Abstract
Purpose
Pathological data suggest that the rate of oestrogen receptor (ER) expression in uterine sarcoma is significantly lower than in leiomyoma. The present study aimed to investigate whether ER expression using ER imaging agents for positron emission tomography (PET), of which the most successful has been 16α-[18F]-fluoro-17β-oestradiol (FES), is able to add useful information to the differential diagnosis of uterine sarcoma and leiomyoma in patients with positive or equivocal findings on [18F]fluorodeoxyglucose (FDG) PET.
Methods
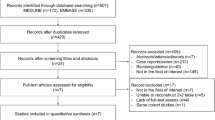
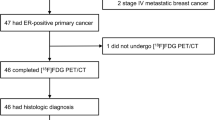
A total of 76 patients with suspected uterine sarcoma based on ultrasound and magnetic resonance imaging findings from 2007 to 2010 were enrolled. Twenty-four of the present patients were referred for FES PET because of FDG PET findings that showed equivocal or positive FDG uptake. PET images were quantitatively evaluated with reference to histopathological findings. Receiver-operating characteristic analysis was performed to determine the optimal cutoff value to differentiate uterine sarcoma and leiomyoma.
Results
Of the 24 patients, 11 had a final diagnosis of uterine sarcoma, while 13 had leiomyoma. The sensitivity, specificity and accuracy of an FDG to FES standardized uptake value (SUV) ratio greater than 2.0 were significantly higher using Cochran’s Q test (p = 0.024) when compared with FDG PET greater than 3.0 alone (90.9 vs 81.8%, 92.3 vs 84.6% and 91.3 vs 83.3%, respectively).
Conclusion
Additional FES PET findings confirmed uterine sarcoma in 91.3% of a selected group of patients with equivocal or positive FDG uptake.


Similar content being viewed by others
References
Adams Hillard PJ. Benign disease of the female reproductive tract. In: Berek JS, editor. Berek & Novak’s gynecology. 14th ed. Philadelphia: Lippincott Williams & Wilkins; 2006. p. 431–504.
Sutton GP, Stehman FB, Michael H, Young PC, Ehrlich CE. Estrogen and progesterone receptors in uterine sarcomas. Obstet Gynecol 1986;68:709–14.
Amant F, Coosemans A, Debiec-Rychter M, Timmerman D, Vergote I. Clinical management of uterine sarcomas. Lancet Oncol 2009;10:1188–98.
Milman D, Zalel Y, Biran H, Open M, Caspi B, Hagay Z, et al. Unsuspected uterine leiomyosarcoma discovered during treatment with a gonadotropin-releasing hormone analogue: a case report and literature review. Eur J Obstet Gynecol Reprod Biol 1998;76:237–40.
Wallach EE, Vlahos NF. Uterine myomas: an overview of development, clinical features, and management. Obstet Gynecol 2004;104:393–406.
Parker WH. Uterine myomas: management. Fertil Steril 2007;88:255–71.
Schwartz LB, Zawin M, Carcangiu ML, Lange R, McCarthy S. Does pelvic magnetic resonance imaging differentiate among the histologic subtypes of uterine leiomyomata? Fertil Steril 1998;70:580–7.
Sahdev A, Sohaib SA, Jacobs I, Shepherd JH, Oram DH, Reznek RH. MR imaging of uterine sarcomas. AJR Am J Roentgenol 2001;177:1307–11.
Kido A, Togashi K, Koyama T, Yamaoka T, Fujiwara T, Fujii S. Diffusely enlarged uterus: evaluation with MR imaging. Radiographics 2003;23:1423–39.
Tanaka YO, Nishida M, Tsunoda H, Okamoto Y, Yoshikawa H. Smooth muscle tumors of uncertain malignant potential and leiomyosarcomas of the uterus: MR findings. J Magn Reson Imaging 2004;20:998–1007.
Rohren EM, Turkington TG, Coleman RE. Clinical applications of PET in oncology. Radiology 2004;231:305–32.
Yoshida Y, Kurokawa T, Sawamura Y, Shinagawa A, Tsujikawa T, Okazawa H, et al. Comparison of 18F-FDG PET and MRI in assessment of uterine smooth muscle tumors. J Nucl Med 2008;49:708–12.
Kitajima K, Murakami K, Kaji Y, Sugimura K. Spectrum of FDG PET/CT findings of uterine tumors. AJR Am J Roentgenol 2010;195:737–43.
Tsujikawa T, Yoshida Y, Mori T, Kurokawa T, Fujibayashi Y, Kotsuji F, et al. Uterine tumors: pathophysiologic imaging with 16alpha-[18F]fluoro-17beta-estradiol and 18F fluorodeoxyglucose PET–initial experience. Radiology 2008;248:599–605.
Mori T, Kasamatsu S, Mosdzianowski C, Welch MJ, Yonekura Y, Fujibayashi Y. Automatic synthesis of 16 alpha-[(18)F]fluoro-17beta-estradiol using a cassette-type [(18)F]fluorodeoxyglucose synthesizer. Nucl Med Biol 2006;33:281–6.
Tsujikawa T, Yoshida Y, Kudo T, Kiyono Y, Kurokawa T, Kobayashi M, et al. Functional images reflect aggressiveness of endometrial cancer: estrogen receptor expression combined with 18FDG PET. J Nucl Med 2009;50:1598–604.
Gompel C, Silverberg SG. Pathology in gynecology and obstetrics. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 1994. p. 163–283.
Bodner K, Bodner-Adler B, Kimberger O, Czerwenka K, Leodolter S, Mayerhofer K. Estrogen and progesterone receptor expression in patients with uterine leiomyosarcoma and correlation with different clinicopathological parameters. Anticancer Res 2003;23:729–32.
Leitao MM, Soslow RA, Nonaka D, Olshen AB, Aghajanian C, Sabbatini P, et al. Tissue microarray immunohistochemical expression of estrogen, progesterone, and androgen receptors in uterine leiomyomata and leiomyosarcoma. Cancer 2004;101:1455–62.
Zhai YL, Kobayashi Y, Mori A, Orii A, Nikaido T, Konishi I, et al. Expression of steroid receptors, Ki-67, and p53 in uterine leiomyosarcomas. Int J Gynecol Pathol 1999;18:20–8.
Mittal K, Demopoulos RI. MIB-1 (Ki-67), p53, estrogen receptor, and progesterone receptor expression in uterine smooth muscle tumors. Hum Pathol 2001;32:984–7.
Ioffe YJ, Li AJ, Walsh CS, Karlan BY, Leuchter R, Forscher C, et al. Hormone receptor expression in uterine sarcomas: prognostic and therapeutic roles. Gynecol Oncol 2009;115:466–71.
Uchida T, Nakakawaji K, Sakamoto J, Kojima H, Murakami H, Kato J, et al. The effectiveness of medroxyprogesterone in the treatment of multiple metastasizing leiomyosarcomas: report of a case. Surg Today 1996;26:138–41.
Tsujikawa T, Yoshida Y, Kiyono Y, Kurokawa T, Kudo T, Fujibayashi Y, et al. Functional oestrogen receptor alpha imaging in endometrial carcinoma using 16alpha-[(18)F]fluoro-17beta-oestradiol PET. Eur J Nucl Med Mol Imaging 2011;38(1):37–45.
Conneely OM, Lydon JP, De Mayo F, O’Malley BW. Reproductive functions of the progesterone receptor. J Soc Gynecol Investig 2000;7:S25–32.
Zhu XQ, Shi YF, Cheng XD, Zhao CL, Wu YZ. Immunohistochemical markers in differential diagnosis of endometrial stromal sarcoma and cellular leiomyoma. Gynecol Oncol 2004;92:71–9.
Kir G, Cetiner H, Karateke A, Gurbuz A, Bulbul D. Utility of MIB-1 and estrogen and progesterone receptor in distinguishing between endometrial stromal sarcomas and endometrial stromal nodules, highly cellular leiomyomas. Int J Gynecol Cancer 2005;15:337–42.
Policarpio-Nicolas ML, Cathro HP, Kerr SE, Stelow EB. Cytomorphologic features of low-grade endometrial stromal sarcoma. Am J Clin Pathol 2007;128:265–71.
Gregory S, John K, Aaron W, Carmen T. Corpus: mesenchymal tumors. In: Barakat RR, editor. Principles and practice of gynecologic oncology. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2009. p. 733–61.
Oda K, Okada S, Nei T, Shirai T, Takahashi M, Sano Y, et al. Cytodiagnostic problems in uterine sarcoma. Analysis according to a novel classification of tumor growth types. Acta Cytol 2004;48:181–6.
Tsuchida T, Okazawa H, Mori T, Kobayashi M, Yoshida Y, Fujibayashi Y, et al. In vivo imaging of estrogen receptor concentration in the endometrium and myometrium using FES PET—influence of menstrual cycle and endogenous estrogen level. Nucl Med Biol 2007;34:205–10.
Acknowledgments
This study was partly funded by the Research and Development Project Aimed at Economic Revitalization (Leading Project) from MEXT Japan, Grants-in-Aid for Scientific Research (Nos. 20790887 and 21390342) and the 21st Century Center of Excellence Program from the Japan Society for the Promotion of Science.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoshida, Y., Kiyono, Y., Tsujikawa, T. et al. Additional value of 16α-[18F]fluoro-17β-oestradiol PET for differential diagnosis between uterine sarcoma and leiomyoma in patients with positive or equivocal findings on [18F]fluorodeoxyglucose PET. Eur J Nucl Med Mol Imaging 38, 1824–1831 (2011). https://doi.org/10.1007/s00259-011-1851-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-011-1851-8