Abstract
Purpose
The intra-arterial administration of 90Y microspheres is a new palliative treatment option for unresectable liver metastases. The aim of this study was to quantitatively assess changes in FDG uptake and tumour size following 90Y microsphere treatment (SIR-Spheres) using 18F-fluorodeoxyglucose (FDG) PET/CT imaging.
Methods
Five patients with unresectable liver metastases who had failed multiple prior chemotherapy regimens received seven 90Y microsphere treatments to a single liver lobe. All patients underwent a baseline PET/CT scan prior to treatment, as well as up to four follow-up PET/CT scans. The tumour area of 30 liver metastases was measured on CT and the FDG uptake was semiquantitatively assessed by calculation of standardised uptake values (SUVs). A total of 18 FDG-PET/CT scans were performed.
Results
The SUVs in the 30 treated liver metastases decreased from 6.5±2.3 at baseline to 4.2±1.8 after the first follow-up PET/CT scan (p=0.001). In contrast, the SUVs of untreated metastases increased slightly from 7.2±2.3 to 8.0±0.8. There was no difference in FDG uptake in treated versus untreated normal liver tissue. Using a previously defined threshold of 20% decrease in SUV from baseline to determine response, 20 out of 30 liver metastases were considered to have responded at the first follow-up PET/CT scan approximately 1 month after treatment. In these metastases, the SUV decreased by 47±12%, compared with a slight increase by 5.9±19% in ten non-responding metastases (p=0.0001). The changes in tumour size did not correlate with changes in FDG uptake. On the first follow-up PET/CT scan, the tumour area on CT increased by 3.1±57% in treated metastases compared with 23.3±32% in untreated metastases. A wide range of post-treatment changes of target lesions was observed on CT, including an increase in the size of hypodense lesions, necrotic features and complete resolution of CT abnormalities.
Conclusion
The metabolic information obtained from FDG-PET/CT seems to provide a more accurate and earlier assessment of therapy response following 90Y microsphere treatment than does the anatomical CT information.
Similar content being viewed by others
Introduction
The intra-arterial administration of 90Y microspheres (SIR-Spheres, Sirtex Medical Ltd., Sydney, Australia) is a new palliative treatment option for unresectable liver tumours [1]. It has been initially established for the treatment of unresectable hepatocellular carcinoma [2, 3] and has also been applied to liver metastases [4–6]. The radiopharmaceutical consists of non-biodegradable 90Y-imprinted resin-based microspheres with a diameter of approximately 29–35 μm. After injection into the hepatic artery, the radiolabelled microspheres induce microembolisation of the hepatic arterioles. While hepatocytes receive blood supply from the hepatic artery and the portal vein, liver metastases primarily depend on the nutrition from the hepatic artery. The radiolabelled microspheres are administered under fluoroscopic monitoring until the blood flow in the hepatic artery is suspended, resulting in mechanical occlusion of the neovascular arterioles [7]. 90Y is a beta-emitter with a half-life of 64 h and an average penetration depth in tissue of approximately 2.4 mm. In addition to the mechanical occlusion, a substantial radiation dose is delivered to the tumour tissue by the locally trapped 90Y microspheres, ranging from 30 to 60 Gy depending on the activity administered.
Promising response rates have been reported following 90Y microsphere treatment of unresectable liver metastases [1, 7, 8]. In a randomised trial of 90Y microspheres plus hepatic arterial infusion chemotherapy versus chemotherapy alone, 74 patients were assessed for tumour response, time to disease progression, overall survival, quality of life and treatment-related toxicity [8]. Tumour response was measured by changes in tumour areas and tumour volumes as well as by changes in serum carcino-embryonic antigen (CEA) levels. The combination of 90Y microspheres plus hepatic arterial infusion chemotherapy induced substantially higher tumour response rates and increased progression-free survival compared with hepatic arterial infusion chemotherapy alone. In another study, Herba and Thirlwell [1] treated 37 patients with metastatic liver disease. Follow-up included CT or ultrasound as well as CEA measurements but response was difficult to assess, especially when diffuse and irregular tumour infiltration was present. However, decreased tumour attenuation and sharper delineation of tumour lesions was noted on CT scans. Based on these and other studies, selective internal radiation therapy with 90Y microspheres combined with the administration of hepatic arterial infusion chemotherapy was recently approved by the FDA for unresectable colorectal liver metastases. It is to be noted that the optimal procedures for assessment of therapy response still need to be determined.
Positron emission tomography (PET) using 18F-fluorodeoxyglucose (FDG) provides diagnostic information based on the metabolic activity of malignant tissue. FDG-PET has been shown to be superior for staging and restaging of various types of cancer, including colorectal cancer [9, 10]. PET allows accurate quantification of FDG uptake in tissue, and previous studies have demonstrated that standardised uptake values (SUVs) provide highly reproducible parameters of tumour glucose utilisation [11]. Combined positron emission tomography and computed tomography (PET/CT) is a new imaging modality that allows the acquisition of spatially registered PET and CT data in one imaging procedure, permitting tissue characterisation as well as assessment of the exact localisation and extent of tumour tissue [12].
The relationship between changes in tumour glucose metabolism and response to treatment has been well established in different types of tumours over recent years. However, little information is available on the potential role of FDG-PET/CT in the evaluation of tumour response to radiolabelled microsphere treatment. The goal of this retrospective analysis was to directly compare changes in FDG uptake and tumour size following 90Y microsphere treatment of unresectable liver metastases, by means of FDG-PET/CT.
Materials and methods
Patients
A retrospective analysis was performed in five patients, two females and three males (aged 42–72 years), who underwent 90Y microsphere treatment (SIR-Spheres) of unresectable liver metastases and had failed multiple prior chemotherapy regimens. All patients had a baseline PET/CT scan and at least one follow-up PET/CT scan approximately 1 month after treatment. Four patients had liver metastases from colorectal cancer and one patient had liver metastases from pancreatic cancer. All patients had undergone surgery for the primary tumour. One patient had undergone resection of the left liver lobe prior to 90Y microsphere treatment. All patients had previously received systemic and hepatic arterial infusion chemotherapy but none of them had received systemic chemotherapy within the 2 months prior to 90Y microsphere treatment. At the time of 90Y microsphere treatment, the duration of disease was 18.8±6.7 months.
90Y microsphere treatment
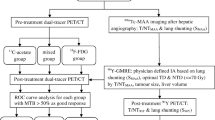
All patients underwent pre-therapy hepatic arteriography via the femoral artery to assess the vascular supply of the metastatic lesions and to evaluate the vascular anatomy of the liver. Then, 99mTc-macroaggregated albumin (MAA) was injected into the hepatic artery supplying the target liver lobe. 99mTc-MAA and 90Y microspheres have a similar particle size (approximately 30 μm), and the distribution of 99mTc-MAA reflects the delivery of the 90Y microspheres, which were administered in a separate setting for the therapy. Planar and single-photon emission computed tomographic (SPECT) images of 99mTc-MAA were obtained after completion of the hepatic arteriogram to visualise the particle distribution within the target tissue and to exclude significant liver–lung shunting as well as any possible aberrant extrahepatic flow. No dose adjustment for lung shunting was necessary. In a separate session, 90Y microspheres were injected under fluoroscopic control in either the left or the right hepatic artery under low pressure after ensuring adequate catheter placement. A total of seven 90Y microsphere treatments were performed: five into the right hepatic artery and two into the left hepatic artery.
The mean administered activity was 930 MBq (470–1,390 MBq) or 25.1 mCi (12.7–37.6 mCi) 90Y microspheres. The activity for each patient was based on delivering a radiation dose of approximately 50 Gy to the target tissue. The mass of the target liver lobe was obtained from CT images. The calculated radiation dose delivered to the target liver lobe was 44±6 Gy (33–52 Gy). In addition, patients received hepatic arterial infusion chemotherapy with 5-FU (600 mg/m2) over 2 h through the same catheter as was used to deliver the SIR-Spheres. The interval between the infusion of chemotherapy and treatment with 90Y microspheres did not exceed approximately 60 min.
PET/CT imaging protocol
PET/CT imaging was performed on a Reveal BGO PET/CT (CPS Innovations, Knoxville, TN), which consists of an ECAT EXACT HR+ PET scanner operated in 3D acquisition mode and a Siemens Somatom Emotion single-slice helical CT scanner. Patients were fasted for at least 6 h prior to FDG-PET/CT imaging with the exception of liberal water intake. An intravenous catheter was placed for radiopharmaceutical administration and the patient’s blood glucose level was determined prior to tracer injection. The blood glucose levels of all patients were below 150 mg/dl at the time of FDG injection. Each patient received 370–550 MBq (10–15 mCi) of 18F-FDG intravenously, depending on the body weight. After tracer injection, patients rested on a comfortable chair during the FDG uptake period. PET/CT imaging was initiated approximately 60 min after tracer injection. A scanogram was performed to determine the axial range of the study. The CT scanning was performed from the base of the skull through the pelvis in one imaging procedure. Helical CT scanning (pitch 1.0, 80–120 mAs, 130 kVp) started approximately 40 s after administration of intravenous contrast agent (120 ml Optiray 350, Mallinckrodt, St. Louis, MO, USA) to image the liver in the portal venous phase. Following the CT, 3D PET data were acquired using 5-min bed positions. The PET acquisition included a dead time correction and online delayed coincidence subtraction to correct for random coincidences.
Data processing was performed using the manufacturer’s software. The helical CT scan was reconstructed by filtered backprojection into 512×512 pixel images with a slice thickness of 2.4 mm to match the PET scan. Images were reconstructed using ordered subset expectation maximisation (OSEM) with two full iterations of eight subsets. Rescaled CT images were used to produce attenuation correction values for the PET emission reconstruction.
PET/CT image analysis
PET: Regions of interest (ROIs) were drawn around the liver metastases on axial PET images. In the slice with the highest tumour activity, the maximum pixel activity was obtained and normalised to the injected dose and the patient’s body weight, yielding SUVs.
CT: The size (area) of the liver metastases was obtained on the corresponding CT image. On the slice with the largest tumour extension, the area was calculated as the product of perpendicular diameters.
If multiple liver metastases were present, all clearly separate lesions were analysed. The PET and CT information from the baseline PET/CT scan was available to accurately obtain corresponding SUVs and area measurements from liver metastases on follow-up PET/CT scans.
Assessment of treatment response
Evaluation of metabolic response was accomplished by comparing the relative changes in tumour FDG uptake, expressed as SUVs. The SUVs from FDG-PET/CT performed approximately 1 and 3 months after 90Y microsphere treatment (and from additional follow-up PET/CT studies when available) were compared with the baseline study. Metabolic response has previously been defined as a decrease in SUV of more than twice the standard deviation of spontaneous changes, which equates to a decrease of 20% or more [11, 13]. Response was classified according to the following criteria: liver metastases with a decrease in SUV of more than 20% were classified as responding to 90Y microsphere treatment while metastases with a decrease in SUV of less than 20%, no change in SUV or an increase in SUV were classified as not responding to treatment.
Patient follow-up
Patients were clinically followed up, the follow-up including measurement of the tumour marker CEA. Serum CEA was measured at baseline and monthly after 90Y microsphere treatment. PET/CT was performed approximately 1 month after treatment in all patients and 3 months after treatment in all patients except one; thereafter it was performed as clinically indicated.
Statistical analysis
Differences in SUV between baseline and follow-up PET/CT were analysed using the Wilcoxon signed rank test. The Mann-Whitney U test was used to analyse differences in changes in SUV between responding and non-responding metastases at the first follow-up PET/CT scan. A p value of <0.01 was considered statistically significant.
Results
PET imaging
Five patients received seven treatments with 90Y microspheres. The baseline PET/CT scan was performed 29±21 days before therapy. Subsequently, the first follow-up PET/CT scan was performed 33±10 days after therapy and a second follow-up PET/CT scan (n=5) was performed 101±31 days after treatment. A total of 38 liver metastases were measurable on PET and CT, of which 30 were treated with 90Y microspheres.
In the 30 treated liver metastases, the SUV decreased from 6.5±2.3 at baseline to 4.2±1.8 after the first follow-up PET/CT scan (p=0.001). In contrast, the SUV of untreated metastases increased slightly from 7.2±2.3 to 8.0±0.8. The SUVs obtained from normal liver tissue did not differ when comparing baseline with follow-up PET/CT. The details of changes in SUV over time for all seven 90Y microsphere treatments are shown in Tables 1, 2, 3, 4 and 5.
Twenty out of 30 liver metastases showed a decrease in SUV of more than 20% when comparing the baseline scan with the first follow-up PET/CT scan. In these metastases, the SUV decreased on average by 47±12%. The SUV in the ten non-responding metastases increased slightly by 5.9±19%. The difference was statistically significant (p=0.0001). A second follow-up PET/CT scan was performed following five 90Y microsphere treatments and included a total of 24 metastatic lesions that were measurable on baseline PET/CT. In 20 out of 24 metastases, the response classification did not change between the first and second follow-up PET/CT scans, whereas four lesions demonstrated an increase in SUV on the second follow-up PET/CT scan. Figure 1 demonstrates the changes in FDG uptake and tumour size on PET/CT in a patient with multiple metastases in the right liver lobe.
Transaxial PET/CT images of the upper abdomen in a patient with multiple metastases in the right liver lobe. On the first follow-up PET/CT scan after 90Y microsphere treatment of the right liver lobe, a marked decrease in FDG uptake is visible in the metastasis in the posterior lateral aspect of the right lobe, with residual activity centrally in the right lobe. The abnormal FDG uptake had resolved on the second follow-up PET/CT scan; however, there is a new area of increased FDG uptake in the (untreated) left lobe
CT imaging
The changes in tumour size did not correlate with changes in FDG uptake. A wide range of post-treatment changes of target lesions was observed on CT, including an increase in the size of hypodense lesions, necrotic- features and complete resolution of CT abnormalities. On the first follow-up PET/CT scan, performed 33±10 days after 90Y microsphere treatment, the tumour area on CT increased by 3.1±57% in treated metastases (n=29) compared with an increase of 23.3±32% in untreated metastases (n=8). Changes in the area of treated metastases ranged from a decrease of 91% to an increase of 174%. There was no significant difference between the changes in tumour area in PET responders (6.2±64%) versus metabolic non-responders (−3.4±42%).
On the second follow-up PET/CT scan, performed 101±31 days after treatment, the tumour area of treated metastases (n=23) increased slightly by 7.0±93% on CT. However, a wide range of changes in tumour area was observed, from a decrease of 83% to an increase of 340%. As shown in Tables 1–5, the changes in FDG uptake preceded changes in tumour area and further follow-up PET/CT imaging confirmed the initial PET response.
Treatment response on a patient basis
In the first patient, all ten measurable metastases responded, with a mean decrease in SUV between baseline and the first follow-up PET/CT scan of 50±12%. There was a further decrease in SUV after the second follow-up PET/CT scan, and the FDG uptake in five out of ten metastases was at background level. In the second patient, the decrease in SUV was less pronounced (−33±18) and only four out of five metastases demonstrated a decrease in SUV of more than 20%. In the third patient, a large metastasis in the left lobe of the liver did not show increased FDG uptake on baseline PET and there was no change after treatment. On the second follow-up PET/CT scan, however, there was a threefold increase in FDG uptake, which responded to subsequent hepatic arterial infusion chemotherapy. After approximately 10 weeks, the patient received a second 90Y microsphere treatment to the right lobe of the liver. One metastasis responded with a decrease in SUV of 62%, whereas a second metastasis showed an increase in SUV of 24%. Overall, the patient did not respond, and multiple new intrahepatic metastases were seen on the first follow-up PET/CT scan. In the fourth patient, a decrease in SUV was observed in all seven liver metastases but only four showed a decrease in SUV of more than 20%. After approximately 11 weeks, the patient received a second 90Y microsphere treatment to the left lobe of the liver, which showed diffuse FDG uptake at baseline PET/CT, indicating extensive diffuse tumour involvement; there was no significant change in SUV on follow-up PET/CT. In the fifth patient, one out of four metastases responded, whereas three had an increase in SUV. In addition, multiple new intrahepatic metastases were seen on the first follow-up PET/CT scan, leading to subsequent local and systemic chemotherapy.
No side-effects of 90Y microspheres were identified in extrahepatic organs or tissues. The median follow-up for all patients was 22 months (range 3–23). Median survival after 90Y microsphere therapy was 19 months. Four patients had an elevated baseline CEA level (range 4.6–124.0 ng/ml) and one patient had a normal CEA level. The CEA level decreased in three out of the five patients within 2 months after therapy; one patient had an initial increase in CEA before a decline was observed. Two patients had a rising CEA level despite 90Y microsphere treatment.
Discussion
We used combined FDG-PET/CT imaging for assessment of therapy response in patients with liver metastases and found significant metabolic and morphological changes approximately 4 weeks after intrahepatic treatment with 90Y microspheres. Metabolic changes were more accurate than anatomical changes in the assessment of treatment response. A threshold of 20% decrease in SUV has recently been suggested as a cut-off value to differentiate responding from non-responding tumours [11, 13]. Prospectively applying this threshold, it was found that 20 out of 30 measurable liver metastases responded to 90Y microsphere treatment. The SUV in responding metastases decreased by 47±12%, compared with an increase of 5.9±19% in non-responding metastases (p=0.0001).The differences in FDG uptake of non-responding metastases between baseline and follow-up PET/CT were comparable to those of untreated liver metastases.
In contrast to the coherent changes on FDG-PET, a wide range of post-treatment changes in target lesions was observed on CT, including an increase or decrease in tissue attenuation as well as in the size of metastases. Some metastases developed necrotic- features while others were less distinct on CT, but a complete resolution was seen in only a few metastases. Colorectal liver metastases are frequently hypovascular and have a lower attenuation than normal liver, which is best detectable by portal venous phase imaging [14]. Helical CT with portal venous phase imaging was also used in our study, and most of the liver metastases were seen on both the PET and the CT portion of the pre-treatment PET/CT scan. Consistent with previous reports on the diagnostic accuracy of PET versus CT for the detection of liver metastases, PET showed additional metastases not seen on CT [9]. All patients had received previous treatments, and it is of note that some hypodense lesions apparent on CT did not display increased FDG uptake on PET, suggesting that the aforementioned treatments had been successful. The identification of increased metabolic activity of viable tumour might be a distinct advantage of FDG-PET, particularly relevant when planning treatment with 90Y microspheres for previously treated liver metastases.
An important finding of our study is that changes in tumour size did not correlate with changes in FDG uptake. On the first follow-up PET/CT scan, performed approximately 4 weeks after treatment, the average tumour area on CT was essentially unchanged compared with that on the baseline scan. However, there were substantial post-treatment alterations, as shown by the wide variation of changes in the size of metastases (Tables 1–6), from a decrease of 91% to an increase of 174%. When the changes in tumour area in metastases showing a metabolic response as assessed by FDG-PET were compared with those in metastases not showing such a response, no significant difference was observed (6.2±64% vs −3.4±42% respectively). It is noteworthy that the tumour area in untreated metastases increased by 23.3±32% compared with baseline. On the second follow-up PET/CT scan, approximately 3 months after treatment, the average tumour area in treated metastases increased non-significantly by 7.0±93%, again with wide variation of changes in size. These data clearly demonstrate the limitations of CT in accurately assessing therapy response after intrahepatic therapy with 90Y microspheres.
Currently, little information is available on the use of imaging modalities to assess response following 90Y microsphere therapy. In a phase I or II study which included 37 patients with metastatic liver disease, 15 patients had tumour involvement in the liver that was diffuse, irregular or infiltrating with mixed or poor vascularity, as a result of which definitive imaging changes could not be appreciated on follow-up scans [1]. Mirroring our own results, Wong et al. [15] also recently found a significant difference between the metabolic and the anatomical response in eight patients when comparing FDG-PET with CT and MRI obtained at baseline and approximately 3 months after treatment. The metabolic response after 90Y microsphere treatment was significantly greater than the response on CT or MRI, and reduction in the serum CEA level was significantly correlated with the PET response but not with the CT or MRI response. The CEA levels in our study were only of limited use for treatment evaluation since only one liver lobe was treated at a time and four out of five patients had metastases in both lobes. In a larger series the same group analysed FDG-PET semiquantitatively and found a significantly greater percentage of metabolic response in the response group compared with the non-response group [16]. However, the analysis was based on the FDG uptake in the entire liver (lobe) and did not address changes in individual metastases.
An increase in tumour size is generally associated with disease progression. The WHO or more recently the RECIST criteria have been established to monitor response to chemotherapy [17]. For other types of therapies, however, such as laser ablation, chemoembolisation and radiofrequency ablation, even completely necrotic lesions may not demonstrate a significant reduction in size [18]. For chemoembolisation a marked discrepancy was found between the reduction in tumour size seen on CT and histopathology [19]. Our data suggest that the RECIST criteria might also not be valid for 90Y microsphere treatment. The combined arterial embolisation and internal radiation might not result in a proportional reduction of viable tumour and tumour size. Since the full radiation dose delivered from 90Y takes several weeks, the observed initial increase in tumour size in some metastases at the first follow-up PET/CT scan might have been due to oedema and tissue swelling 4 weeks after treatment.
In contrast, the metabolic information provided by PET/CT consistently documented therapeutic response. Several studies have shown that changes in tumour metabolism occur early in the course of therapy and precede the reduction in tumour size [20–23]. These studies suggest that quantification of tumour glucose metabolism is highly accurate for monitoring the effect of chemotherapy. In breast cancer, sequential FDG-PET imaging provided a sensitive means of early detection of response to therapy when compared with histopathology [20, 22, 23]. In oesophageal and gastric cancer, the initial decrease in FDG uptake in tumour tissue also correlated well with the results of histological response after neoadjuvant treatment [24–26].
Although PET/CT provided co-registered PET and CT images, there is potential for misregistration due to patient movement and internal organ movement, e.g. during breathing between the CT and PET data acquisition [12]. In our study most of the liver metastases were well aligned between PET and CT images. In a few cases in which there was obvious misalignment, the implemented software was used for realignment of the PET and CT images. In our experience from this small series, combined PET/CT imaging is very helpful in the treatment evaluation of patients with colorectal liver metastases. The co-registered anatomical and metabolic information allowed exact identification of individual metastases on pre-treatment and post-treatment scans and was particularly useful in cases in which the post-treatment metabolic activity was at background level. In addition, whole-body PET/CT allowed accurate assessment of both the hepatic and the extrahepatic extent of disease. FDG-PET/CT also permitted differentiation between viable and necrotic metastases, which poses a frequent problem in the imaging or follow-up of colorectal liver metastases, especially after previous treatment, as discussed above. Combined PET/CT may become an important modality for the early assessment of treatment response after intrahepatic microsphere treatment. The co-registered anatomical and metabolic information allows the identification and exact localisation of residual viable tumour that can either be re-treated with 90Y microspheres or targeted by another therapeutic approach such as radiofrequency ablation.
Interestingly, we did not observe differences in FDG uptake in treated versus untreated normal liver tissue. Since, the administration of 90Y microspheres into the hepatic artery resulted in occlusion of the neovascular as well as the hepatic arterioles one could expect changes in the metabolic activity of normal liver tissue. In addition, the non-specific microembolisation of hepatic arterioles in the treated liver lobe resulted in considerable radiation exposure of normal liver tissue. However, no apparent increase in FDG uptake due to inflammatory reactions was observed 4 weeks after the 90Y microsphere treatment. PET imaging using 15O-labelled water could help to elucidate the changes in blood flow after administration of radiolabelled microspheres and the duration of vascular occlusion.
There are several limitations of our study beside the small number of patients studied. The most important limitation is the general lack of a gold standard for assessment of treatment response. Since 90Y microspheres are primarily used in the palliative setting of unresectable liver metastases, histopathology following treatment is generally not obtained. Clinical end-points might be helpful on an individual patient basis. Patient survival and quality of life depend largely on the extent of disease, the number and location of metastases, the presence of extrahepatic disease and subsequent local and systemic treatments after the administration of radiolabelled microspheres. An inherent difference between FDG-PET and CT measurements also has to be taken into account. There is a direct relationship between tumour growth and increase in tumour size on CT but not usually with an increase in FDG uptake. However, the FDG-PET response criteria that we used took this into account by classifying response as a decrease in SUV of more than 20% and non-response as a decrease in SUV of less than 20%, no change or an increase in SUV.
Conclusion
Compared with the anatomical information obtained from CT alone, the metabolic information from FDG-PET/CT appears to provide a more accurate and earlier assessment of therapy response following treatment with 90Y. Changes in FDG uptake preceded changes in tumour size and response could be assessed as early as 4 weeks after treatment. Nevertheless, the co-registered PET/CT images were specifically helpful in the exact localisation of metabolic abnormalities when comparing baseline with follow-up scans. PET/CT may be useful in defining the optimal dosing of 90Y microspheres, in determining early recurrence and in helping to stratify patients for re-treatment or alternative therapeutic options.
References
Herba MJ, Thirlwell MP. Radioembolization for hepatic metastases. Semin Oncol 2002;29:152–9.
Houle S, Yip TK, Shepherd FA, Rotstein LE, Sniderman KW, Theis E, et al. Hepatocellular carcinoma: pilot trial of treatment with Y-90 microspheres. Radiology 1989;172:857–60.
Lau WY, Ho S, Leung TW, Chan M, Ho R, Johnson PJ, et al. Selective internal radiation therapy for nonresectable hepatocellular carcinoma with intraarterial infusion of 90yttrium microspheres. Int J Radiat Oncol Biol Phys 1998;40:583–92.
Blanchard RJ, Morrow IM, Sutherland JB. Treatment of liver tumors with yttrium-90 microspheres alone. Can Assoc Radiol J 1989;40:206–10.
Gray BN, Burton MA, Kelleher DK, Anderson J, Klemp P. Selective internal radiation (SIR) therapy for treatment of liver metastases: measurement of response rate. J Surg Oncol 1989;42:192–6.
Yan ZP, Lin G, Zhao HY, Dong YH. An experimental study and clinical pilot trials on yttrium-90 glass microspheres through the hepatic artery for treatment of primary liver cancer. Cancer 1993;72:3210–5.
Stubbs RS, Cannan RJ, Mitchell AW. Selective internal radiation therapy with yttrium-90 microspheres for extensive colorectal liver metastases. J Gastrointest Surg 2001;5:294–302.
Gray B, Van Hazel G, Hope M, Burton M, Moroz P, Anderson J, et al. Randomised trial of SIR-Spheres plus chemotherapy vs. chemotherapy alone for treating patients with liver metastases from primary large bowel cancer. Ann Oncol 2001;12:1711–20.
Huebner RH, Park KC, Shepherd JE, Schwimmer J, Czernin J, Phelps ME, et al. A meta-analysis of the literature for whole-body FDG PET detection of recurrent colorectal cancer. J Nucl Med 2000;41:1177–89.
Rohren EM, Turkington TG, Coleman RE. Clinical applications of PET in oncology. Radiology 2004;231:305–32.
Weber WA, Ziegler SI, Thodtmann R, Hanauske AR, Schwaiger M. Reproducibility of metabolic measurements in malignant tumors using FDG PET. J Nucl Med 1999;40:1771–7.
Townsend DW, Carney JP, Yap JT, Hall NC. PET/CT today and tomorrow. J Nucl Med 2004;45:4S–14S.
Weber WA, Petersen V, Schmidt B, Tyndale-Hines L, Link T, Peschel C, et al. Positron emission tomography in non-small-cell lung cancer: prediction of response to chemotherapy by quantitative assessment of glucose use. J Clin Oncol 2003;21:2651–7.
Sica GT, Ji H, Ros PR. CT and MR imaging of hepatic metastases. AJR Am J Roentgenol 2000;174:691–8.
Wong CY, Salem R, Raman S, Gates VL, Dworkin HJ. Evaluating 90Y-glass microsphere treatment response of unresectable colorectal liver metastases by [18F]FDG PET: a comparison with CT or MRI. Eur J Nucl Med Mol Imaging 2002;29:815–20.
Wong CY, Salem R, Qing F, Wong KT, Barker D, Gates V, et al. Metabolic response after intraarterial 90Y-glass microsphere treatment for colorectal liver metastases: comparison of quantitative and visual analyses by 18F-FDG PET. J Nucl Med 2004;45:1892–7.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 2000;92:205–16.
Kamel IR, Fishman EK. Recent advances in CT imaging of liver metastases. Cancer J 2004;10:104–20.
Takayasu K, Arii S, Matsuo N, Yoshikawa M, Ryu M, Takasaki K, et al. Comparison of CT findings with resected specimens after chemoembolization with iodized oil for hepatocellular carcinoma. AJR Am J Roentgenol 2000;175:699–704.
Wahl RL, Zasadny K, Helvie M, Hutchins GD, Weber B, Cody R. Metabolic monitoring of breast cancer chemohormonotherapy using positron emission tomography: initial evaluation. J Clin Oncol 1993;11:2101–11.
Romer W, Hanauske AR, Ziegler S, Thodtmann R, Weber W, Fuchs C, et al. Positron emission tomography in non-Hodgkin’s lymphoma: assessment of chemotherapy with fluorodeoxyglucose. Blood 1998;91:4464–71.
Schelling M, Avril N, Nährig J, Kuhn W, Römer W, Sattler D, et al. Positron emission tomography using [F-18]fluorodeoxyglucose for monitoring primary chemotherapy in breast cancer. J Clin Oncol 2000;18:1689–95.
Smith FW, Heys SD, Evans NT, Roeda D, Gvozdanovic D, Eremin O, et al. Pattern of 2-deoxy-2-[18F]-fluoro-D-glucose accumulation in liver tumours: primary, metastatic and after chemotherapy. Nucl Med Commun 1992;13:193–5.
Weber WA, Ott K, Becker K, Dittler HJ, Helmberger H, Avril NE, et al. Prediction of response to preoperative chemotherapy in adenocarcinomas of the esophagogastric junction by metabolic imaging. J Clin Oncol 2001;19:3058–65.
Ott K, Fink U, Becker K, Stahl A, Dittler HJ, Busch R, et al. Prediction of response to preoperative chemotherapy in gastric carcinoma by metabolic imaging: results of a prospective trial. J Clin Oncol 2003;21:4604–10.
Wieder HA, Brucher BL, Zimmermann F, Becker K, Lordick F, Beer A, et al. Time course of tumor metabolic activity during chemoradiotherapy of esophageal squamous cell carcinoma and response to treatment. J Clin Oncol 2004;22:900–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bienert, M., McCook, B., Carr, B.I. et al. 90Y microsphere treatment of unresectable liver metastases: changes in 18F-FDG uptake and tumour size on PET/CT. Eur J Nucl Med Mol Imaging 32, 778–787 (2005). https://doi.org/10.1007/s00259-004-1752-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-004-1752-1