Abstract
Involvement of the cervical lymph nodes is the most important prognostic factor for patients with oral/oropharyngeal squamous cell carcinoma (OSCC), and the decision whether to electively treat patients with clinically negative necks remains a controversial topic. Sentinel node biopsy (SNB) provides a minimally invasive method of determining the disease status of the cervical node basin, without the need for a formal neck dissection. This technique potentially improves the accuracy of histological nodal staging and avoids over-treating three-quarters of this patient population, minimizing associated morbidity. The technique has been validated for patients with OSCC, and larger-scale studies are in progress to determine its exact role in the management of this patient population. This article was designed to outline the current best practice guidelines for the provision of SNB in patients with early-stage OSCC, and to provide a framework for the currently evolving recommendations for its use. These guidelines were prepared by a multidisciplinary surgical/nuclear medicine/pathology expert panel under the joint auspices of the European Association of Nuclear Medicine (EANM) Oncology Committee and the Sentinel European Node Trial Committee.
Similar content being viewed by others
Introduction
Oral/oropharyngeal squamous cell cancer (OSCC) is one of the most common cancers worldwide, accounting for more than 274,000 new cases annually [1]. Three-quarters of affected people are in the developing world, while in developed countries, OSCC is the eighth most prevalent form of cancer. Determining the presence or absence of nodal metastasis is of paramount importance for staging, treatment planning and prognosis. The incidence of occult metastases in patients with clinically node-negative OSCC is high, with many series reporting rates greater than 30% [2–5]. Cervical lymph node involvement is the most important prognostic factor for patients with OSCC [5–7].
Elective treatment of the clinically-negative neck remains a controversial topic. Over the last two decades much work has been undertaken to find reliable predictors of occult metastases, of which tumour depth appears to be the best available [8–11]. However, the predictive capacity of tumour depth and other primary tumour characteristics is still insufficient to negate the need for surgical staging of the cervical node basin [12, 13].
Elective neck dissection (END) is the current gold-standard staging procedure for the clinically node-negative neck, providing valuable prognostic information regarding nodal status and simultaneously treating those patients found to be pathologiaclly node-positive. Previously, ENDs invariably took the form of a modified radical neck dissection; however, there is increasing evidence that selective neck dissection is as efficacious as comprehensive neck dissection in treating the negative neck [2, 14–20]. The shift toward more conservative surgical procedures has occurred primarily in the last two decades, facilitated by the work undertaken by Lindberg [21], Byers et al. [22] and Shah et al. [3] to describe the common patterns of lymphatic drainage. Knowledge of these patterns has allowed the extent of neck dissections to be progressively limited to those nodal levels at highest risk, and sentinel node biopsy (SNB) represents an extension of this philosophy.
The aim of this review is to provide evidence-based guidelines for the use of SNB as a staging tool in patients with early OSCC, presenting the best available evidence at the time of writing. The existing literature was reviewed, utilizing electronic techniques (Medline, Best evidence, the Cochrane Library, Dare) and hand searching techniques. Where little or no data existed from randomized controlled prospective trials, emphasis was given to data from large series or reports from recognized experts in the field. It is recognized that higher-level evidence from future studies may modify the recommendations made in these guidelines.
Definition of a sentinel node
The sentinel node concept states that the spread of a tumour is embolic in nature, via the lymphatics to the first echelon lymph node(s) encountered in the regional draining basin. These represent the lymph nodes most likely to harbour occult metastases, and are designated the sentinel lymph nodes (SLN). Excisional biopsy and pathological evaluation of the SLNs therefore allows prediction of the disease status of the remaining cervical lymph node basin, potentially avoiding the need for a neck dissection. SLNs need not be those closest to the tumour, and there may be multiple SLNs [23]. With the application of early dynamic lymphoscintigraphy (LSG), lymphatic channels are usually visualized and nodes on a direct drainage pathway may be distinguished. The practical approach may include a combination of available detection techniques.
Lymphatic mapping and SNB were first reported in 1977 by Cabanas for penile cancer [24]. In 1992, Morton et al. [23] were the first to describe the use of intradermal isosulphan blue dye injection for lymphatic mapping and SLN localization in patients with malignant melanoma. The following year, Alex et al. [25] described a peritumoral intradermal injection of radioactive tracer (99mTc sulphur colloid), followed by imaging and intraoperative gamma probe radiolocalization of SLNs. The sentinel node concept has since been extensively studied and validated for patients with cutaneous melanoma [26] and breast cancer [27], and studies to date have indicated a high level of accuracy in patients with OSCC [28, 29].
Clinical indications
Inclusion criteria
The most important inclusion criterion for SNB is a clinically negative neck, as defined by physical examination and clinical imaging by CT, contrast-enhanced MRI, ultrasound-guided fine-needle aspiration cytology and/or 18F-fluorodeoxyglucose PET with or without low-dose CT [30, 31]. There remains considerable debate as to the preferred imaging modality, and to date none has the ability to detect small or micrometastatic tumour deposits, but all techniques improve on the sensitivity of palpation alone, and are therefore recommended prior to SNB. Recently, the high specificity of PET has been highlighted as an important means of avoiding unnecessary neck dissections [30]. Gross lymphatic involvement can lead to distortion of the normal architecture, leading to aberrant drainage patterns and biopsy of false SLNs [32]. SNB is therefore contraindicated to stage clinically positive necks.
Following the first report of SNB for OSCC [33], the technique has undergone extensive validation against the gold-standard END, for tumours located in the oral cavity and accessible subsites of the oropharynx [29, 34]. It has been demonstrated to be an accurate means of staging the clinically negative neck, and more recently the potential prognostic value of SNB for these tumour sites has also been highlighted [35]. While SNB has been successfully reported for tumours in other locations such as the hypopharynx and supraglottic larynx [36], there remain significant technical barriers, and SNB for these sites should therefore still be considered investigational. Poor access to these sites requires general anaesthesia and endoscopic guidance for radiotracer injection, precluding the use of preoperative LSG, while the close proximity of the primary tumour to the first-echelon lymph nodes can potentially obscure the true location of SLNs. Additionally, advanced stage at presentation is common for these hidden tumours, precluding the use of SNB or indeed any surgical intervention.
There is an existing consensus that SNB for OSCC should be restricted to early tumours staged T1/2 [37–39]. Larger tumours are difficult to completely surround with the tracer injection, tend to drain to multiple lymphatic basins, and in most patients require a neck dissection for access to the primary tumour or defect reconstruction. Inclusion of T3/4 tumours in study protocols can lead to variability in the accuracy of the technique [37].
The first and most frequent indication for SNB is to stage the ipsilateral clinically node-negative neck in patients with a unilateral primary tumour. A second indication is for assessment of bilateral clinically node-negative necks in primary tumours close to, or crossing, the midline. The third indication is for assessment of the contralateral clinically node-negative neck in primary tumours close to the midline with an ipsilateral clinically node-positive neck, in order to decide whether these patients need bilateral neck dissections, or an ipsilateral neck dissection and contralateral SNB only. Patients should also be fit enough preoperatively to withstand a neck dissection.
Patients who have received prior radiation or surgical treatment to the neck are routinely excluded from SNB protocols, since the previous intervention can distort the normal lymphatic pathways and give rise to unexpected patterns of metastasis. It is possible that lymphatic mapping and SNB may yield potentially useful information in these patients. Similarly, patients with small recurrent or second primary tumours may also benefit from lymphatic mapping to guide surgical intervention. However, these applications of the SNB technique, whilst clinically attractive, remain largely unexplored.
Exclusion criteria
In pregnant women, the urgency and the necessity for staging the neck should be discussed. LSG is specifically contraindicated in the pelvis of pregnant women, but no such recommendations are currently available for the head and neck. As discussed in the section “Dosimetry – patient”, the risk of fetal damage is negligible during routine SNB procedures. However, SNB protocols should be modified in pregnant patients to minimize the risks of radiation exposure and blue-dye injections. For example, the use of a 1-day protocol allows a lower injected radiation dose, and the additional radiation associated with SPECT-CT imaging may not be warranted in the pregnant patient. SNB can be performed in lactating women, but it is advised that breastfeeding be discontinued following the procedure. OSCC is rare in children, though each case should be treated individually. In the UK, Nanocolloid is approved for use in children, though licensing varies between countries. The potential benefits of SNB are not as well delineated in the paediatric population and, in practice, most SNB trial protocols generally exclude these patients from participation. Off-label use of radiopharmaceuticals should be considered with caution and respect to an individual risk-benefit analysis. Other relative contraindications include a known allergy to albumin colloid, and primary tumour treatment by external beam radiotherapy.
In summary, SNB is currently indicated for cT1/2, clinically node-negative oral and selected oropharyngeal SCC, where it may be considered a valid alternative to END. Other head and neck sites, histologies and clinical situations remain under investigation.
Radiopharmaceuticals
Introduction
A variety of colloidal and soluble tracers have been used over the years for lymph studies. It is believed that radiocolloids are taken up by macrophages in lymph nodes whereas the transit of macromolecules through lymph nodes is delayed simply because of their large molecular size [40].
Choice of radiopharmaceutical
The main radiopharmaceutical used in European studies of SLN localization in oral cancers is 99mTc-labelled human serum albumin colloid (Nanocoll, GE Healthcare). Nanocoll has a particle size range of 5–80 nm, with a reported mean size of 8–30 nm [40]. Although in theory a larger particle such as Albures (GE Healthcare) or Sentiscint (Medi-Radiopharma) may be preferred for tumours in the floor of the mouth or anterior tongue where the lymphatic densities are high [37], Nanocoll performs satisfactorily in all tumour types studied. Nanocoll migrates to the SLN within minutes, yet prolonged retention allows surgery to take place the following day.
Other radiocolloids which have been used include 99mTc-rhenium sulphide colloid (Nanocis, IBA), which has been shown to have a mean particle size of 23–25 nm [41], and 99mTc-sulphide colloid. Standard preparations of 99mTc-sulphide colloid result in a wide range of particle sizes, so the product is often filtered through a 100- or 200-nm membrane filter to obtain a smaller and more uniform size distribution. While there are currently no clinical studies comparing different radiopharmaceuticals, investigators have described satisfactory results with each of the available colloids [42, 43].
Preparation and quality control
Nanocoll is labelled by incubation with 99mTc-pertechnetate at room temperature for 30 min [44]. Radiochemical purity can be checked by thin layer chromatography and the labelling efficiency should be >95%. The EANM guidelines on current good radiopharmacy practice (cGRPP, www.eanm.org) recommend that the labelling efficiency be checked on each preparation. The stated expiry is 6 h after preparation, although extended stability has been demonstrated [45].
Drug interactions and adverse effects
No interactions of drugs with radiocolloids are expected following local intradermal or subcutaneous administration. Adverse effects are rare and mild following interstitial administration of radiocolloids, although allergic reactions have been reported with Nanocoll [46, 47] and the blue dyes used at surgery [48]. The incidence of allergic reactions is too low to quantify, but appropriate emergency medicines should be kept available during the procedure.
Summary
99mTc-labelled Nanocoll is easy to prepare and supply, and has suitable properties for SLN localization in oral cancers, with rapid migration to the SLN and prolonged retention.
Dosimetry – patient
General remarks
Presently available dosimetric data are derived from the breast cancer SNB literature, where the absorbed doses to patients are determined to be low; therefore, the radiation risk associated with this procedure is low. While no specific OSCC data exist, the radiopharmaceuticals and administered activity are identical, leading to the assumption that OSCC SNB is a safe procedure from the radiation protection point of view.
Patient exposure
The estimated local radiation dose varies greatly, depending on the administered dose and time to surgery. As mentioned in the section “Injection”, there is little consensus on the optimal administered dose and timing of surgery relative to the radiocolloid injection. Most centres perform LSG within 24 h of surgery, but recommendations for administered activity range from 15 MBq (for a same-day procedure) to 120 MBq (for a 2-day procedure) in a total injection volume of 0.4–1.0 ml. The aim is to achieve an activity of at least 10 MBq at the time of surgery [49, 50]. Current EANM guidelines for SNB in breast cancer recommend a mean value for the effective dose of 0.048 mSv [51]. While other authors have reported doses approximately tenfold higher [52], these remain low compared with other nuclear medicine procedures. Extensive calculations performed at the Memorial Sloan Kettering Cancer Center have confirmed the safety of SNB by reporting an effective dose around 0.2 mSv [53].
Fetal exposure
The maximum value for fetal absorbed dose has been calculated to be 0.013 mSv following injection of 18.5 MBq [53]. This dose is equivalent to that received by the mother from 1 day of natural background radiation in the USA [52], and is orders of magnitude below the 100–200 mSv threshold for deterministic effects (malformation, growth retardation, neurodevelopmental abnormalities) [54]. Current consensus is that noncancer health effects are not detectable below 50 mSv [53], while congenital malformations occur above 200 mSv. With respect to childhood cancer induction (stochastic effect), ICRP (International Commission on Radiological Protection) reports a threshold of 10 mSv for a 40% risk increase [54].
In summary, the advantages of SNB for OSCC outweigh the potential risks of the absorbed radiation dose, and this is also true for pregnant patients. While SNB is not contraindicated in pregnant patients, it is preferable to use a same-day protocol, enabling a lower injected dose [50].
Lactating women
The current recommendation is that nursing mothers should suspend breast-feeding for 24 h following radiopharmaceutical injection, during which time the general anaesthetic agent and radiocolloid will be excreted in the breast milk [51].
Dosimetry – staff
Staff in operating room
Studies in breast and melanoma patients have determined the mean whole-body dose received by surgical staff to be <1µSv per operation [52, 55–57], with a maximum dose to the surgeon of <2µSv. The absorbed doses are further minimized when SNB is performed at 24 h after injection [58]. Monitoring of operating room personnel for occupational exposure during the procedure is therefore unnecessary, and additional shielding is not required. While the pregnant surgeon or scrub nurse requires specific consideration, radiation exposure from participation in fewer than 100 SNB operations during gestation will remain below the recommended limits for pregnant women [57].
Staff in pathology department
Radiation exposure to pathology staff is very low, and should not require badge monitoring. Even personnel performing unusually high numbers of procedures receive radiation doses well below established limits for members of the general public [59].
Radiation safety precautions
Labelling specimens as radioactive for transportation to the laboratory is not required, since the surface dose rate is <5µGy/h [60].
Radioactive clinical waste
Surgical instruments and pathology slides appear to stay at background radiation levels, while measurable contamination of absorptive surgical sponges and other materials used in proximity to the injection site is observed [61]. It is advisable to monitor these materials for contamination, and contaminated materials should be held for an appropriate period of decay-in-storage before disposal [52, 59].
Injection
The lymphatic anatomy within the oral cavity and oropharynx is extremely complicated and varies significantly between subsites, emphasizing the need for precise injection technique [39, 62, 63].
Patient preparation
No special preparation is needed. Patients should be fully informed about the procedure, including discussion of potential problems such as bleeding and discomfort, before consent can be obtained.
Syringe, activity and volume
Tuberculin syringes with minimal dead space are recommended; otherwise 0.1 ml of air may be drawn into the syringe behind the radiocolloid to ensure complete administration. A 25- or 27-gauge needle should be used. The total activity to be injected may vary, depending on the size and location of the primary tumour. As described in the section “Dosimetry – patient”, there is currently little consensus as to the optimum activity for injection [39, 64, 65], and this varies considerably from 15 to 120 MBq between studies. The total injected activity should be adjusted according to the timing of LSG with respect to surgery. Higher doses are required for a 2-day protocol, in order to ensure the activity exceeds 10 MBq at the time of surgery [50]. Small volumes of 0.1–0.2 ml per aliquot are recommended to minimize contamination due to the resistance of the tongue tissue. Contamination can be avoided by placement of a sheet over the injected region and a gauze swab over the needle puncture site before withdrawal. Following injection, the skin/mucosa should be checked for contamination.
Injection site and depth, and number of injections
Tracer should be injected at 0.1–0.5 cm from the tumour or scar margin. The number of aliquots to be injected varies (two to four) according to the size and location of the lesion. The tracer should be administered on each side of the tumour/scar keeping as a reference the orientation of the surgical scar. For lesions in sites with abundant soft tissue (i.e. soft palate or floor of the mouth) four separate submucosal injections must be given around the lesion (at 3, 6, 9 and 12 o'clock). For lesions located in muscle (i.e. tongue), injections should be performed according to the depth of the lesion. Ideally, the operating surgeon should be present for the injections to ensure consistency with injection of blue dye if used. Following injection, bleeding may be controlled with a gauze swab, and the patient should be asked to use a mouth rinse to minimize pooling of the radiotracer in the oral cavity [34].
Imaging
Introduction
LSG uses a gamma camera to assess the drainage of injected radiotracer via the lymphatic capillaries to the larger collector lymphatics until it either passes through, or is retained within, the regional lymph nodes [66]. Accurate preoperative localization and cutaneous marking of the SLNs correlates well with the precision of the surgical procedure [67, 68].
Cameras and camera settings (quality control)
A gamma camera with a large field of view equipped with a high- or ultrahigh-resolution low-energy collimator should be used, with a 10–20% window centred on the 140-keV energy peak of 99mTc. A two-headed camera allows simultaneous dynamic acquisition in the anterior and a lateral projection allowing more time for the static images and SPECT [69]. Quality control for the gamma camera should be routinely performed and should follow published protocols [70].
Image acquisition
Dynamic acquisition for 20 to 30 min (20 s per frame, with a 128×128 matrix [69] or 256×256 matrix [71]) starting immediately after radiotracer injection will show the drainage pattern and help to differentiate between SLNs, which can appear very early following injection, and second-echelon lymph nodes. Two (or three if a three-headed camera is used) simultaneous images in the anterior and lateral projections is recommended.
Static images in the anterior and lateral projections from one or both sides (and oblique as needed) are acquired (300 s, with a 256×256 matrix) to localize the nodes in three dimensions. If hot nodes are not clearly depicted, static images can be repeated at, for example, 2 h, 4–6 h or even just before surgery. The patient is imaged in the supine position with head up. A small flat pillow under the neck may help to fix the head and neck area.
SPECT imaging may improve the identification of SLNs, especially close to the injection site. Lesion detectability is increased by attenuation and scatter correction, which is easily accomplished with hybrid SPECT/CT devices [69, 72]. The increased anatomical detail provided with CT improves localization of SLNs to the anatomical neck level [69]. SPECT acquisition parameters can be 128×128 matrix, 180° in the anterior L-mode rotation, 3° angle step with 20–25 s per projection [73] or as 60 steps per head, 30 s each, and slice thickness 4.42 mm [69].
CT acquisition parameters differ depending on the CT system used. To date, most reports on SPECT/CT for SNB in oral cancer have used a low-end slow CT scanner (GE Hawkeye) with acquisition performed over 220° using 16 s for each transaxial slice, with a fixed tube current of 2.5 mA, 140 kV, and slice thickness 10 mm [69, 73]. With fast high-end CT scanners providing higher-quality scans, either a low dose or a higher dose of CT can be used. Low dose can be, for example, 20 ms per slice, slice thickness/increment 3/3 mm, and 120 kV. If a diagnostic CT scan is required, intravenous contrast agent can also be used. If CT images are used for attenuation correction, inspection of both uncorrected and attenuation-corrected SPECT images is recommended, to avoid overlooking contrast agent-induced artefacts on the latter.
A number of studies have shown advantages of adding SPECT/CT to planar imaging, including identification of missed SLNs, exclusion of ambiguous SLNs, and/or better anatomical localization in 30–47% of patients [69, 73]. However, it has been suggested that meticulous oblique planar imaging can visualize the additional SLNs seen with SPECT imaging, and this may represent an adequate alternative [43]. Furthermore, a number of investigators have reported no advantage to SPECT imaging with respect to the number and location of visualized hot-spots [74, 75]. The true role of SPECT imaging in OSCC SNB has yet to be determined. If used, SPECT/CT should not be a substitute for meticulous planar imaging technique.
The location of SLNs harvested during surgery does not always correlate perfectly with the preoperative imaging [69], though higher quality CT images can allow visualization of individual SLNs of <1 cm, leading to improved preoperative and intraoperative SLN localization [76].
Body contouring
To facilitate topographic localization, a 57Co flood source (or, if available, a 153Gd source) can be used for simultaneous transmission imaging in each projection. Since there is a risk of missing faint nodes when using a transmission source, it has been suggested that the scan be repeated without a transmission source [77]. Alternatively, a radioactive point source may be used to outline the patient's contour while recording the scan.
Image interpretation
On dynamic imaging, SLNs are identified as one or more foci to which lymphatic drainage passes [78], and may be multiple, in one or several areas of the neck, ipsilateral and/or contralateral to the primary tumour. Imaging should begin immediately, since SLNs can be seen in the first minute after injection [79]. Foci appearing only on later images are also labelled as SLNs, and most appear within 1 to 3 h [43, 80].
According to some reports, SPECT/CT may identify a median of one additional SLN compared with planar imaging. In addition, SLNs located very close to the primary tumour may be detected by SPECT/CT but not with the gamma probe during surgery [69]. While the benefits of SPECT/CT have not been universally accepted [74, 75], both planar and SPECT images demonstrate good or excellent inter- and intraobserver agreement for evaluation of SLNs, with kappa values of 68–89% [43].
Nonvisualization
SLNs are usually detected 15–60 min after radiotracer injection. Failure to detect SLNs may be related to incorrect injection technique or close proximity of SLNs to the injection site (e.g. floor of mouth tumours). In addition, metastatic deposits may block lymphatic drainage causing nonvisualization of SLNs [32, 81]. Repeat injection and imaging may be considered; however, proceeding to neck dissection is preferred in order to avoid a false-negative SLN.
Aberrant nodes and in-transit SLNs
Individual lymphatic mapping by LSG is a major advantage of SNB [81, 82], demonstrating occasional unexpected drainage to, for example, level IV or contralateral metastases from well-lateralized tumours [43, 64, 83–89]. In addition, LSG has been reported to detect “in-transit” lymph nodes: SLNs lying between the primary tumour and the regional lymph basin [90]. These have been described in the context of malignant melanoma, but to date there have been no reports of in-transit SLNs in OSCC.
Report and display
Introduction
There are two main indications for careful report and display of the results from LSG: (1) unambiguous guidance for surgical biopsy, and (2) a comprehensive dataset for ongoing/future studies [37, 43].
Report
The type of radiocolloid, lot number, volume injected, and effective dose should be recorded, along with the initials and title of the nuclear medicine physician or surgeon performing the injection. The type of camera used and imaging technique should be described in detail [69]:
-
1.
Start time for dynamic imaging.
-
2.
Timing and location of the first echelon node(s) to appear.
-
3.
Timing and number of anterior, posterior and oblique recordings.
-
4.
Timing and location of any additional (second echelon) nodes. These should be clearly differentiated from the first echelon nodes.
-
5.
If CT or hybrid imaging is used, the manufacturer, software and protocol should be described in detail. The number and location of nodes recorded by these modalities should be described and compared to planar recordings. If the results of the tomographic images differ from the planar recordings, this should be clearly stated.
Shine-through from the primary tumour or opposite side should be described and marked clearly on the images. Increased absorption in the thyroid gland can be seen due to unstable colloid solution as a result of a colloid production error [91], and this may lead to difficulties in interpreting the LSG images. Artefacts may also occur due to cutaneous contamination at the time of injection [92]. Rarely, a widened lymphatic capillary may form a “colloid lake”; however, the associated hot-spot will invariably disappear during subsequent imaging, in contrast with true SLNs.
Display
LSG findings should be summarized by the nuclear medicine physician, providing a clear, unambiguous report for preoperative consultation. In addition, hard-copy or digital copies of the LSG images should be available to the surgeon, both prior to and during surgery [37, 43].
Skin marking
First echelon nodes should be marked on the skin using an indelible marker of one colour, guided by gamma camera and hand-held gamma probe [93]. Second echelon nodes should be marked with a different colour, and clearly differentiated.
Use of dye
Introduction
The use of blue dye in head and neck mucosal cancer SLN surgery is optional. However, when used it is a useful adjunct to aid SLN localization and harvest. Blue dye cannot be used alone to perform OSCC SNB, but can be used in addition to radiolocalization with preoperative LSG and intraoperative gamma probe use [34].
Following injection, blue dye drains to the SLNs via the same lymphatic pathways as radiocolloid, staining the channels, which can then be followed to the first-echelon nodes. Direct visualization and dissection of these channels is a natural process for the head and neck surgeon.
Rarely, nonradioactive blue nodes may contain metastases in the absence of a tumour-positive radioactive node; two such SLNs were reported in a series of 40 patients undergoing SNB with both radiocolloid and blue dye injection [63]. The hand-held gamma probe is more sensitive for the detection of SLNs, and not all radioactive nodes will also appear blue [28]. However, blue dye may aid performance of SNB, in terms of both technical success of the procedure and identification of subclinical nodal metastasis.
Contraindications and special precautions
Blue dye is contraindicated in children, pregnant women, lactating women and those who have a history of allergy to the blue dye or any of the products. It can, however, be used in all mucosal SLN procedures, for any malignant process for which the procedure has been deemed suitable, including OSCC.
Blue dyes
In the UK and Europe, the blue dye used is Patent Blue V (Laboratoire Guerbet, Aulnay-Sous-Bois, France; Fig. 1) which comes in 2-ml vials at a concentration of 2.5%. Outside Europe, the use of other agents such as Isosulphan Blue (Lymphazurin) is more common. Gloves should be worn to avoid staining, and a gauze swab used to prevent dye spillage where possible. The dye will rarely mask the edge of the tumour and if this is a concern, the tumour edge can be marked prior to injection with staples or diathermy marks.
Timing of injection
Patent Blue V dye is injected at the time of surgery, under general anaesthesia. It takes approximately 10–15 min for a significant amount of dye to travel from the injection site to the SLN and this is the approximate time it takes to scrub, prepare the patient, make the initial excision and begin to explore the neck. The patient and anaesthetist should be informed that the dye will be excreted in the urine, and the urine will remain discoloured for approximately 2 days.
Injection technique
One vial of dye is injected slowly into the tissues surrounding and deep to the tumour, to minimize leakage from ulcerated tumours. Gauze swabs may be used to protect normal tissue and mop up excess dye. The number of injections is usually between two and four, but is as many as is necessary to completely surround the tumour on its deep and lateral surfaces. Occasionally it may be necessary to grab the tongue with forceps or a retracting suture during the injection. The injection site should not be massaged, in order to maintain oncological safety of the procedure.
Adverse effects
Anaphylaxis and allergic reactions, while rare, are a possibility [94], and clinicians should be mindful of this during the injection. In the event of a reaction, the injection should be discontinued and appropriate resuscitation performed. A decision should be made as to whether to continue or abandon the procedure based on clinical findings and discussion between the surgeon and anaesthetist. The mucosa is stained after injection, but the dye tends not to diffuse further than the margins of excision of the tumour and it has not been the authors' (T.S.) experience that dye interferes with pulse oximetry or pathological interpretation of the excised tumour specimen [34].
In summary, injection of blue dye is a useful adjunct to gamma probe localization of the SLN. It is an optional procedure, but one that offers significant advantages for OSCC SNB.
Gamma probe
Introduction
There are a wide variety of available gamma probes with individual feature sets, each requiring specific training and information. In many countries, effective competency training is required as part of the regulations governing the use of radioactivity.
Probe components
The gamma probe is a radiation detector, providing a count rate from gamma rays. The hand-held probe contains the radiation detector, either a crystal or a solid-state device, with surrounding metal shielding and collimation to give a restricted field of view (Fig. 2). It is connected to a power supply and an analyser unit which receives electrical signals from the radiation detector. The analyser and hand-held probe together form the probe system, which may be powered by mains connection or battery. The analyser provides a response related to the detected count rate, usually by audible pitch or volume variation and by a visual display as a dial or digital count rate (counts per second, cps). The probe technology is described in a number of reference books [95–97].
Probe size and shape
Probes typically have outer dimensions of 12–15 mm, with smaller probes producing problems related to the smaller—less-sensitive—detector, and less adequate shielding of the probe housing from gamma rays. Probe tips may be angled relative to the handle. This may be viewed as an advantage for minimal access surgery, or a disadvantage according to the preference of the surgeon.
Probe performance
The probe performance is described in terms of its spatial resolution and its count sensitivity [98–100]. Spatial resolution indicates how spread out the signal is from a point source; Sensitivity is the number of counts per second for a given strength of source. At a typical node depth of 30 mm, a point source node will appear to be about 25 mm wide due to the imperfect spatial resolution of the probe, and resolution worsens with increasing distance. Many nodes contain well below 1% of the injected activity, and with the 6-h half-life of 99mTc the activity in a given node can be low, particularly if the surgery is delayed after injection of the radiopharmaceutical. A probe should be able to achieve sensitivity in the range 650–900 cps/MBq of 99mTc for a 3-cm deep node. For a 3-cm deep node with 1% uptake from a 40-MBq injection of radiocolloid, with surgery 2 h after injection, the surgeon will see a count rate of about 220 cps. The detected count rate falls rapidly with deeper nodes, and if this arises with lower percentage uptake and a longer delay to surgery there may be a much lower count rate and more difficult localization. With experience, localization at low count rates is possible, but with greater variability, longer search time and less confidence than at higher count rates.
The probe also picks up counts from sources that are not directly in front of the probe; gamma rays can penetrate through the side of the probe, and scattered gamma rays can enter the detector. Adequate shielding of the probe is therefore important, especially in OSCC due to close proximity of the injection site. The rejection of scatter is achieved by having a probe with a good “energy resolution”, and with a narrow window.
Probe controls
The probe analyser has a number of settings affecting practical performance of the probe, and therefore ease of SLN localization. These include the following.
Energy window setting
For 99mTc, the probe should be set to a fixed energy level of 140 keV, but the “width” setting is variable. The wider the window, the higher the sensitivity but more scatter is detected. This is especially problematic close to the injection site, and the “high sensitivity” (wider window) setting is therefore most useful for low uptake nodes remote from the injection site.
Collimation
Collimators may be removable, allowing great gain in sensitivity while sacrificing spatial resolution. Removal of the collimation can aid localization of low-uptake nodes remote from the injection site.
Additional shielding
Direct penetration of gamma rays through the side of the probe may be reduced by the use of lead plates to shield the injection site.
Integration time
Some systems allow averaging of the signal over time, reducing signal variability. Integration times of more than one second must be used with caution, since the user may be misled by the delay between the probe position and the corresponding sound signal.
Count range
The probe produces an audible change in pitch between a minimum and maximum counts per second, e.g. 100–1,000 cps. Counts outwith the set range will all produce the same (low or high) pitch, necessitating adjustment. Inappropriate range setting can lead to failure of localization. Some probe systems can automatically adjust the pitch range for the detected counts, though this can be confusing when trying to get a sense of the absolute count at any point.
Care of the probe and quality assurance
All radiation detectors must be checked and managed within a quality assurance programme. Surgeons are advised to work closely with their nuclear medicine colleagues and medical physicists in setting up quality control procedures. Recommendations for testing are:
-
On purchase, tests of performance are advised to give a reference value for sensitivity, energy resolution and spatial resolution, and to form a baseline for day-to-day checks
-
Before each use, a basic check of function and performance with determination of count rate sensitivity to a long-lived radioactive source and its energy spectrum.
-
Visual inspection for damage, particularly cables and connectors. All users must be advised that the probe detector is easily damaged by dropping.
-
In the operating room, aiming the probe at the injection site can demonstrate that the probe is functioning; however, this is not a substitute for quality control checks since even a 50% loss in sensitivity would not have any effect on the general response to the injection site.
Sterility
The probe is placed into a sterile sheath, though this makes the probe tip larger. The skin surface may be scanned before sheathing, in which case the probe must be decontaminated by wiping with 70% alcohol or another supplier-recommended agent. When removing a sheath, care must be taken not to accidentally take off any removable collimator, since these are costly to replace.
Common sources of error or problems
-
1.
Dropping the probe will usually cause it to stop functioning, so staff should be made aware of its fragility, and quality assurance performed before each operating list. A spare probe can easily be interchanged. Damage to the cable and connectors is avoided by careful handling, aided by staff training.
-
2.
Failure to replace a removable collimator considerably reduces spatial resolution.
-
3.
An incorrect energy window setting may be caused by selecting the wrong isotope, or if the quality assurance procedures are performed with a 57Co isotope and the procedure specifies that the energy window is set to 57Co. To avoid this, perform all quality assurance procedures on the 99mTc window, unless the window is unusually narrow, in which case attention must be paid to resetting the window after quality assurance.
-
4.
Good support from radiation experts in the nuclear medicine or medical physics department can be invaluable, particularly for routine quality assurance, optimization and purchase advice on performance. Awareness of the major pitfalls, both technical and patient-related, is essential.
Surgical technique and gamma probe detection
The following remarks are valid provided that: (a) preoperative LSG is carried out, and (b) no cervical cutaneous flap will be raised.
Procedure
At the time of LSG, SLNs are marked on the skin surface under scintigraphic guidance of a 57Co-labelled pen-marker (held 90° to the skin surface) and controlled transcutaneously by the nuclear medicine physician with a collimated, hand-held gamma probe. Marking the skin with the head and neck in a position as similar as possible to the positioning during surgery may facilitate harvesting of the SLN.
Following radiotracer injection and LSG, the patient undergoes general anaesthesia and preparation for operation. Optionally, blue dye may be injected at this time. Transoral excision of the primary tumour is performed either before or after SNB. Prior excision reduces the problem of “shine-through” from the injection site, but potentially limits the usefulness of blue dye due to rapid transit times through the lymphatics from the injection sites.
In the operating room, the gamma probe is covered with sterile latex and applied transcutaneously to confirm the accuracy of the skin markings, which may have changed due to changes in patient positioning between LSG and surgery [101]. The theoretically optimal search pattern is to start closest to the injection site, with the probe perpendicular to the skin, using a raster pattern of parallel lines 2 cm apart at right angles to the direction of the injection site. A rise in activity is then confirmed by scanning in the other direction. Scanning should be no faster than a few centimetres per second. However, excessively slow scanning can lead to loss of information from the change in pitch as the probe passes over a hot node. The drop in counts as the probe is angulated whilst over a hot-spot can confirm location.
Location
The LSG images and skin markings guide the site of incision, which is placed along the relaxed skin tension lines and positioned to facilitate excision of the scar should subsequent neck dissection be required. SLNs are reached using one or more small incisions, and removed from levels I–V according to the classification of Robbins et al. [102]. Subplatysma skin flaps are not routinely raised for biopsy-only procedures. The gamma probe is introduced into the space along the plane of dissection and angled in various directions to guide the surgeon to the SLN, which is then excised. SLNs in the jugular chain are found close to the internal jugular vein and those in level I will usually be found in the submandibular triangle. If blue dye is used, blue-stained lymphatics may be followed to the SLNs, which may be hot, blue, or both. The anatomical location of the SLNs should be noted, as should their colour and radioactivity ex vivo in the operating theatre because both blue dye and radioactivity will dissipate before the pathological examination. In order to avoid potential confusion, surgeons and histopathologists should agree beforehand on the exact nomenclature used for labelling SLNs and drainage basins. Following excision of SLNs, repeated readings are taken of the excision bed to ensure that there are no adjacent hot nodes that also need to be removed [36].
Selection of nodes
In OSCC, multiple SLNs are usually present, with reported mean numbers of 1.3 to 4 (range 1–11) [36]. Preoperative LSG may underestimate the number of SLNs, especially when multiple SLNs are in close proximity [87, 103]. However, the numerous other advantages of preoperative LSG counter the suggestion that it may safely be omitted from the procedure [87]. Careful consideration of inactive lymph nodes in the immediate vicinity of SLNs is imperative. Although non-sentinel nodes should not be excised, there may be a scenario where closely adjacent nodes are almost completely excised while dissecting out a SLN. Although this is uncommon, the non-sentinel node thus labelled may be sent for pathological examination [104].
While preoperative imaging should detect the majority of grossly involved nodes, clinical staging remains imperfect [105]. Any suspicious lymph nodes observed during SNB must be excised, even in the absence of radioactivity, since gross lymphatic involvement may block the flow of radiotracer to these nodes (see also the section “Measured radioactivity”).
SLNs are ranked according to their respective tracer uptake ex vivo, with the SLN with the highest activity named SLN1, the second highest activity SLN2, and so forth. This does not mean that SLN2 is dependent on SLN1, as metastases may be found in any of the multiple SLNs independently [63, 106–108].
Close spatial relation
The problems of “shine-through”, whereby the high radioactivity levels from the injection site are detected from behind the tissue of interest, and “scatter”, in which the direction of radioactivity from the injection site is changed by the tissues and detected by the probe [36], are most prevalent in the submandibular and submental areas of the neck. For floor-of-mouth tumours, where the distance between primary site and SLN is smallest, this creates technical difficulty and results in lower SLN identification rates (86%, vs 96% for other OSCC subsites) [28, 109, 110]. Careful positioning of the gamma probe, judicious use of malleable lead shields and excision of the primary tumour before SLN localization may all help to minimize these effects [34]. Another option to improve identification in level I is to perform some initial dissection below the level of the marginal mandibular nerve, transecting the tissues down to the level of the mylohyoid muscle. In this manner, the lymph nodes are mobilized away from the oral cavity, and the gamma probe placed into the newly created tunnel and directed inferiorly away from the injection site [111].
Activity counting
Following excision, SLN radioactivity is confirmed ex vivo using the gamma probe, and must be above background activity to be classified as hot [43]. The SLN should be placed on a surface away from the patient, or on the upturned probe tip (facing the ceiling). Anatomic location and radioactivity levels (counts per second) are recorded for all excised nodes. All radioactive nodes should be considered SLNs because, while there exists some confusion over the exact definition of a SLN [106], it is best to err on the side of patient safety. The lymphatic basin should be rechecked for reduced radioactivity after SLN excision [112]. Bed counts in the neck after removal of SLN almost never exceed 8–10 cps (with the head of the probe slightly turned away from the injection site).
Risk
SNB is not without risks, and injuries to the facial and spinal accessory nerves are possible through minimal exposure. Although complication rates of less than 1% are reported, the risk of injury to these nerves via minimal-access incisions is theoretically higher during SNB than during neck dissection. Similarly, neck dissection following positive SNB represents re-exploration in a recently operated field, and carries with it higher risks of nerve or vessel damage. This reinforces the need for minimal tissue injury during the initial SNB procedure [111].
Experience
It is clear that experience is needed before a surgeon starts performing SNB, as it carries a steep learning curve. This has led to the recommendation of completion of at least ten SNB-assisted ENDs before the procedure is performed alone [38]. In addition, it is necessary for practitioners of SNB to understand the theoretical aspects including handling of radioactivity and optimal use of gamma probes.
Measured radioactivity
The role of measured counts per second during gamma probe detection is unclear. Because of the narrow anatomic relationships, defining a lower cut-off point for SLNs is practically impossible. It has been suggested that the number of harvested SLNs may be limited to the three nodes with the highest absolute counts per second [87, 113] or the highest ratio of ex vivo node:background activity (as for early studies in melanoma) [25, 114–117], in order to reduce surgical morbidity.
For correct staging, at least the three nodes with the highest activity should be excised as SLNs [104, 113] and all positive SLNs are detected within the first five nodes of highest activity in each patient [87, 104]. The detection of more than five SLNs is very rare, with three-quarters of patients having three or fewer SLNs. For safety’s sake, all radioactive nodes should be excised [69, 104].
In a study investigating the role of radioactivity in SNB, Kovacs et al. [104] found no significant difference in absolute counts per second between positive and negative SLNs (medians of 157 cps and 235 cps, respectively), and that the positive SLN need not have the highest tracer accumulation (range 13–4,716 cps) [36, 104]. Activity in SLNs was not found to correlate with the administered dose, and the highest activity was found in level II. The authors reported that there was one SLN in each patient with a significantly higher count rate than the remaining active nodes, and this node could be found in all levels.
Following SLN excision, the remaining lymphatic basin is searched for residual radioactive nodes by means of an in-situ survey measurement. A count-rate less than one-tenth that of the excised node with the lowest radioactivity is considered indicative that all SLNs have been identified and removed. In some centres, lymph nodes with count rates of less than one-tenth that of the “hottest” excised node are not removed. This practice is based on the results of the large Sunbelt Melanoma trial, demonstrating a low failure rate of 2% [118]. However, no similar data have yet been reported for SCC.
The time from injection has also been found not to affect the relative counts between SLNs [119], or if it does, it affects the results only in cases of very large time spans of >14 hours [120], depending on the half-life of the tracer used. It is important, however, that the time span between injection and surgery is consistent for a given study population.
As a result, the absolute radioactivity counts are less important than relative levels between the excised nodes in the context of SNB. Similarly, absolute radioactivity counts cannot be compared between centres due to differences in protocols.
Pathology evaluation of SLN
In OSCC, SNB has been examined only in the context of relatively small observational cohort studies and the pathology protocols have typically been designed to detect micrometastases and isolated tumour cells with high sensitivity. At present, the significance of finding micrometastases and isolated tumour cells is unknown in OSCC. The grade of evidence is currently at level III, as described in the SIGN methodology for clinical guidelines [121]. Several large-scale validation studies (ACOSOG and the University of Miami [111], European Sentinel Node Trial group [122], the Danish national group [81] and the Brazilian head and neck group [123]) are currently underway.
Histological definitions
The present UICC definitions are shown in Table 1 [31]. Whilst these definitions have been largely accepted, little information is available regarding the evidence on which they are based. The relationships between these definitions and TNM coding are shown in Table 2.
One element which is clearly subjective in nature is the assessment of cell viability, as the significance of individual cytokeratin positive “nonviable cells” is difficult to establish. Various terms have been employed for these cells, including “mummified cells” or thanatosomes [124]. The present authors’ practice (K.H., P.S.) is to include such elements in the morphological description, with careful correlation to the adjacent H&E-stained section. Features which may be useful include the lack of a nucleus, but the biological potential of these cells is as yet unknown.
In addition, the presence of cells in the lymphatic plexus should always be recorded. Whilst their significance is unknown, it appears that they do not represent extracapsular extension of tumour.
Protocol
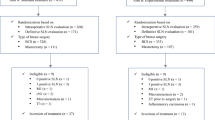
A well-defined, written, standard operating procedure should be established between the surgical team and the reporting pathology laboratory. This should include how the specimen should be delivered to the laboratory, outline the supporting documentation which accompanies it, and include appropriate elements of radiological protection practice. Other important elements may include agreed turnaround times and the manner in which the results are to be reported. An overview of the proposed pathological evaluation protocol is presented in Fig. 3.
Gross sectioning
The node or nodal basin should be fixed in 10% neutral buffered formalin (or equivalent) for 24 hours, as per standard laboratory practice. The nodes are described macroscopically, including dimensions, and excess fat is carefully trimmed away. Nodes less than 2 mm (longest dimension) should be processed whole, while nodes 2–5 mm should be cut through the hilum or longest pole to pole diameter, and both halves processed en face. Nodes greater than 5 mm should be cut into 2-mm slices longest pole to pole, with processing of all slices en face.
Step sectioning
A routine H&E section is prepared, and metastatic disease reported if present. If negative, six exact serial sections are mounted, and separately numbered 1–6. Next, 150 µm of material is discarded, or retained for research, before a further six numbered serial sections are mounted. This pattern is continued throughout the entire block. All number 3 sections are stained by the H&E method, and metastatic disease reported if present. If negative or equivocal, immunocytochemistry (IHC) is performed on all number 2 sections using a pancytokeratin antibody (see below), and the slides examined for positivity. IHC-positive slides are compared with the adjacent section 3 H&E slide. The remaining sections may be used if required.
Much of the published literature has utilized AE1/AE3 pancytokeratin antibody. However, concern has been expressed regarding the specificity of this anticytokeratin cocktail. Cross-reactivity is a problem seen with a number of pan-cytokeratin antibodies, and may mandate the use of more than one antibody in SNB protocols to clearly delineate micrometastases and isolated tumour cells from other elements in the node, such as dendritic cells and macrophages. However, presently it is reasonable to assume that any reputable commercially available pancytokeratin antibody (such as AE1/AE3 or MNF116) may be used. It is important to recognize artefacts and any cytokeratin-positive components should always be compared with adjacent sections stained by H&E (Figs. 4, 5, 6, 7, 8 and 9).
Cytokeratin-positive cells in a SLN stained by CKC pancytokeratin. The white arrow shows a contaminant squame (this can be ascertained by the geometric outline, lack of nucleus and by focusing at high power). The black arrows show nonnucleated individual tumour cells, and dendritic cells can be seen in the background
Adjacent field to Fig. 5 stained by AE1/AE3, showing absence of tumour cells
Microscopy
Sections should be examined using a good-quality bright-field microscope and equivocal findings discussed with an experienced colleague. Where pancytokeratin-positive cells are present, it is essential that adjacent sections are stained to allow morphological comparison.
Report
The side, number and level of each node basin in the neck must be recorded. A diagram provided by the surgical team should be incorporated into the pathology record where possible.
The report must include details of the numbers of nodes found in each individual basin and which nodes were hot, blue, both, or unlabelled. The dimensions of each node must be included and the macroscopic appearance of the gross and cut surfaces stated.
-
Macrometastasis
-
Note the largest dimension of the metastatic deposit in each node, and whether extracapsular spread is present or not.
-
-
Micrometastasis
-
Should be recorded, even in the presence of macrometastasis.
-
The largest dimension should be recorded.
-
Anatomical location within the node: capsular, subcapsule, parenchymal.
-
Unifocal or multifocal. It is often not possible to be confident of the exact numbers.
-
Presence of extracapsular spread. This is permitted if the deposit is peripherally located and is associated with a reactive stromal response.
-
-
Isolated tumour cells
-
If evident, should be recorded, even in the presence of macro or micrometastasis.
-
If cohesive, the size of the largest deposit should be stated.
-
If dispersed, note the anatomical distribution.
-
-
Benign inclusions including naevus cells, salivary inclusions and false-positive cytokeratin artefacts (e.g. dendritic cells or scattered nonviable anucleate cells) should be recorded.
The histopathological features of isolated tumour cells need careful description, as the UICC size cut-off by necessity encompasses small metastases which vary greatly in size and presumably in biological potential. Positive findings using nonmorphological methods in the absence of histologically proven metastasis are generally considered as isolated tumour cells.
Other methodologies
Frozen sections
The use of frozen section evaluation for SLNs has been described in a number of recent reports, and the results appear promising with negative predictive values ranging from 83% to 99% [64, 125, 126]. These results are in contrast to an earlier report by Civantos et al. who described poor sensitivity of frozen section compared with step-serial sectioning in a series of 43 patients with oral cancer [127]. The main advantage to the technique is that it may allow a majority of patients to undergo a single-stage procedure. While the use of frozen section evaluation is advocated by some authors, it has not yet gained universal acceptance.
Imprint cytology
The use of imprint cytology in conjunction with frozen sections in the assessment of SLNs has been described in other tumours such as breast adenocarcinoma. One study in OSCC based on 30 cases demonstrated high sensitivity and specificity [128] though a recent study showed frozen section evaluation to be a more accurate method of intraoperative diagnosis [125]. Imprint cytology has an advantage over frozen section evaluation in that no tissue is lost in generation of the sample; however, much larger studies are required before considering adoption into the protocol.
Reverse transcriptase polymerase chain reaction
Methods with increased sensitivity, such as cytokeratin RT-PCR, have been suggested. The small number of studies published demonstrate expression of cytokeratins in nodes which were metastasis-negative on initial assessment. However, only a proportion of the nodes demonstrated metastases on serial sectioning [129, 130]. The clinical role of these methods in the future remains uncertain given the ongoing concerns regarding their specificity together with the associated medicolegal problems, given that significant tissue must be used which has not been assessed histopathologically.
Burden of work
The authors recognize that on average 2.5 sentinel node basins are yielded per neck side. The protocol above may produce up to 12 levels per node. If three nodes are present in each basin there could be 180 slides to examine. On the other hand, the majority of SLNs are small and the nodes from a single basin can often be grouped into one cassette (using ink to identify ‘hot’ and ‘blue’ nodes) saving laboratory time and effort. In addition, the described protocol has the ability to detect all micrometastases.
According to Cochran’s principle, metastatic deposits tend to cluster in the plane of the hilum, and some authors argue the case for examination of bisected SLNs at three or six levels only [131]. Although such a protocol can theoretically miss a micrometastasis [132], it may turn out that no useful information is added by levelling through the block beyond six levels. However, several studies have shown that additional SLNs are upstaged by step serial sectioning with cytokeratin immunohistochemistry, compared with H&E only [81].
Outcome analysis
The success of this multidisciplinary staging technique depends on good communication between all of the individual components: imaging, surgery, and histopathology. The multidisciplinary team setting should be utilized for the discussion of every patient, and regular audit of patient outcomes against published data should be carried out. SLNs should be successfully located and harvested in >90% of patients [28]. The accuracy of the technique can be assessed by the proportion of patients whose SLN contains metastases, which should match that of END (20–30%, depending on patient population and tumour size [133]). Lastly, the rate of false-negatives (SLN-negative patients who develop early recurrent disease) should be <5% [134].
Further studies are required to determine the full clinical significance of micrometastasis and individual tumour cells in OSCC. The biological potential of the tumour cells may vary with different types of tumours, and clinical decisions currently have to be made on the basis of grade, stage and margin status of the primary lesion as well as on microscopic findings in the SLN [135, 136]. The optimum protocol will hopefully emerge from the large-scale trials and studies currently in progress [81, 109, 111, 122, 123]. One of the major aims of SNB in OSCC is to achieve better staging, and thorough pathological examination of SLNs remains the standard.
Summary
Successful application of the SNB technique is dependent on good communication between all members of the multidisciplinary team, and this joint guideline represents an extension of that approach. SNB provides an additional tool for staging patients with early OSCC. However, it is not without limitations, and all practitioners of SNB must be aware of these. It is hoped that this document will serve as a reference outlining the optimal practice for the provision of SNB in patients with OSCC, based on the best currently available evidence. As such, the use of the above protocol is recommended until further data, in the form of large prospective studies currently underway, becomes available.
Abbreviations
- SNB:
-
Sentinel node biopsy
- OSCC:
-
Oral/Oropharyngeal squamous cell carcinoma
- EANM:
-
European Association of Nuclear Medicine
- SENT:
-
European Sentinel Node Trial group
- END:
-
Elective neck dissection
- SLN:
-
Sentinel lymph node
- cN0:
-
Clinical node-negative
- pN0:
-
Pathological node-negative
- cN+:
-
Clinical node-positive
- pN+:
-
Pathological node-positive
- Tc-99m:
-
Technetium-99
- LSG:
-
Lymphoscintigraphy
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- USg-FNAC:
-
Ultrasound-guided fine-needle aspiration cytology
- FDG-PET:
-
18F-fluoro-deoxyglucose positron emission tomography
- PET/CT:
-
FDG-PET with low dose CT
- MBq:
-
Mega-becquerel
- mSv:
-
MilliSievert
- µSv:
-
MicroSievert
- µGy:
-
MicroGray
- keV:
-
kilo-electron volt
- SPECT:
-
Single photon emission computed tomography
- IV:
-
Intravenous
- ICRP:
-
International Commission on Radiological Protection
- 57Co:
-
Cobalt-57
- 153Gd:
-
Gadolinium-153
- cps:
-
counts per second
- QA:
-
Quality assurance
- QC:
-
Quality control
- UICC:
-
Union Internationale Contre le Cancer (International Union Against Cancer)
- H&E:
-
Haematoxylin-eosin stain
- MM:
-
Micrometastasis
- ITC:
-
Isolated/individual tumour cells
- RT-PCR:
-
Reverse-transcriptase polymerase chain reaction
References
Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics 2002. CA Cancer J Clin 2005;55:74–108.
Pitman KT, Johnson JT, Myers EN. Effectiveness of selective neck dissection for management of the clinically negative neck. Arch Otolaryngol Head Neck Surg 1997;123:917–22.
Shah JP, Candela FC, Poddar AK. The patterns of cervical lymph node metastases from squamous carcinoma of the oral cavity. Cancer 1990;66:109–13.
Spiro JD, Spiro RH, Shah JP, Sessions RB, Strong EW. Critical assessment of supraomohyoid dissection. Am J Surg 1988;156:286–9.
Gourin CG, Conger BT, Porubsky ES, Sheils WC, Bilodeau PA, Coleman TA. The effect of occult nodal metastases on survival and regional control in patients with head and neck squamous cell carcinoma. Laryngoscope 2008;118:1191–4.
Don DM, Anzai Y, Lufkin RB, Fu YS, Calcaterra TC. Evaluation of cervical lymph node metastasis in squamous carcinoma of the head and neck. Laryngoscope 1995;105:669–74.
Leemans CR, Tiwari R, Van der Waal I, Karim AB, Nauta JJ, Snow GB. The efficacy of comprehensive neck dissection with or without postoperative radiotherapy in nodal metastases of squamous cell carcinoma of the upper respiratory and digestive tracts. Laryngoscope 1990;100:1194–8.
Ambrosch P, Kron M, Fischer G, Brinck U. Micrometastases in carcinoma of the upper aerodigestive tract: detection, risk of metastasizing, and prognostic value of depth of invasion. Head Neck 1995;17:473–9.
Kane SV, Gupta M, Kakade AC, D' Cruz A. Depth of invasion is the most significant histological predictor of subclinical cervical lymph node metastasis in early squamous carcinomas of the oral cavity. Eur J Surg Oncol 2006;32:795–803.
Pimenta Amaral TM, Da Silva Freire AR, Carvalho AL, Pinto CA, Kowalski LP. Predictive factors of occult metastasis and prognosis of clinical stages I and II squamous cell carcinoma of the tongue and floor of the mouth. Oral Oncol 2004;40:780–6.
Yamamoto E, Miyakawa A, Kohama G. Mode of invasion and lymph node metastasis in squamous cell carcinoma of the oral cavity. Head Neck Surg 1984;6:938–47.
Alkureishi LW, Ross GL, Shoaib T, Soutar DS, Robertson AG, Sorensen JA, et al. Does tumor depth affect nodal upstaging in squamous cell carcinoma of the head and neck. Laryngoscope 2008;118:629–34.
Goerkem M, Braun J, Stoeckli SJ. Evaluation of clinical and histomorphological parameters as potential predictors of occult metastases in sentinel lymph nodes of early squamous cell carcinomas of the oral cavity. Ann Surg Oncol 2009; in press.
Byers RM. Modified neck dissection: a study of 967 cases from 1970 to 1980. Am J Surg 1985;150:414–21.
Byers RM, Wolf PF, Ballantyne AJ. Rationale for elective modified neck dissection. Head Neck Surg 1988;10:160–7.
Shah JP. Cervical lymph node metastases-diagnostic, therapeutic and prognostic implications. Oncology 1990;4:61–9.
Shah JP, Andersen PE. Evolving role of modifications in neck dissection for oral squamous carcinoma. Br J Oral Maxillofac Surg 1995;33:3–8.
Brazilian Head and Neck Cancer study group. Results of a prospective trial on elective modified radical classical versus supraomohyoid neck dissection in the management of oral squamous carcinoma. Am J Surg 1998;176:422–6.
Pitman KT. Rationale for elective neck dissection. Am J Otolaryngol 2000;21:31–7.
Cheng A, Schmidt BL. Management of the N0 neck in oral squamous cell carcinoma. Oral Maxillofac Surg Clin North Am 2008;20:477–97.
Lindberg R. Distribution of cervical lymph node metastases from squamous cell carcinoma of the upper respiratory and digestive tracts. Cancer 1972;29:1446–9.
Byers RM, Clayman GL, McGill D, Andrews T, Kare RP, Roberts DB, et al. Selective neck dissections for squamous carcinoma of the upper aerodigestive tract: patterns of regional failure. Head Neck 1999;21:499–505.
Morton DL, Wen DR, Wong JH, Economou JS, Cagle LA, Storm FK, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 1992;127:392–9.
Cabanas RM. An approach for the treatment of penile carcinoma. Cancer 1977;39:456–66.
Alex JC, Weaver DL, Fairbank JT, Rankin BS, Krag DN. Gamma-probe-guided lymph node localization in malignant melanoma. Surg Oncol 1993;2:303–8.
Morton DL, Wen DR, Cochran AJ. Management of early-stage melanoma by intraoperative lymphatic mapping and selective lymphadenectomy or "watch and wait". Surg Oncol Clin North Am 1992;1:247–59.
Krag DN. Surgical resection and radiolocalization of the SLN in breast cancer using a gamma probe. Surg Oncol 1993;2:335–40.
Ross GL, Soutar DS, Gordon MacDonald D, Shoaib T, Camilleri I, Roberton AG, et al. Sentinel node biopsy in head and neck cancer: preliminary results of a multicenter trial. Ann Surg Oncol 2004;11:690–6.
Stoeckli SJ, Steinert H, Pfaltz M, Schmid S. Sentinel lymph node evaluation in squamous cell carcinoma of the head and neck. Otolaryngol Head Neck Surg 2001;125:221–6.
Kovács AF, Döbert N, Gaa J, Menzel C, Bitter K. Positron emission tomography in combination with sentinel node biopsy reduces the rate of elective neck dissections in the treatment of oral and oropharyngeal cancer. J Clin Oncol 2004;22:3973–80.
Sobin LH, Wittekind Ch, editors. TNM classification of malignant tumours. 6th ed. New York: Wiley; 2002.
Hornstra MT, Alkureishi LWT, Ross GL, Shoaib T, Soutar DS. Predictive factors for failure to identify sentinel nodes in head and neck squamous cell carcinoma. Head Neck 2008;30:858–62.
Alex JC, Krag DN. The gamma-probe-guided resection of radio-labeled primary lymph nodes. Surg Oncol Clin North Am 1996;5:33–41.
Shoaib T, Soutar DS, Prosser JE, Dunaway DJ, Gray HW, McCurrach GM, et al. A suggested method for sentinel node biopsy in squamous cell carcinoma of the head and neck. Head Neck 1999;21:728–33.
Kovács AF, Stefenelli U, Seitz O, Middendorp M, Diener J, Sader R, et al. Positive sentinel lymph nodes are a negative prognostic factor for survival in T1–2 oral/oropharyngeal cancer − a long-term study on 103 patients. Ann Surg Oncol 2009;16:233–9.
Werner JA, Dünne AA, Ramaswamy A, Dalchow C, Behr T, Moll R, et al. The sentinel node concept in head and neck cancer: solution for the controversies in the N0 neck? Head Neck 2004;26:603–11.
Ross GL, Soutar DS, Shoaib T, Camilleri IG, MacDonald DG, Robertson AG, et al. The ability of lymphoscintigraphy to direct sentinel node biopsy in the clinically N0 neck for patients with head and neck squamous cell carcinoma. Br J Radiol 2002;75:950–8.
Ross GL, Shoaib T, Soutar DS, MacDonald DG, Camilleri IG, Bessent RG, et al. The First International Conference on Sentinel Node Biopsy in Mucosal Head and Neck Cancer and adoption of a multicenter trial protocol. Ann Surg Oncol 2002;9:406–10.
Stoeckli SJ, Pfaltz M, Ross GL, Steiner HC, MacDonald DG, Wittekind C, et al. The second international conference on sentinel node biopsy in mucosal head and neck cancer. Ann Surg Oncol 2005;12:919–24.
Wilhelm AJ, Mijnhout GS, Franssen EJF. Radiopharmaceuticals in sentinel lymph-node detection – an overview. Eur J Nucl Med 1999;26:S36–42.
Jimenez IR, Roca M, Vega E, García ML, Benitez A, Bajén M, et al. Particle sizes of colloids to be used in sentinel lymph node radiolocalization. Nucl Med Commun 2008;29:166–72.
Kovács AF, Döbert N, Walendzik H, Zaplatnikov K, Landes CA. The diagnostic role of radioactivity in sentinel nodes in oral and oropharyngeal cancer. Cancer Biother Radiopharm 2006;21:535–43.
Thomsen JB, Sørensen JA, Grupe P, Krogdahl A. Sentinel lymph node biopsy in oral cancer: validation of technique and clinical implications of added oblique planar lymphoscintigraphy and/or tomography. Acta Radiol 2005;46:569–75.
GE Healthcare. Nanocoll® technical leaflet. GE Healthcare, Milan, Italy. 2009.
Millar AM, O’Brien LM, Beattie LA, Craig F, McDade J. Validation of an extended shelf-life for Tc-99m albumin nanocolloid injection. Nucl Med Commun 2007;28:A15.
Burton DA, Cashman JN. Allergic reaction to nanocolloid during lymphoscintigraphy for sentinel node biopsy. Br J Anaesth 2002;89:105.
Chicken DW, Mansouri R, Ell PJ, Keshtgar MR. Allergy to technetium-labeled nanocolloidal albumin for sentinel node identification. Ann R Coll Surg Engl 2007;89:W12–3.
Keller B, Yawalkar N, Pichler C, Braathen LR, Hunger RE. Hypersensitivity reaction against patent blue during sentinel lymph node removal in three melanoma patients. Am J Surg 2007;193:122–4.
Koizumi M, Nomura E, Yamada Y, Takiguchi T, Tanaka K, Yoshimoto M, et al. Sentinel node detection using Tc-99m-rhenium sulphide colloid in breast cancer patients: evaluation of 1 day and 2 day protocols, and a dose-finding study. Nucl Med Commun 2003;24:663–70.
Chakera AH, Hesse B, Burak Z, Ballinger JR, Britten A, Caracò C, et al. EANM-EORTC recommendations for sentinel node diagnostics in melanoma. Eur J Nucl Med Mol Imaging 2009; in press.
Buscombe J, Paganelli G, Burak ZE, Waddington W, Maublant J, Prats E, et al. Sentinel node in breast cancer procedural guidelines. Eur J Nucl Med Mol Imaging 2007;12:2154–9.
Waddington WA, Keshtgar MRS, Taylor I, Lakhani SR, Short MD, Ell PJ. Radiation safety of the sentinel node technique in breast cancer. Eur J Nucl Med 2000;27:377–91.
Pandit-Tskar NN, Dauer LT, Montgomery L, St Germain J, Zanzonico PB, Divgi CR. Organ and fetal absorbed dose estimates from Tc-99m-sulfur colloid lymphoscintigraphy and sentinel node localization in breast cancer patients. J Nucl Med 2006;47:1202–8.
International Commission on Radiological Protection. ICRP Publication 54: Individual monitoring for intakes of radionuclides by workers: design and interpretation. Annals of the ICRP, Volume 19/1-3, ISBN-13: 9780080356006, ISBN-10: 008035600-1, 1989.
Sera T, Mohos G, Papos M, Osvay M, Varga J, Lazar M, et al. Sentinel node detection in malignant melanoma patients: radiation safety considerations. Dermatol Surg 2003;29:141–5.
Stratmann SL, McCarthy TM, Kuhn JA. Radiation safety with breast sentinel node biopsy. Am J Surg 1999;25:196–202.
Klausen TL, Chakera AH, Friis E, Rank F, Hesse B, Holm S. Radiation doses to staff involved in sentinel node operations for breast cancer. Clin Physiol Funct Imaging 2005;25:196–202.
Nejc D, Wrzesien M, Piekarski J, Olszewski J, Pluta P, Kuśmierek J, et al. Sentinel node biopsy in skin melanoma patients – measurements of absorbed doses of radiation to the hands of medical staff. J Surg Oncol 2006;1;93:355–61.
Glass EC, Basinski JE, Krashne DL, Guiliano AE. Radiation safety considerations for sentinel node techniques. Ann Surg Oncol 1999;6:10–1.
IAEA. Nuclear medicine resources manual. Chapter 8: Radiation safety practice in nuclear medicine. Vienna: IAEA; 2006. p. 509–21.
Nugent N, Hill AD, Casey M, Kelly L, Dijkstra B, Collins CD, et al. Safety guidelines for radiolocalised sentinel node resection. Ir J Med Sci 2001;170:236–8.
Chiesa F, Mauri S, Grana C, Tradati N, Calabrese L, Ansarin M, et al. Is there a role for sentinel node biopsy in early N0 tongue tumors? Surgery 2000;128:16–21.
Shoaib T, Soutar DS, MacDonald DG, Camilleri IG, Dunaway DJ, Gray HW, et al. The accuracy of head and neck carcinoma sentinel lymph node biopsy in the clinically N0 neck. Cancer 2001;91:2077–83.
Stoeckli SJ. Sentinel node biopsy for oral and oropharyngeal squamous cell carcinoma of the head and neck. Laryngoscope 2007;117:1539–51.
De Cicco C, Trifirò G, Calabrese L, Bruschini R, Ferrari ME, Travaini LL, et al. Lymphatic mapping to tailor selective lymphadenectomy in cN0 tongue carcinoma: beyond the sentinel node concept. Eur J Nucl Med Mol Imaging 2006;33:900–5.
Modi S, Stanton AW, Mortimer PS, Levick JR. Clinical assessment of human lymph flow using removal rate constants of interstitial macromolecules: a critical review of lymphoscintigraphy. Lymphat Res Biol 2007;5:183–202.
Uren RF, Howman-Giles RB, Chung D, Thompson JF. Role of lymphoscintigraphy for selective sentinel lymphadenectomy. Cancer Treat Res 2005;127:15–38.
Glass EC, Essner R, Morton DL. Kinetics of three lymphoscintigraphic agents in patients with cutaneous melanoma. J Nucl Med 1998;39:1185–90.
Bilde A, von Buchwald C, Mortensen J, Marving J, Hamilton TM, Kirkegaard J, et al. The role of SPECT-CT in the lymphoscintigraphic identification of sentinel nodes in patients with oral cancer. Acta Otolaryngol 2006;126:1096–103.
International Electrotechnical Commission. IEC/TR 61948-2 Ed. 1.0 English. Nuclear medicine instrumentation - Routine tests - Part 2: Scintillation cameras and single photon emission computed tomography imaging. 2001. Geneva: International Electrotechnical Commission.
Tartaglione G, Vigili MG, Rahimi S, Celebrini A, Pagan M, Lauro L, et al. The impact of superficial injections of radiocolloids and dynamic lymphoscintigraphy on sentinel node identification in oral cavity cancer: a same-day protocol. Nucl Med Commun 2008;29:318–22.
Wagner A, Schicho K, Glaser C, Zettinig G, Yerit K, Lang S, et al. SPECT-CT for topographic mapping of sentinel lymph nodes prior to gamma probe-guided biopsy in head and neck squamous cell carcinoma. J Craniomaxillofac Surg 2004;32:343–9.
Khafif A, Schneebaum S, Fliss DM, Lerman H, Metser U, Ben-Yosef R, et al. Lymphoscintigraphy for sentinel node mapping using a hybrid single photon emission CT (SPECT)/CT system in oral cavity squamous cell carcinoma. Head Neck 2006;28:874–9.
Haerle SK, Hany TF, Strobel K, Sidler D, Stoeckli SJ. Is there an additional value of SPECT/CT over lymphoscintigraphy for sentinel node mapping in oral/oropharyngeal squamous cell carcinoma? Ann Surg Oncol 2009; in press
Keski-Santti H, Matzke S, Kauppinen T, Tornwall J, Atula T. Sentinel lymph node mapping using SPECT-CT fusion imaging in patients with oral cavity squamous cell carcinoma. Eur Arch Otorhinolaryngol 2006;263:1008–12.
Lopez R, Payoux P, Gantet P, Esquerre JP, Boutault F, Paoli JR. Multimodal image registration for localization of sentinel nodes in head and neck squamous cell carcinoma. J Oral Maxillofac Surg 2004;62:1497–504.
Uren RF, Howman-Giles RB, Shaw HM, Thompson JF, McCarthy WH. Lymphoscintigraphy in high-risk melanoma of the trunk: predicting draining node groups, defining lymphatic channels and locating the sentinel node. J Nucl Med 1993;34:1435–40.
Uren RF, Howman-Giles RB, Thompson JF, Roberts J, Bernard E. Variability of cutaneous lymphatic flow rates in melanoma patients. Melanoma Res 1998;8:279–82.
Nieuwenhuis EJ, Pijpers R, Castelijns JA, Snow GB. Lymphoscintigraphic details of sentinel lymph node detection in 82 patients with squamous cell carcinoma of the oral cavity and oropharynx. Nucl Med Commun 2003;24:651–6.
Even-Sapir E, Lerman H, Lievshitz G, Khafif A, Fliss DM, Schwartz A, et al. Lymphoscintigraphy for sentinel node mapping using a hybrid SPECT/CT system. J Nucl Med 2003;44:1413–20.
Bilde A, von Buchwald C, Therkildsen MH, Mortensen J, Kirkegaard J, Charabi B, et al. Need for intensive histopathologic analysis to determine lymph node metastases when using sentinel node biopsy in oral cancer. Laryngoscope 2008;118:408–14.
Werner JA, Dunne AA, Myers JN. Functional anatomy of the lymphatic drainage system of the upper aerodigestive tract and its role in metastasis of squamous cell carcinoma. Head Neck 2003;25:322–32.
Frerich B, Forster M, Schiefke F, Wittekind C, Hemprich A, Sabri O. Sentinel lymph node biopsy in squamous cell carcinomas of the lips and the oral cavity – a single center experience. J Surg Oncol 2007;95:97–105.
Alvarez Amézaga J, Barbier Herrero L, Pijoan del Barrio JL, Martín Rogriguez JC, Romo Simón L, Genolla Subirats J, et al. Diagnostic efficacy of sentinel node biopsy in oral squamous cell carcinoma. Cohort study and meta-analysis. Med Oral Patol Oral Cir Bucal 2007;12:E235–E243.
Shoaib T, Soutar DS, MacDonald DG, Gray HW, Ross GL. The nodal neck level of sentinel lymph nodes in mucosal head and neck cancer. Br J Plast Surg 2005;58:790–4.
Gallegos-Hernandez JF, Hernandez-Hernandez DM, Flores-Diaz R, Sierra-Santiesteban I, Pichardo-Romero P, rias-Ceballos H, et al. The number of sentinel nodes identified as prognostic factor in oral epidermoid cancer. Oral Oncol 2005;41:947–52.
Hoft S, Maune S, Muhle C, Brenner W, Czech N, Kampen WU, et al. Sentinel lymph-node biopsy in head and neck cancer. Br J Cancer 2004;91:124–8.
Kontio R, Leivo I, Leppanen E, Atula T. Sentinel lymph node biopsy in oral cavity squamous cell carcinoma without clinically evident metastasis. Head Neck 2004;26:16–21.
Mozzillo N, Chiesa F, Botti G, Caraco C, Lastoria S, Giugliano G, et al. Sentinel node biopsy in head and neck cancer. Ann Surg Oncol 2001;8:103S–5S.
Uren RF, Howman-Giles R, Thompson JF, McCarthy WH, Quinn MJ, Roberts JM, et al. Interval nodes: the forgotten sentinel nodes in patients with melanoma. Arch Surg 2000;135:1168–72.
Klutmann S, et al. Lymphoscintigraphy in tumors of the head and neck using double tracer technique. J Nucl Med 1999;40(5):776–82.
Warner J, Hovey S, Crawford ES. Contamination problem with sentinel node localization procedure: a case study. J Nucl Med Technol 2002;30:18–20.
Laasanen MS, Heikkinen JO, Saarakkala S, Paajanen H. Localization of sentinel nodes in breast cancer: novel method and device to help pen marking of active nodes during gamma camera imaging. Phys Med Biol 2005;50:N49–54.
Scherer K, Studer W, Figueiredo V, Bircher AJ. Anaphylaxis to isosulfan blue and cross-reactivity to patent blue V: case report and review of the nomenclature of vital blue dyes. Ann Allergy Asthma Immunol 2006;96:497–500.
Keshtar MRS, Waddington WA, Ell PJ, Lakhani SR. The sentinel node in surgical oncology. Berlin: Springer; 1999.
Nieweg OE, Essner R, Reintgen DS, Thompson JF (eds) Lymphatic mapping and probe applications in oncology. New York: Marcel Dekker; 2000.
Cody HS (ed) Sentinel lymph node biopsy. London: Martin Dunitz; 2002.
Perkins AC, Britten AJ. Specification and performance of intra-operative gamma probes for sentinel node detection. Nucl Med Commun 1999;20:309–15.
Tiourina T, Arends B, Huysmans D, Rutten H, Lemaire B, Muller S. Evaluation of surgical gamma probes for radioguided sentinel node localisation. Eur J Nucl Med 1998;25:1224–31.
Britten AJ. A method to evaluate intra-operative gamma probes for sentinel lymph node localisation. Eur J Nucl Med 1999;26:76–83.
Alex JC. The application of sentinel node radiolocalization to solid tumors of the head and neck: a 10-year experience. Laryngoscope 2004;114:2–19.
Robbins KT, Medina JE, Wolfe GT, Levine PA, Sessions RB, Pruet CW. Standardizing neck dissection terminology. Official report of the Academy's Committee for Head and Neck Surgery and Oncology. Arch Otolaryngol Head Neck Surg 1991;117:601–5.
Thomsen JB, Sorensen JA, Grupe P, Karstoft J, Krogdahl A. Staging N0 oral cancer: lymphoscintigraphy and conventional imaging. Acta Radiol 2005;46:492–6.
Kovacs AF, Acker P, Berner U, Risse JH. Sentinel lymph node excision. Treatment method of the N0 neck in patients with oral and oropharyngeal carcinoma. HNO. 2001;49(8):646–53.
Alkureishi LW, Ross GL, MacDonald DG, Shoaib T, Gray H, Robertson G, et al. Sentinel node in head and neck cancer: use of size criterion to upstage the N0 neck in head and neck squamous cell carcinoma. Head Neck 2007;29:95–103.
Nieweg OE, Tanis PJ, Kroon BB. The definition of a sentinel node. Ann Surg Oncol 2001;8:538–41.
Werner JA, Dünne AA, Ramaswamy A, Folz BJ, Brandt D, Külkens C, et al. Number and location of radiolabeled, intraoperatively identified sentinel nodes in 48 head and neck cancer patients with clinically staged N0 and N1 neck. Eur Arch Otorhinolaryngol 2002;259:91–6.
Hyde NC, Prvulovich E, Newman L, Waddington WA, Visvikis D, Ell P. A new approach to pretreatment assessment of the N0 neck in oral squamous-cell carcinoma: the role of sentinel node biopsy and positron emission tomography. Oral Oncol 2003;39:350–60.
Alkureishi LWT, Ross GL, Shoaib T, Soutar DS, Robertson AG, Sorensen JA, et al. Sentinel node biopsy in oral/oropharyngeal squamous cell cancer: five year follow-up. Presented at the American Head and Neck Society Annual Meeting, San Francisco, California, July 2008.
Civantos F, Zitsch R, Bared A. Sentinel node biopsy in oral squamous cell carcinoma. J Surg Oncol 2007;96:330–6.
Civantos FJ, Werner JA, Bared A. Sentinel node biopsy in cancer of the oral cavity. Oper Tech Otolaryngol Head Neck Surg 2005;16:275–85.
Chikamatsu K, Kamada H, Ninomiya H, Takahashi K, Sakurai T, Oriuchi N, et al. A preliminary study on sentinel lymph node biopsy: feasibility and predictive ability in oral cavity cancer. Ann Nucl Med 2004;18:257–62.
Werner JA, Dünne AA, Ramaswamy A, Folz BJ, Lippert BM, Moll R, et al. Sentinel node detection in N0 cancer of the pharynx and larynx. Br J Cancer 2002;87:711–5.
Albertini JJ, Cruse CW, Rapaport D, Wells K, Ross M, DeConti R, et al. Intraoperative radio-lympho-scintigraphy improves sentinel lymph node identification for patients with melanoma. Ann Surg 1996;223:217–24.
Bostick P, Essner R, Sarantou T, Kelley M, Glass E, Foshag L, et al. Intraoperative lymphatic mapping for early-stage melanoma of the head and neck. Am J Surg 1997;174:536–9.
Brobeil A, Kamath D, Cruse CW, Rapaport DP, Wells KE, Shons AR, et al. The clinical relevance of sentinel lymph nodes identified with radiolymphoscintigraphy. J Fla Med Assoc. 1997;84:157–60.
Glass LF, Messina JL, Cruse W, Wells K, Rapaport D, Miliotes G, et al. The use of intraoperative radiolymphoscintigraphy for sentinel lymph node biopsy in patients with malignant melanoma. Dermatol Surg 1996;22:715–20.
McMasters KM, Noyes RD, Reintgen DS, Goydos JS, Beitsch PD, Davidson BS, et al.; Sunbelt Melanoma Trial. Lessons learned from the Sunbelt Melanoma Trial. J Surg Oncol 2004;86:212–23.
Carlson GW, Murray DR, Thourani V, Hestley A, Cohen C. The definition of the sentinel lymph node in melanoma based on radioactive counts. Ann Surg Oncol 2002;9:929–33.
Essner R, Bostick PJ, Glass EC, Foshag LJ, Haigh PI, Wang HJ, et al. Standardized probe-directed sentinel node dissection in melanoma. Surgery 2000;127:26–31.
Scottish Intercollegiate Guidelines Network 2008 SIGN 50: A guideline developer's handbook Chapter 7 ISBN 19781905813254 http://www.sign.ac.uk/guidelines/fulltext/50/index.html.
Ross GL, on behalf of the Sentinel European Node Trial (SENT) Organising Committee. Sentinel node biopsy for squamous cell carcinoma of the oral cavity: preliminary results of the SENT trial. Presented at the Annual Meeting of the American Head and Neck Society (AHNS), San Francisco, July 2008.
Chone CT, Magalhes RS, Etchehebere E, Camargo E, Altemani A, Crespo AN. Predictive value of sentinel node biopsy in head and neck cancer. Acta Otolaryngol 2008;128:920–4.
Papadimitriou JC, Drachenberg CB, Brenner DS, Newkirk C, Trump BF, Silverberg SG. “Thanatosomes”: a unifying morphogenetic concept for tumor hyaline globules related to apoptosis. Hum Pathol 2000;31:1455–65.
Terada A, Hasegawa Y, Yatabe Y, Hyodo I, Ogawa T, Hanai N, et al. Intraoperative diagnosis of cancer metastasis in sentinel lymph node of oral cancer patients. Oral Oncol 2008;44:838–43.
Tschopp L, Nuyens M, Stauffer E, Krause T, Zbären P. The value of frozen section analysis of the sentinel lymph node in clinically N0 squamous cell carcinoma of the oral cavity and oropharynx. Otolaryngol Head Neck Surg 2005;132:99–102.
Civantos FJ, Moffat FI, Goodwin WJ. Lymphatic mapping and sentinel lymphadenectomy for 106 head and neck lesions: contrasts between oral cavity and cutaneous malignancy. Laryngoscope 2006;16:1–15.
Asthana S, Deo SV, Shukla NK, Jain P, Anand M, Kumar R. Intraoperative neck staging using sentinel node biopsy and imprint cytology in oral cancer. Head Neck 2003;25:368–72.
Garrel R, Dromard M, Costes V, Barbotte E, Comte F, Gardiner Q, et al. The diagnostic accuracy of reverse transcription-PCR quantification of cytokeratin mRNA in the detection of sentinel lymph node invasion in oral and oropharyngeal squamous cell carcinoma: a comparison with immunohistochemistry. Clin Cancer Res 2006;12:2498–505.
Shores CG, Yin X, Funkhouser W, Yarbrough W. Clinical evaluation of a new molecular method for detection of micrometastases in head and neck squamous cell carcinoma. Arch Otolaryngol Head Neck Surg 2004;130:937–42.
Cochran AJ, Ohsie SJ, Binder SW. Pathobiology of the sentinel node. Curr Opin Oncol 2008;20:190–5.
Thomsen JB, Christensen RK, Sorensen JA, Krogdahl A. Sentinel lymph nodes in cancer of the oral cavity: is central step-sectioning enough? J Oral Pathol Med 2007;36:425–9.
Woolgar JA. Micrometastasis in oral/oropharyngeal squamous cell carcinoma: incidence, histopathological features and clinical implications. Br J Oral Maxillofac Surg 1999;37:181–6.
von Buchwald C, Bilde A, Shoaib T, Ross G. Sentinel node biopsy: the technique and the feasibility in head and neck cancer. ORL J Otorhinolaryngol Relat Spec 2002;64:268–74.
Rutgers EJ. Sentinel node biopsy: interpretation and management of patients with immunohistochemistry-positive sentinel nodes and those with micrometastases. J Clin Oncol 2008;26:698–702.
Woolgar JA, Beirne JC, Vaughan ED, Lewis-Jones HG, Scott J, Brown JS. Correlation of histopathologic findings with clinical and radiologic assessments of cervical lymph-node metastases in oral cancer. Int J Oral Maxillofac Surg 1995;24:30–7.
Acknowledgments
The authors would like to thank the European Association of Nuclear Medicine's Physics, Dosimetry and Radiopharmacy Committees for their assistance in production of this article.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
This article is to appear in the November 2009 issue of European Journal of Nuclear Medicine and Molecular Imaging, Volume 36, Number 11 and of Annals of Surgical Oncology, Volume 16, Number 11.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Alkureishi, L.W.T., Burak, Z., Alvarez, J.A. et al. Joint practice guidelines for radionuclide lymphoscintigraphy for sentinel node localization in oral/oropharyngeal squamous cell carcinoma. Eur J Nucl Med Mol Imaging 36, 1915–1936 (2009). https://doi.org/10.1007/s00259-009-1248-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-009-1248-0