sponsor: PHRC 2006 AOM 06176 & P040303 EUDRACT 2007-002610-19. The authors thank Mrs. Z. Idir who was the project manager for those research activities on PET/CT in NET at the Direction de la Recherche Clinique AP-HP and proved to be very effective and committed.
Conflicts of interests
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Balogova, S., Talbot, JN., Nataf, V. et al. 18F-Fluorodihydroxyphenylalanine vs other radiopharmaceuticals for imaging neuroendocrine tumours according to their type. Eur J Nucl Med Mol Imaging 40, 943–966 (2013). https://doi.org/10.1007/s00259-013-2342-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-013-2342-x