Abstract
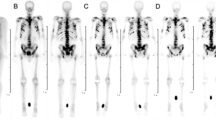
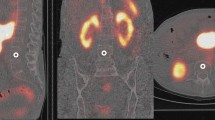
In high-activity rhenium-186 hydroxyethylidene diphosphonate (186Re-HEDP) treatment of bone metastatic disease from prostate cancer the dose-limiting factor is haematological toxicity. In this study, we examined the correlation of the injected activity and the whole-body absorbed dose with treatment toxicity and response. Since the best response is likely to be related to the maximum possible injected activity limited by the whole-body absorbed dose, the relationship between pre-therapy biochemical and physiological parameters and the whole-body absorbed dose was studied to derive an algorithm to predict the whole-body absorbed dose prior to injection of the radionuclide. The whole-body retention of radioactivity was measured at several time points after injection in a cohort of patients receiving activities ranging between 2,468 MBq and 5,497 MBq. The whole-body absorbed dose was calculated by fitting a sequential series of exponential phases to the whole-body time-activity data and by integrating this fit over time to obtain the whole-body cumulated activity. This was then converted to absorbed dose using the Medical Internal Radiation Dose (MIRD) committee methodology. Treatment toxicity was estimated by the relative decrease in white cell (WC) and platelet (Plt) counts after the injection of the radionuclide, and by their absolute nadir values. The criterion for a treatment response was a 50% or greater decrease in prostate-specific antigen (PSA) value lasting for 4 weeks. Alkaline phosphatase (AlkPh), chromium-51 ethylene diamine tetra-acetate (51Cr-EDTA) clearance rate and weight were measured before injection of the radionuclide. The whole-body absorbed dose showed a significant correlation with WC and Plt toxicity (P=0.005 and 0.003 for the relative decrease and P=0.006 and 0.003 for the nadir values of WC and Plt counts respectively) in a multivariate analysis which included injected activity, whole-body absorbed dose, pre-treatment WC and Plt baseline counts, PSA and AlkPh values, and the pre-treatment Soloway score. The injected activity did not show any correlation with WC or Plt toxicity, but it did correlate with PSA response (P=0.005). These results suggest that the administration of higher activities would be likely to generate a better response, but that the quantity of activity that can be administered is limited by the whole-body absorbed dose. We have derived and evaluated a model that estimates the whole-body absorbed dose on an individual patient basis prior to injection. This model uses the level of injected activity and pre-injection measurements of AlkPh, weight and 51Cr-EDTA clearance. It gave good estimates of the whole-body absorbed dose, with an average difference between predicted and measured values of 15%. Furthermore, the whole-body absorbed dose predicted using this algorithm correlated with treatment toxicity. It could therefore be used to administer levels of activity on a patient-specific basis, which would help in the optimisation of targeted radionuclide therapy. We believe that algorithms of this kind, which use pre-injection biochemical and physiological measurements, could assist in the design of escalation trials based on a toxicity-limiting whole-body absorbed dose, rather than using the more conventional activity escalation approach.







Similar content being viewed by others
References
O'Sullivan JM, McCready VR, Flux G, Norman AR, Buffa FM, Chittenden S, Guy M, Pomeroy K, Cook G, Gadd J, Treleaven J, Al Deen A, Horwich A, Huddart RA, Dearnaley DP. High activity rhenium-186 HEDP with autologous peripheral blood stem cell rescue: a phase I study in progressive hormone refractory prostate cancer metastatic to bone. Br J Cancer 2002; 86:1715–1720.
Sgouros G. Bone-marrow dosimetry for radioimmunotherapy—theoretical considerations. J Nucl Med 1993; 34:689–694.
Juweid M, Sharkey RM, Siegel JA, Behr T, Goldenberg DM. Estimates of red marrow dose by sacral scintigraphy in radioimmunotherapy patients having non-Hodgkin's lymphoma and diffuse bone marrow uptake. Cancer Res 1995; 55:5827s–5831s.
Siegel JA, Lee RE, Pawlyk DA, Horowitz JA, Sharkey RM, Goldenberg DM. Sacral scintigraphy for bone marrow dosimetry in radioimmunotherapy. Int J Rad Appl Instrum B 1989; 16:553–559.
Samaratunga RC, Thomas SR, Hinnefeld JD, Von Kuster LC, Hyams DM, Moulton JS, Sperling MI, Maxon HR. A Monte Carlo simulation model for radiation dose to metastatic skeletal tumor from rhenium-186(Sn)-HEDP. J Nucl Med 1995; 36:336–350.
van Aswegen A, Roodt A, Marais J, Botha JM, Naude H, Lotter MG, Goedhals L, Doman MJ, Otto AC. Radiation dose estimates of186Re-hydroxyethylidene diphosphonate for palliation of metastatic osseous lesions: an animal model study. Nucl Med Commun 1997; 18:582–588.
Limouris G, Shukla SK, Manetou A, Kouvaris I, Plataniotis G, Triantafyllou N, Rigas AV, Vlahos L. Rhenium-186-HEDP palliative treatment in disseminated bone metastases due to prostate cancer. Anticancer Res 1997; 17:1699–1704.
Graham MC, Scher HI, Liu GB, Yeh SD, Curley T, Daghighian F, Goldsmith SJ, Larson SM. Rhenium-186-labeled hydroxyethylidene diphosphonate dosimetry and dosing guidelines for the palliation of skeletal metastases from androgen-independent prostate cancer. Clin Cancer Res 1999; 5:1307–1318.
Israel O, Keidar Z, Rubinov R, Iosilevski G, Frenkel A, Kuten A, Betman L, Kolodny GM, Yarnitsky D, Front D. Quantitative bone single-photon emission computed tomography for prediction of pain relief in metastatic bone disease treated with rhenium-186 etidronate. J Clin Oncol 2000; 18:2747–2754.
Trotti A, Byhardt R, Stetz J, Gwede C, Corn B, Fu K, Gunderson L, McCormick B, Morrisintegral M, Rich T, Shipley W. Common toxicity criteria: version 2.0. An improved reference for grading the acute effects of cancer treatment: impact on radiotherapy. Int J Radiat Oncol Biol Phys 2000; 47:13–47.
Siegel JA, Thomas SR, Stubbs JB, Stabin MG, Hays MT, Koral KF, Robertson JS, Howell RW, Wessels BW, Fisher DR, Weber DA, Brill AB. MIRD pamphlet no. 16: techniques for quantitative radiopharmaceutical biodistribution data acquisition and analysis for use in human radiation dose estimates. J Nucl Med 1999; 40:37S–61S.
Toohey RE, Stabin MG, Watson EE. The AAPM/RSNA physics tutorial for residents: internal radiation dosimetry: principles and applications. Radiographics 2000; 20:533–546.
Flux GD, Guy MJ, Beddows R, Pryor M, Flower MA. Estimation and implications of random errors in whole-body dosimetry for targeted radionuclide therapy. Phys Med Biol 2002; 47:3211–3223.
Soloway MS, Hardeman SW, Hickey D, Raymond J, Todd B, Soloway S, Moinuddin M. Stratification of patients with metastatic prostate cancer based on extent of disease on initial bone scan. Cancer 1988; 61:195–202.
Bubley GJ, Carducci M, Dahut W, Dawson N, Daliani D, Eisenberger M, Figg WD, Freidlin B, Halabi S, Hudes G, Hussain M, Kaplan R, Myers C, Oh W, Petrylak DP, Reed E, Roth B, Sartor O, Scher H, Simons J, Sinibaldi V, Small EJ, Smith MR, Trump DL, Wilding G. Eligibility and response guidelines for phase II clinical trials in androgen-independent prostate cancer: recommendations from the Prostate-Specific Antigen Working Group. J Clin Oncol 1999; 17:3461–3467.
Berruti A, Piovesan A, Torta M, Raucci CA, Gorzegno G, Paccotti P, Dogliotti L, Angeli A. Biochemical evaluation of bone turnover in cancer patients with bone metastases: relationship with radiograph appearances and disease extension. Br J Cancer 1996; 73:1581–1587.
Fossa SD, Dearnaley DP, Law M, Gad J, Newling DW, Tveter K. Prognostic factors in hormone-resistant progressing cancer of the prostate. Ann Oncol 1992; 3:361–366.
Dudewicz EJ, Mishra SN. Modern mathematical statistics. New York: Wiley, 1988.
Matthews DE, Farewell VT. Using and understanding medical statistics. Basel: Karger, 1996.
Press WH, Teukolsky SA, Vellering WT, Flannery BP. Numerical recipes in C. Cambridge: Cambridge University Press, 1993.
Acknowledgements
This work was undertaken in The Institute of Cancer Research and The Royal Marsden NHS Trust and was funded by an NIH grant (with ref. numb. 1 R21 CA86784–01A1) and by the NHS Executive. The views expressed in this publication are those of the authors and not necessarily those of the NIH or NHS Executive. The Institute of Cancer Research Physics Department, The Royal Marsden Nuclear Medicine Department and the Bob Champion Cancer Trust supported this work. The authors would like to thank Dr. Maggie Flower for her useful comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Buffa, F.M., Flux, G.D., Guy, M.J. et al. A model-based method for the prediction of whole-body absorbed dose and bone marrow toxicity for 186Re-HEDP treatment of skeletal metastases from prostate cancer. Eur J Nucl Med Mol Imaging 30, 1114–1124 (2003). https://doi.org/10.1007/s00259-003-1197-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-003-1197-y