Abstract
Purpose
Radioimmunotherapy (RIT) for relapsed non-Hodgkin’s lymphoma is emerging as a promising treatment strategy. Myelosuppression is the dose-limiting toxicity and may be particularly problematic in patients heavily pretreated with chemotherapy. Reliable dosimetry is likely to minimise toxicity and improve treatment efficacy, and the aim of this study was to elucidate the complex problems of dosimetry of RIT by using an integrated SPECT/CT system.
Methods
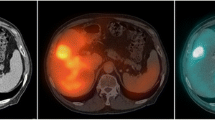
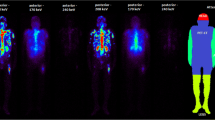
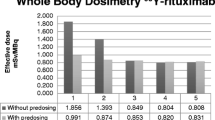
As a part of a clinical trial of 131I-anti-CD20 rituximab RIT of non-Hodgkin’s lymphoma, we employed a patient-specific prospective dosimetry method utilising the whole-body effective half-life of antibody and the patient’s ideal weight to calculate the administered activity for RIT corresponding to a prescribed radiation absorbed dose of 0.75 Gy to the whole body. A novel technique of quantitation of bone marrow uptake with hybrid SPECT/CT imaging was developed to validate this methodology by using post-RIT extended imaging and data collection.
Results
A strong, statistically significant correlation (p=0.001) between whole-body effective half-life of antibody and effective marrow half-life was demonstrated. Furthermore, it was found that bone marrow activity concentration was proportional to administered activity per unit weight, height or body surface area (p<0.001).
Conclusion
The results of this study show the proposed whole-body dosimetry method to be valid and clinically applicable for safe, effective RIT.







Similar content being viewed by others
References
Turner JH, Martindale AA, Boucek J, Claringbold PG, Leahy MF. 131I-Anti CD20 radioimmunotherapy of relapsed or refractory non-Hodgkin’s lymphoma: a phase II clinical trial of a nonmyeloablative dose regimen of chimeric rituximab radiolabeled in a hospital. Cancer Biother Radiopharm 2003;18:513–24.
Wahl RL. Iodine-131 anti-B1 antibody therapy in non-Hodgkin’s lymphoma: dosimetry and clinical implications. J Nucl Med 1998;39(suppl):1S–9S.
Wahl RL, Kroll S, Zasadny KR. Patient-specific whole-body dosimetry: principles and a simplified method for clinical implementation. J Nucl Med 1998;39(suppl):9S–16S.
Wiseman GA, Leigh B, Lamonica D, Kornmehl E, Spies SM, Silverman DHS, et al. Radiation dosimetry results for Zevalin radioimmunotherapy of rituximab-refractory non-Hodgkin lymphoma. Cancer 2002;94:1349–57.
DeNardo SJ, DeNardo GL, Kukis D, Shen S, Kroger L, DeNardo DA, et al. 67Cu-2IT-BAT-Lym-1 pharmacokinetics, radiation dosimetry, toxicity and tumour regression in patients with lymphoma. J Nucl Med 1999;40:303–10
Turner JH, Martindale AA, Sorby P, Hetherington EL, Fleay R, Hoffman R, et al. Samarium-153 EDTMP therapy of disseminated skeletal metastasis. Eur J Nucl Med 1989;15:784–95.
Rizzieri DA, Akabani G, Zalutsky M, Coleman RE, Metzler SD, Bowsher JE, et al. Phase 1 trial study of 131I-labeled chimeric 81C6 monoclonal antibody for the treatment of patients with non-Hodgkin lymphoma. Blood 2004;104:642–8.
Sgouros G. Bone marrow dosimetry for radioimmunotherapy: theoretical considerations. J Nucl Med 1993;34:689–94.
Macey DJ, DeNardo SJ, DeNardo GL, DeNardo DA, Shen S. Estimation of radiation absorbed doses to the red marrow in radioimmunotherapy. Clin Nucl Med 1995;20:117–25.
Stabin MG. MIRDOSE: personal computer software for internal dose assessment in nuclear medicine. J Nucl Med 1996;37:538–46.
Bouchet LG, Bolch WE, Howell RW, Rao DV. S values for radionuclides localized within the skeleton. J Nucl Med 2000;41:189–212.
Bolch WE, Patton PW, Rajon DA, Shah AP, Jokisch DW, Inglis BA. Considerations of marrow cellularity in 3-dimensional dosimetric models of the trabecular skeleton. J Nucl Med 2002;43:97–108.
Stabin MG, Eckerman KF, Bolch WE, Bouchet LG, Patton PW. Evolution and status of bone and marrow dose models. Cancer Biother Radiopharm 2002;17:427–33.
Coffey JL, Watson EE. Calculating dose from remaining body activity: a comparison of two methods. Med Phys 1979;6:307–8.
Wiseman GA, Kornmehl E, Leigh B, Erwin WD, Podoloff DA, Spies S, et al. Radiation dosimetry results and safety correlations from 90Y-ibritumomab tiuxetan radioimmunotherapy for relapsed or refractory non-Hodgkin’s lymphoma: combined data from four clinical trials. J Nucl Med 2003;44:465–74.
Snyder WS et al. Report of the task group on reference man. Pergamon Press, ICRP report No.23. Oxford, UK: International Commission on Radiological Protection; 1974.
Juweid ME. Radioimmunotherapy of B-cell non-Hodgkin’s lymphoma: from clinical trials to clinical practice. J Nucl Med 2002;43:1507–29.
ICRP 70, Basic anatomical and physiological data for use in radiological protection: the skeleton. ICRP publication 70. Oxford, UK: International Commission on Radiological Protection; 1995.
Patton JA, Delbeke D, Sandler MP. Image fusion using an integrated, dual-head coincidence camera with X-ray tube-based attenuation maps. J Nucl Med 2000;41:1364–68.
Knoos T, Nilsson M, Ahlgren L. A method for conversion of Hounsfield number to electron density and prediction of macroscopic pair production cross-sections. Radiother Oncol 1986;5:337–45.
Duck FA. Physical properties of tissue: a comprehensive reference book. New York: Academic Press; 1990.
Acknowledgements
The technical assistance and advice of Christopher Jones and the data evaluation and statistical analysis by Kerryn Butler-Henderson are gratefully acknowledged. This study was supported in part by Fremantle Hospital Nuclear Medicine Research Fund and the loan of an eNTegra workstation from GE Medical Systems. The phase II clinical trial of 131I-rituximab in NHL is a physician-sponsored study and no commercial funding support has been solicited or received.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
Calibration of SPECT/CT scanner
For quantitation of 131I-rituximab uptake a SPECT/CT hybrid scanner (Millennium VG HawkEye, GE Medical Systems, WI, USA) was used [19]. To accurately quantify organ uptake of 131I using SPECT/CT imaging, a calibration factor must first be obtained to convert SPECT image count density (or count rate in the pixel or region) to the 131I tracer activity concentration for patient images, and thus in the organs, by extrapolation and summation.
For calibration, a standard reference phantom (PET/SPECT Performance Phantom 76-823, Nuclear Associates, NY, USA) with a “Linearity/Uniformity Insert” and a “Hot Lesion Insert” was filled with water and 403 MBq of 131I. The solution was mixed thoroughly to ensure uniform distribution of activity. The phantom was then scanned at 15 time points, each time point corresponding to a different activity concentration of 131I. The acquisition was performed using a standard 131I tumour imaging protocol comprising 90 projections (45 projections for each detector), at 50 s for every projection. The SPECT matrix was 128×128 and the pixel size, 3.45 mm. The CT component of acquisition used a full-circle rotation, 40 slices, with 140 kVp voltage and 2 mA current. Each scan was reconstructed using standard automatic iterative OSEM reconstruction on a nuclear medicine workstation (eNTegra v2.016, GE Medical Systems, WI, USA). All SPECT images were attenuation corrected by means of CT-based attenuation correction.
All SPECT and corresponding CT scans were reconstructed in 128 slices and then exported into Interfile image format. The number of counts was quantified in IDL (Research Systems, CO, USA) programming environment using several programs developed in-house. The calibration strategy comprised placing an ROI where counts or count density is not affected by partial volume effects, which may compromise application of calibration factors. The exclusion of partial volume effects in vitro was achieved by placing ROIs, where counting was performed, inside the phantom cylinder and ensuring that pixels near the walls of the phantom were not included by using an automated computer program written in IDL. The program scanned through the dataset on a slice-by-slice basis. First, the centre of mass in a slice was found and then a circle centred on the centre of mass was drawn in that slice to delineate the ROI. The circle had a diameter which was smaller than the physical diameter of the phantom by at least of one full-width at half-maximum, which was approximately 18 mm. The calibration VOI comprised all ROIs in all relevant slices. Such established count densities in VOIs were then plotted for 15 different activity concentrations. The calibration parameters were established by fitting a linear function onto measured data. The statistical errors were assessed using conventional parametric methods on goodness of fit and confidence intervals.
Calibration of linear function for computation of activity (kBq) in a pixel
where Apix is activity in a pixel in kBq, C is the number of counts in a pixel per second and a and b are calibration parameters. It should be noted that this is independent of pixel size. Calibration parameters as computed were a=8.0789±0.0579 kBq·s and b=0.0045±0.2109 kBq.
The SPECT/CT calibration is performed using a similar technique to that employed for SUV calibration of PET scanners. It is based on an ideal case of infinite source, that is, as if partial volume effect did not exist. Every implementation of such parameters thus may need to estimate a quantitation error. Errors will be dependent upon the volume and geometry of VOI and sources surrounding the VOI.
Appendix 2
Calculation of active marrow uptake
Uptake of 131I-rituximab in the bone marrow was estimated using marrow VOIs. It is reasonable to assume that the VOI drawn on CT consists of a mixture of cortical bone and bone marrow only. We can then represent the fraction of bone in the VOI as p and the fraction of marrow in the VOI as q, while M is the average intensity of the VOI on the CT image expressed in CT numbers. The mean CT number of bone tissue is 3,000 and mean CT numbers for red marrow and yellow marrow are 1,008 and 965, respectively [20, 21]. Thus the mean CT number of a mixture of yellow and red marrow will be dependent upon the ratio of yellow to red marrow. In practice, the bone marrow density and its CT number are dependent upon the fraction of yellow marrow, which will vary depending upon the location of bone marrow and the age of the patient. We used the values published in ICRP 23 [16] and ICRP 70 [18]. Active marrow volume fraction R is 0.7 (spinal), 0.48 (pelvic) and 0.25 (femoral), and the respective S numbers for spinal, pelvic and femoral marrow compartments are 995, 986 and 976.
Relationship between correction factors p and q
Computation of bone tissue correction factor q
Bone tissue fraction can then be expressed.
Formula for correcting activity concentration for bone tissue and yellow marrow volume
The activity concentration in active marrow (ARM) can then be obtained from activity concentration in bone marrow VOI (ACT_VOI) by correcting by factor q for supporting bone tissue volume and by factor R for yellow marrow volume.
Rights and permissions
About this article
Cite this article
Boucek, J.A., Turner, J.H. Validation of prospective whole-body bone marrow dosimetry by SPECT/CT multimodality imaging in 131I-anti-CD20 rituximab radioimmunotherapy of non-Hodgkin’s lymphoma. Eur J Nucl Med Mol Imaging 32, 458–469 (2005). https://doi.org/10.1007/s00259-004-1692-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-004-1692-9