Abstract
Anthracyclines, e.g., doxorubicin (DOX), and anthracenediones, e.g., mitoxantrone (MTX), are drugs used in the chemotherapy of several cancer types, including solid and non-solid malignancies such as breast cancer, leukemia, lymphomas, and sarcomas. Although they are effective in tumor therapy, treatment with these two drugs may lead to side effects such as arrhythmia and heart failure. At the same clinically equivalent dose, MTX causes slightly reduced cardiotoxicity compared with DOX. These drugs interact with iron to generate reactive oxygen species (ROS), target topoisomerase 2 (Top2), and impair mitochondria. These are some of the mechanisms through which these drugs induce late cardiomyopathy. In this review, we compare the cardiotoxicities of these two chemotherapeutic drugs, DOX and MTX. As described here, even though they share similarities in their modes of toxicant action, DOX and MTX seem to differ in a key aspect. DOX is a more redox-interfering drug, while MTX induces energy imbalance. In addition, DOX toxicity can be explained by underlying mechanisms that include targeting of Top2 beta, mitochondrial impairment, and increases in ROS generation. These modes of action have not yet been demonstrated for MTX, and this knowledge gap needs to be filled.
Similar content being viewed by others
Introduction
Anthracyclines such as doxorubicin (DOX), epirubicin, and daunorubicin are important chemotherapeutic agents used in the treatment of several types of cancer, including solid and non-solid malignancies such as breast cancer, leukemia, lymphomas, and sarcomas. Daunorubicin was the first anthracycline isolated in the 1960s. It was initially obtained from the soil bacterium Streptomyces peucetius (Di Marco et al. 1964). There are two hypotheses explaining how anthracyclines kill cancer cells. They include targeting of DNA topoisomerases (Vejpongsa and Yeh 2014a) and generation of reactive oxygen species (ROS) through interaction of anthracyclines with iron (Stěrba et al. 2013). Anthracyclines that are widely used in several chemotherapeutic regimens increased the survival rates for pediatric cancer in excess of 75 % (Sant et al. 2009). Although they are effective in cancer treatment, side effects such as arrhythmia and heart failure were reported for anthracyclines (Tan et al. 1967; Von Hoff et al. 1977). In a survey of 1807 cancer survivors who had been treated with anthracyclines and followed for 7 years, 33 % died of heart disease, and 51 % died of cancer (Ning et al. 2012). Anthracycline treatment is the primary cause of chemotherapy-induced cardiotoxicity (Vejpongsa and Yeh 2014b). It is estimated that about 26 % of patients will develop DOX-related congestive heart failure at a cumulative conventional DOX dose of 550 mg/m2 (Senkus and Jassem 2011).
The mechanisms by which anthracyclines induce cardiac toxicity are not fully understood. Energy imbalance induced by mitochondrial dysfunction (Green and Leeuwenburgh 2002) and ROS generation (Iarussi et al. 2001; Neilan et al. 2007; Wallace 2003) are among possible modes of action. Recently, Vejpongsa and Yeh (2014a) discussed the role of DNA topoisomerase 2β (Top2β) in DOX-mediated cardiotoxicity. Mitochondrial topoisomerase 1 (mtTop1) also appears to be a possible target of anthracycline-induced cardiac cell death (Khiati et al. 2014).
To reduce the anthracycline-related cardiotoxicity while maintaining the desired antineoplastic activity, anthracenedione compounds were developed, including the chemotherapeutic agents mitoxantrone (MTX), ametantrone, and pixantrone (Cheng and Zee-Cheng 1983; De Isabella et al. 1995). MTX inhibits both DNA replication and DNA-dependent RNA synthesis. It also intercalates into DNA, thereby decreasing the protein synthesis and cell proliferation (Faulds et al. 1991). Owing to its small size, MTX can easily cross the blood–brain barrier and interact with cells in the central nervous system; it also has immunosuppressant activity. Owing to these properties, MTX has also been used against neurological disorders such as multiple sclerosis (MS) (Fenu et al. 2015; Millefiorini et al. 1997).
Rossato et al. (2013a, b, 2014) demonstrated the relation between MTX-induced cardiotoxicity and mitochondrial impairment in in vitro (H9c2 cardiomyoblasts) and in vivo (male Wistar rats) studies. These studies pointed to the electron transport chain (ETC) as the endpoint of toxicity induced by MTX and its metabolites and revealed the importance of cumulative exposure. Although experimental (Rossato et al. 2013a, 2014) and clinical studies (Dores-Sousa et al. 2015; Joyce et al. 2013) highlighted the MTX-induced cardiac toxicity, little is known about the mechanisms involved in this process and whether anthracenediones induce the cardiac damage via a mechanism similar to that of anthracyclines. In this review, we try to elucidate the mechanisms of DOX- and MTX-induced cardiotoxicity.
ROS generation, iron accumulation, and mitochondrial dysfunction
Mitochondrial respiration accounts for about 90 % of cellular oxygen consumption, and therefore, the ETC in mitochondria is mainly responsible for physiological ROS production (Papa 1996). It is well known that under physiological conditions, 1–5 % of the oxygen consumed by mitochondria is converted to ROS (Halliwell 2009; Halliwell and Gutteridge 1984).
ETC complexes I, III, and IV in the mitochondrial membrane guide electrons through reactions to create the proton motive force that drives the ATP synthesis by complex V (ATP synthase) (Fig. 1). It is plausible to believe that the superoxide anion radical (O ∙−2 ) is derived from intermediates of the normal catalytic cycles of complexes I and III (Dröse and Brandt 2012). There are three well-described sites where superoxide anion radicals are generated, the ubiquinone-binding sites in complexes I and III and the flavin prosthetic group in complex I. In addition, Wosniak et al. (2009) demonstrated the existence of a crosstalk between mitochondria and NADPH oxidases. Mitochondrial ROS activate O ∙−2 and hydrogen peroxide (H2O2) production by NADPH oxidases, which, in turn, stimulate mitochondrial ROS formation. The O ∙−2 generation by the respiratory chain is a highly regulated process in which ROS can function both adversely and beneficially (Figueira et al. 2013). Mitochondrial ROS are demonstrated to take part in cellular signaling pathways as messenger molecules (Murphy et al. 2011). The formation of ROS should be a highly controlled process since their excess generation can be extremely harmful to the cell. The majority of the O ∙−2 formed inside mitochondria does not pass through the membranes, indicating that the damage may be largely contained within the mitochondria (Giulivi et al. 1995).
Reactive oxygen species (ROS) generation in mitochondria. Electron transport chain complexes I, III, and IV in the mitochondrial membrane guide electrons through reactions to create a proton motive force that drives ATP synthesis by complex V (ATP synthase). There are three well-described sites where the superoxide anion radical (O ∙−2 ) is generated, the ubiquinone-binding sites in complexes I and III and the flavin prosthetic group in complex I. O ∙−2 can generate other ROS such as hydrogen peroxide (H2O2) and the hydroxyl radical (OH∙) by reacting with iron. Oxidative stress is induced in response to a decreased level of antioxidant enzymes [superoxide dismutases (CuZnSOD and MnSOD), catalase (CAT), and glutathione peroxidase (GPx)] and increased production of ROS. GSH, glutathione; GSSG, glutathione disulfide
The high level of energy required by the heart to keep us alive comes at a cost, such as the generation of large amounts of oxygen and nitrogen metabolites (Costa et al. 2011). To meet the demand for ATP synthesis via oxidative metabolism, cardiac myocytes have the highest volume density of mitochondria and produce ROS through ETC (Tsutsui et al. 2008). In addition, cardiac tissue has less antioxidant enzymes compared with liver and kidney tissues (Halliwell and Gutteridge 1984). Therefore, oxidative stress, which is known to cause a disturbance in the pro-oxidant/antioxidant balance, is induced in response to the decreased levels of antioxidant enzymes, including copper–zinc and manganese superoxide dismutases (SODs), catalase (CAT), and glutathione peroxidase, and the increased production of ROS and reactive nitrogen species (RNS) or both (Costa et al. 2013; Sies 1997). Mitochondria also function as the crossroads for autophagic, apoptotic, and necrotic pathways. Under mild stress conditions, autophagy is induced to degrade and recycle cytoplasmic components. With increasing stress levels, apoptosis occurs because of cytochrome c release from mitochondria. Under extreme stress, the mitochondrial permeability transition occurs in all mitochondria, and the intracellular supply of ATP is exhausted, leading to necrosis (Nishida and Otsu 2008; Zhang et al. 2009).
It is believed that the main pathway of anthracycline cardiotoxicity is the production of semiquinone metabolites during drug metabolism, which induce O ∙−2 formation (Carvalho et al. 2014). O ∙−2 is a primary radical that can generate other ROS, such as H2O2 and the hydroxyl radical (OH∙)(Ide et al. 2000). As demonstrated by Vásquez-Vivar et al. (1998), binding of DOX to the endothelial nitric oxide synthase (eNOS) reductase domain resulted in O ∙−2 generation. DOX can be reduced to the semiquinone radical by nitric oxide synthases and NADPH oxidase (Fig. 2a). This semiquinone radical undergoes further transformation to the C-7 free radical, which can interact with molecular oxygen and other intracellular molecules, most notably, lipids. The electron donors NADPH and FAD/FMN are oxidized by NADPH oxidase and eNOS, respectively (Octavia et al. 2012). The influence of NADPH oxidase on DOX cardiotoxicity was confirmed in a study that correlated the development of DOX-induced cardiotoxicity with polymorphisms of the NADPH oxidase complex in patients with non-Hodgkin’s lymphoma (Wojnowski et al. 2005).
a Doxorubicin (DOX) can be reduced to the semiquinone radical by nitric oxide synthases (NOSs) and NADPH oxidase. b Mitoxantrone (MTX) is oxidized through a cytochrome P450-mediated reaction generating quinone or quinonediimine intermediates with intracellular nucleophilic components. MTX is also oxidized at a high H2O2 concentration by human myeloperoxidase (MPO)
MTX contains a quinone functional group in its structure (Fig. 2b). Furthermore, similar to DOX, it undergoes activation by phase I metabolic enzymes (Kharasch and Novak 1983; Mimnaugh et al. 1982). Duthie and Grant (1989) demonstrated that in human hepatoma HepG2 cells, the cytotoxic effect of MTX was not mediated by the one-electron reduction oxidative stress mechanism. In addition, inhibition of antioxidant enzymes such as CAT and glutathione reductase did not affect the MXT-induced cell viability loss, suggesting that ROS are not involved in the process (Duthie and Grant 1989).
Unlike DOX, MTX is resistant to reductive enzymatic activation but is subject to oxidative enzymatic action (Basra et al. 1985; Kharasch and Novak 1983). MTX is oxidized by a cytochrome P450-mediated reaction generating quinone or quinonediimine intermediates with intracellular nucleophilic components in HepG2 and MCF-7 cells (Duthie and Grant 1989; Li et al. 1995; Mewes et al. 1993). MTX is also oxidized at a high H2O2 concentration by human myeloperoxidase (Panousis et al. 1994) (Fig. 2b). However, unlike DOX, MTX has a weaker capacity to enter in futile redox cycling (Costa et al. 2013). In fact, both have the ability to block the ETC, while MTX has demonstrated a greater capacity to induce ATP depletion (Cini-Neri and Neri 1986). Rossato et al. (2013b) observed mild oxidative stress after MTX treatment in rat cardiomyoblasts (H9c2) and suggested that the ROS increase as a consequence of the redox cycle is secondary to the energy imbalance, a more dramatic and earlier event. The same research group observed that the ETC complex activities were affected at 2- and 48-day time points after MTX treatment cycles in rats. As a consequence, the ATP generation in heart mitochondria decreased (Rossato et al. 2014). These results are in agreement with those obtained in rats treated with daunorubicin, which demonstrated an increase in complex IV and V protein expression and a decrease in complex I activity and expression (Stěrba et al. 2011).
Anthracyclines can also form complexes with iron, producing ROS via a redox cycle (Link et al. 1996). Heart cell mitochondria were previously identified as the major site of iron–anthracycline interaction. In isolated rat cardiomyocytes, DOX was concentrated in mitochondria, inducing increases in mitochondrial iron and cellular ROS levels (Link et al. 1996). According to Ichikawa et al. (2014), overexpression of ABCB8, a mitochondrial iron-export protein, in vivo and in vitro protected against DOX-induced cardiomyopathy and reduced the DOX-induced accumulation of free iron and ROS in mitochondria. At the mitochondrial level, DOX significantly reduced the mRNA and protein levels of ABCB8 and decreased or did not affect the levels of the import protein, mitoferrin 2, which regulates mitochondrial iron homeostasis both in vitro and in vivo (Ichikawa et al. 2014) (Fig. 3a).
a At the mitochondrial level, doxorubicin (DOX) significantly reduces the mRNA and protein levels of ABCB8, a mitochondrial iron-export protein, and either decreases or does not affect the levels of the import protein, mitoferrin 2 (Mfrn-2), a regulator of mitochondrial iron homeostasis, in vitro and in vivo. b The ABCB1 gene can confer a different susceptibility pattern to mitoxantrone (MTX)-induced cardiotoxicity. ABCB1 is also involved in the mitochondrial iron transport, and its involvement in the MTX-mediated cardiotoxicity cannot be ruled out
Myocardial oxidative damage caused by iron-mediated ROS formation has been suggested as a potential mechanism; however, this hypothesis has been challenged by reports showing that several iron chelators failed to reverse cardiotoxic effects of DOX (Miranda et al. 2003; Panjrath et al. 2007; Rao et al. 2011; Šimůnek et al. 2009).
As demonstrated by Cavalcante et al. (2013), MTX has a high affinity for Fe+3 and can be degraded by the Fenton reaction. Herman et al. (1997) showed that MTX could form a 2:1 complex with Fe+3. The same study reported that in spontaneously hypertensive rats (SHR) treated with DOX (1 mg/kg) or MTX (0.5 mg/kg), no significant difference was observed in the severity of the myocardium lesions induced by these drugs. However, the mitochondrial alterations induced by MTX in these animals were much more severe than those induced by DOX (Herman et al. 1997). Congestive heart failure in patients with MS is considered a dose-dependent and delayed complication of MTX treatment at a dose level above the cumulative dose of 100 mg/m2, especially in patients with additional cardiac risk factors. However, myocardial dysfunction could occur at concentrations below 100 mg/m2, challenging this security threshold (Cotte et al. 2009). The authors further suggested that a single nucleotide polymorphism (SNP) in the ABCB1 gene could confer different susceptibility patterns to MTX-induced cardiotoxicity (Cotte et al. 2009). It is well known that differences in P-glycoprotein (encoded by ABCB1) confer different drug resistance patterns to cancer cells. In vitro cytotoxicity studies demonstrated that leukemic cells from patients carrying the polymorphisms 1236T/T and 2677T/T in the ABCB1 gene were significantly more susceptible to MTX than those with other genotypes (Gréen et al. 2012). P-glycoprotein is also involved in mitochondrial iron transport (Richardson and Ponka 1997), and therefore, its involvement in the MTX-mediated cardiotoxicity cannot be ruled out (Fig. 3b).
Zhao et al. (2014) recently demonstrated that several mitochondrial proteins in mice, including those associated with the citric acid cycle and ETC, formed an adduct with 4-hydroxy-2-nonenal (HNE), which is a toxic sub-product of lipid peroxidation, decreasing enzymatic activity of mitochondrial proteins. In addition, treatment with Mn+3 meso-tetrakis (N-n-butoxyethylpyridinium-2-yl)porphyrin, a SOD mimic, abrogated (or protected against) the DOX-induced HNE–protein adduct formation. The authors concluded that the free radical-mediated alteration of energy metabolism is an important mechanism of DOX-induced cardiac injury and suggested that metabolic intervention may represent a novel approach to prevent cardiac injury after chemotherapy (Zhao et al. 2014). However, antioxidant supplementation had a limited protective effect against the DOX-induced cardiotoxicity in both animals and human clinical studies (Ferreira et al. 2008; Šimůnek et al. 2009). Dexrazoxane (ICRF-187) decreased mitochondrial iron levels and reversed the DOX-induced cardiac damage. It is considered one of the most effective derivatives used clinically to prevent the anthracycline-induced cardiomyopathy. Co-administration of dexrazoxane with an anthracycline has been shown to improve the survival and to minimize the cardiac damage in a variety of animal models (Herman et al. 1988). Other iron chelators such as deferoxamine (DFO) and defarasirox have been investigated in vitro and in vivo, with variable findings. However, none of these compounds, despite being stronger chelators and/or antioxidants, have surpassed or even matched the effectiveness of dexrazoxane against chronic anthracycline-induced cardiotoxicity (Hasinoff et al. 2003; Stěrba et al. 2013). The failure of DFO to chelate mitochondrial iron is consistent with its poor mitochondrial permeability (Elihu et al. 1998; Ichikawa et al. 2014). These findings raise questions regarding how dexrazoxane prevents anthracycline cardiotoxicity, whether this is done through iron chelation only, and whether dexrazoxane can prevent the MTX-induced cardiotoxicity.
Shipp et al. (1993a, b) showed that dexrazoxane significantly reduced the high-dose MTX lethality in mice, facilitating the clinical use of dexrazoxane. The mechanism of cardioprotection postulated by the authors is related to iron chelation because dexrazoxane did not alter the toxicity of the non-chelating MTX analog ametantrone (Shipp et al. 1993a, b). As demonstrated by Herman et al. (2001), pretreatment with dexrazoxane attenuated the severity of MTX-induced myocardial damage in SHR. Furthermore, dexrazoxane augmented the therapeutic efficacy of MTX in experimental autoimmune encephalomyelitis (Weilbach et al. 2004). In this regard, more experimental and clinical studies evaluating the efficacy of co-administration of MTX and dexrazoxane for cancer and neurological disorders are needed to determine whether this combination can improve the symptoms while reducing cardiotoxicity.
Topoisomerase inhibition
DNA topoisomerases are a class of enzymes involved in the topological aspects of DNA replication, transcription, recombination, and chromatin remodeling. These enzymes function by introducing temporary single- or double-strand breaks (DSBs) in the DNA (Champoux 2001). DNA strand breaks are induced by transesterification reactions using the active site tyrosine as a nucleophile that attacks the DNA phosphodiester backbone (Pommier 2013). Human cells have genes encoding six Tops (Top1, mtTop1, Top2α, Top2β, Top3α, and Top3β), whereas bacteria express four Tops (Top I, Top III, gyrase, and Top IV). Quinolone antimicrobial drugs such as norfloxacin, levofloxacin, and gemifloxacin are DNA gyrase and Top IV inhibitors, whereas DOX, MTX, etoposide, and dexrazoxane are Top2α and Top2β inhibitors. This specificity is important for the therapeutic applications of these molecules (Pommier 2013; Pommier et al. 2010). Although development of new molecules for cancer therapy that target Top1 has received increased attention (Pommier 2013), in this review, we focus on Top2α and Top2β since these enzymes are the targets of DOX and MTX.
Top2α and Top2β are nearly 70 % identical in their amino acid sequences but are encoded in humans by genes located on different chromosomes. Top2α is encoded by a gene on chromosome 17, and Top2β is encoded by that on chromosome 3 (Austin et al. 1993).
The mechanism of action of Top inhibitors, which prevent the binding of DNA and the enzyme, revealed another new paradigm of drug action, which is the enzyme poisoning rather than catalytic inhibition (Pommier 2013). DOX binds both DNA and Top2 to form a ternary Top2–DOX–DNA cleavage complex, which triggers the cell death (Capranico and Zunino 1992).Yi et al. (2007) demonstrated that mouse embryonic fibroblasts from Top2β-knockout embryos were resistant to DOX-induced cell death. It has recently been demonstrated that the Top2β enzyme, which is the only Top enzyme expressed in myocytes, is the key molecular mediator in the anthracycline-associated cardiotoxicity (Vejpongsa and Yeh 2014a). Top2 poisons, i.e., drugs that form ternary complexes, such as DOX and MTX, induce γ-H2AX DNA damage signal foci in various cell types, demonstrating the DNA strand break formation (Rogakou et al. 1998; Saffi et al. 2010). Following the generation of a DNA DSB, phosphoinositide 3-like kinases, e.g., ATM, ATR, and DNA-dependent protein kinase, are activated and phosphorylate the Ser139 of histone H2AX (Park et al. 2003). A study conducted by Zhang et al. (2012) that compared Top2β-knockout (Top2βΔ/Δ) mice and Top2β+/+ mice demonstrated that the Top2β+/+ animals treated with DOX showed high levels of expression of genes coding proteins involved in an apoptosis pathway, such as Apaf1, Bax, Fas, and Trp53inp1, a p53-inducible gene, which was 200-fold upregulated. Activation of the DNA damage response in the hearts of the Top2β+/+ mice treated with DOX was confirmed by immunostaining of γ-H2AX, whose intensity was 60 % lower in the Top2βΔ/Δ mice. In addition, the levels of transcripts encoding NADH dehydrogenase 1α subcomplex 3 (NDUFA3), succinate dehydrogenase complex II, subunit A (SDHA), and ATP synthase subunit α (ATP5A1) markedly decreased in the DOX-treated Top2β+/+ cardiomyocytes compared with their levels in the DOX-treated Top2βΔ/Δ cardiomyocytes. This study highlighted the role of Top2β in the DOX-mediated cell death and indicated that the cell death might be due to DNA damage with consequent loss of mitochondrial function (Zhang et al. 2012).
Oxidation of nitrogen bases (8-hydroxydeoxyguanosine) in mitochondrial DNA (mtDNA) of rat hearts, as well as a deletion of about 4 kb in mtDNA of mice hearts, has been detected after subchronic and chronic exposure to DOX (Adachi et al. 1993; Serrano et al. 1999). Besides this, acute DOX exposure was also found to reduce mtDNA synthesis in rat cardiac tissue (Hixon 1981). In rats treated with repeated intravenous injections of a low dose (0.8 mg/kg) of DOX, heart tissue had low activity of cytochrome c oxidase and high activity of citrate synthase. Additionally, expression of respiratory chain subunits encoded by mtDNA decreased, while that nuclear-encoded respiratory chain subunits was preserved (Lebrecht and Walker 2007). Furthermore, Khiati et al. (2014) recently demonstrated that genetic inactivation of mtTop1 in mice led to a reduced mtDNA copy number and increased mtDNA damage in heart tissue following DOX treatment. The mice showed a decrease in O2 consumption because of the mitochondrial defect and an increase in ROS production, as well as enhanced heart muscle damage. The authors concluded that mtTop1, which is conserved across the vertebrates, is critical for cardiac tolerance to DOX and for adaptive responses to cardiotoxicity. They also suggested the potential use of mtTop1 SNP testing to investigate the patient susceptibility to DOX (Khiati et al. 2014). New insights have challenged the concept that DOX cardiotoxicity is a sum of somewhat independent events, indicating that they are all consequences of the interaction among DOX–Top2–DNA. Dexrazoxane, an iron chelator, forms an intricate complex with the ATPase domain of human Top2α and Top2β and prevents anthracyclines from binding to Top2 (Roca and Wang 1994). Therefore, preventing anthracyclines from binding to the Top2–DNA complex might be the mechanism by which dexrazoxane prevents the anthracycline-induced cardiotoxicity (Yi et al. 2007). Consequently, blocking and degrading Top2β should also be considered useful clinical strategies to prevent the anthracycline-induced cardiotoxicity, as recently reported by (Vejpongsa and Yeh 2013).
In the case of MTX, some studies addressed its interaction with Top2β. Wu et al. (2013) determined the high-resolution crystal structures of Top2β cleavage complexes stabilized by MTX. Huang and Lin (2014) demonstrated that this drug formed a weak cleavage complex with Top2β as compared with that formed with Top2α. Top2β downregulation leads to MTX resistance in a leukemia cell line (Hermanson et al. 2013). In another study, an l-methionine-conjugated MTX (MTX-MET) molecule (WRC-213) displayed good cytotoxic potential with less cardiotoxicity compared with that of MTX. WRC-213 induces the comet-tail formation in DNA of fewer cells (indicating less genotoxicity), as well as lower cytotoxicity than MTX in H9c2 cells. The authors suggested that the population-doubling time of H9c2, which is about twofold lower than that of cancer cells, is a determining factor of the less WRC-213 toxicity in cardiac cells (Hsiao et al. 2008). If this hypothesis, however, was true, MTX should have shown less cardiotoxicity as well, which was not observed. Furthermore, in another study from the same research group, 1,4-bis-L/l-methionine-conjugated MTX-induced DNA breaks, cancer cell apoptosis, and revealed antitumor activities comparable to those of MTX. At the same time, the conjugated drug showed more favorable drug resistance profiles and a higher maximum tolerated dose in mice, indicating less toxicity (Lee et al. 2012).
To test the above hypothesis, molecular docking experiments were performed to analyze the interaction mode of selected compounds with the receptor complex Top2β–DNA and MTX or MTX-MET (WRC-213), as well as with Top2α–DNA and MTX or MTX-MET (WRC-213), using the crystal structures of both Top enzymes. The receptor and ligand structures were prepared using AutoDock Tools 1.5.2, while docking simulations were performed with AutoDock4.2 (Morris et al. 2009), granting full flexibility to the ligands. The Lamarckian genetic algorithm was used for the docking with 25 runs, and the remaining parameters were set to their default values. The molecular interaction study of the ligands with the Top enzymes revealed that the lower cardiotoxicity of WRC-213 may result from a change in the binding energy that would lead to a lower affinity to Top2β (ΔG = −3.32 kcal/mol) compared with that of MTX (ΔG = −7.82 kcal/mol). This change in the binding energy is not observed for the Top2α enzyme (Fig. 4). The above results could be partially explained by non-bonded interactions achieved using LIGPLOT (Wallace et al. 1995), which showed that the Top2α–DNA and MTX complex had five hydrogen bonds with DNA bases (DG4, DT12, and DG13) and hydrophobic contacts with Met762 and Ser763. In contrast, the intermolecular interactions of Top2α–DNA and MTX-MET showed six hydrogen bonds and three hydrophobic contacts. The same analysis was performed with Top2β–DNA and MTX and revealed four hydrogen bonds and five hydrophobic contacts versus eight hydrogen bonds and six hydrophobic contacts between Top2β–DNA and MTX-MET. In the case of Top2α–DNA, it seems that the affinity is linked to the number of hydrogen bonds and hydrophobic contacts (Top2α–DNA–MTX, ΔG = −3.53 kcal/mol and Top2α–DNA–MTX-MET, ΔG = −5.88 kcal/mol); however, the same conclusion could not be made for Top2β–DNA. Nevertheless, the affinity and specificity between a ligand and its protein targets depend on directional hydrogen bonds, more specifically, on the distance and angle between the hydrogen donor and acceptor (Caceres et al. 2008; Herman 1997; Morris et al. 2009). The angle could cause an energetic difference in terms of the strength of a hydrogen bond, which can explain the higher affinity between Top2α–DNA and MTX-MET compared with that between Top2α–DNA and MTX.
Molecular docking experiments. The topoisomerase, Top2β and Top2α, tertiary structures are represented as a cartoon, and mitoxantrone (MTX) and MTX-MET (WRC-213) are represented as a stick. In a–d, the crystal structure of Top2β:DNA, associated with MTX (PDB ID: 4G0 V), was used as a template. Top2β is biologically active as a dimer; however, only chain A was used to perform all docking experiments. For all simulations, the 3D-grid dimensions used to define the Top2β active site and to evaluate the scoring function were 28 × 40 × 16, with the spacing of 0.375 Å, and the 3D-grid center was established at 32.723 92.396 51.99. In e–h, the crystal structure of Top2α:DNA (PDB ID: 4FM9) was used as a template. For all simulations, the 3D-grid dimensions used to define the Top2α active site and to evaluate the scoring function were 50 × 50 × 30, with the spacing of 0.375 Å, and the 3D-grid center was established at 32.723 92.396 51.99. a Three-dimensional representations of Top2β–DNA–ligand interactions. Docking simulations for Top2β–DNA–MTX (PDB ID: 4G0 V), showing the crystallographic structure of MTX and the best pose (RMSD: 1.04 Å and ΔG = –7.82 kcal/mol) of the docking protocol (magenta). b LIGPLOT diagram of Top2β amino acids and DNA interacting with MTX. c Three-dimensional representations of Top2β–DNA–MTX-MET achieved by molecular docking (ΔG = –3.32 kcal/mol). The Top2β tertiary structure is represented as a cartoon, and MTX-MET is represented as a stick. d LIGPLOT diagram of Top2β amino acids and DNA interacting with MTX-MET. e Docking simulations for Top2α–DNA–MTX, showing the crystallographic structure of Top2α–DNA and the best pose (ΔG = –3.53 kcal/mol) of the docking protocol. f LIGPLOT diagram of Top2α amino acids and DNA interacting with MTX. g Three-dimensional representations of Top2α–DNA–MTX-MET achieved by molecular docking (ΔG = –5.88 kcal/mol). h LIGPLOT diagram of Top2α amino acids and DNA interacting with MTX-MET. In b, d, f, and h, the ligand bonds are shown in purple, the non-ligand bonds are shown in light brown, and the hydrogen bonds are shown by green dashed lines. Ligand atoms are surrounded by a yellow circle if they are highly accessible and by a brown circle if they are buried. Non-ligand residues in hydrophobic contact with the ligand are presented by red semi-circles with radiating spokes. The figure was prepared using PyMol (www.pymol.org)
It is really a hard task to determine atomic features responsible for selectivity and affinity. Molecular dynamics studies are required in order to unveil and determine the kind of intermolecular forces ruling the selectivity and affinity of MTX and MTX-MET for Top2α–DNA and Top2β–DNA.
Inhibition/overactivation of poly(ADP-ribose) polymerase
Regarding similarities and differences in the mechanisms of action of DOX and MTX, although their clinical aspects are partially the same, the underlying mechanisms seem to differ. Indeed, the MTX-induced cardiotoxicity may have its origin in MTX interference with cardiac energetic metabolism instead of oxidative stress (Alderton et al. 1992; Bachmann et al. 1987; Rossato et al. 2013b). Evidence suggests that the ROS and RNS generated in cardiomyocytes and endothelial cells can induce oxidative DNA damage and consequent activation of the nuclear enzyme poly(ADP-ribose) polymerase 1 (PARP1), the most abundant isoform of the PARP enzyme family (Pacher and Szabó 2007). Energy depletion can be triggered by activating PARP1 since this enzyme consumes NAD+ as its substrate (Satoh and Lindahl 1992).
Poly-ADP-ribosylation, a posttranslational modification involved, among other things, in transcription, DNA repair, and cell death, is carried out by a superfamily of 17 PARPs (Dantzer and Santoro 2013). These polymerases synthesize poly(ADP-ribose) (PAR) from NAD+, releasing nicotinamide. The PAR polymer binds to Glu, Asp, and Lys residues in nuclear proteins, including PARP itself, and creates a transitional nucleophilic environment. By virtue of the high negative charge of PAR polymers, marked auto-PARylation of PARP1 and PARP2 leads to their dissociation from DNA, which is required for DNA repair completion (Satoh and Lindahl 1992). The PARP1 enzyme is activated by DNA breaks and facilitates their repair by loosening chromatin and recruiting repair proteins to the site of injury. Poly-ADP-ribosylation modulates protein functions by regulating either enzymatic activities or macromolecular interactions with other proteins, DNA, or RNA. On the other hand, PAR molecules can also regulate protein activity and function through non-covalent binding that may serve to attract protein targets (Hakmé et al. 2008).
PARP is one of the first proteins that recognize injuries in DNA and is therefore in an ideal position to directly recruit the DNA base excision repair (BER) machinery to the site of DNA damage in living cells (Lindahl et al. 1995). Indeed, this interaction has been supported by the identification of a BER complex comprising PARP1, X-ray repair cross-complementing protein 1 (XRCC1), DNA ligase III, and DNA polymerase β (Caldecott et al. 1996; Kubota et al. 1996; Masson et al. 1998). Moreover, PARP1 has been recently identified as a partner of APE1, the main apurinic/apyrimidinic endonuclease responsible for the generation of apurinic/apyrimidinic sites when the BER mechanism is activated, indicating that PARP1 is able to stimulate the APE1 strand-incision activity (Prasad et al. 2015). The PAR polymer is mainly degraded by poly(ADP-ribose) glycohydrolases to form short polymers and monomers (Aredia and Scovassi 2014; Gagné et al. 2006). The common feature of the involvement of poly-ADP-ribosylation in different paradigms of cell death is represented by PAR, which can cause cells to die through diverse mechanisms (Bürkle and Virág 2013). In addition to catalytic inhibition, it was recently demonstrated that PARP inhibitors induce the formation of cytotoxic PARP–DNA complexes, and clinically relevant PARP inhibitors differ markedly in their potency to trap this complex. This study proposes a novel mechanism involved in the synthetic lethality and the involvement of PARP1 and PARP2, with several approaches to DNA repair, such as BER, homologous recombination (HR), and FANC proteins (Murai et al. 2012). Cancers characterized by BRCA1 and BRCA2 (proteins involved in DSB repair by HR) deficiencies have been treated using PARP inhibitors in the absence of exogenous DNA-damaging agents by targeting spontaneous DNA repair defects observed in certain tumors (Bryant et al. 2005; Farmer et al. 2005). In 2010, PARP inhibitors such as iniparib (BSI-201), olaparib (AZ2281), veliparib (ABT-888), AG014699, and INO-1001, among others, were used alone or in combination with other drugs in several clinical trials. Only two of these drugs reached phase III studies (Annunziata and O’Shaughnessy 2010). Currently, there are 161 clinical trials assessing the efficacy of PARP inhibitors alone or in combination with other drugs in cancer chemotherapy, 13 of which are in Phase III (http://clinicaltrials.gov).
In cardiomyocytes treated with DOX, the activation of poly-ADP-ribosylation can drive cells to energy insufficiency caused by NAD depletion (Pillai et al. 2005). In this case, cells die by necrosis, a more drastic mode of cell death. Infarcted rat hearts were shown to be characterized by increases in PARP activation, left ventricular mass, and the pathological score. These alterations were prevented by the administration of 3-aminobenzamide, a catalytic PARP inhibitor, demonstrating the involvement of PARP in the energy deprivation-mediated cell death (Wang et al. 2014). INO-1001, another catalytic PARP inhibitor, was able to markedly attenuate the reperfusion injury, resulting in a better recovery of biventricular and endothelial function as well as energy reserves after orthotropic pig heart transplantation, which opens great possibilities for clinical use of INO-1001 (Heger et al. 2005). However, a phase II study conducted to evaluate the safety of INO-1001 in subjects who had experienced heart attack and were to be treated with coronary angioplasty, was concluded with no results posted (http://clinicaltrials.gov). Nevertheless, rucaparib (AG014699), a PARP inhibitor tested in trials, ameliorates cardiotoxicity but does not enhance the DOX efficacy, despite improving tumor perfusion and a radiation response in mice (Ali et al. 2011). In a study conducted by Magan et al. (2012), HeLa cells treated with PJ34, a potent PARP inhibitor, showed increased Top2α promoter activity and, consequently, an increase in the Top2α protein level. The results indicated a new potential use for PARP1 inhibitors to reset cellular sensitivity to Top2 poisons by enhancing the amount of the Top2α protein present in cells and highlighted that PARP1 inhibitors have the potential to improve current chemotherapy regimes in a multifactorial manner (Magan et al. 2012). The data obtained in our laboratory demonstrated that the co-treatment with DOX or MTX and 3,4-dihydro-5-[4-(1-piperidinyl)butoxyl]-1(2H)-isoquinolinone (DPQ), a potent PARP inhibitor, diminished the H9c2 cell viability when compared with DOX or MTX treatment alone. There is evidence indicating a strong relation between PARP inhibition and an increase in DNA strand breaks in the rat cardiomyoblasts treated with DOX or MTX. Furthermore, despite the fact that PARP inhibition increased the antioxidant defense and decreased the ROS formation in the H9c2 cells treated with DOX or MTX, it was not sufficient to prevent cell death, demonstrating that ROS generation is not the main player in the cardiotoxicity induced by these drugs (to be published elsewhere).
Conclusions
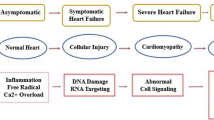
To explore the potential for further use of DOX and MTX in tumor therapy, continued studies are needed to assess the means to reduce their cardiotoxicity. Identification of new drugs with potential chemotherapeutic effectiveness superior to that of DOX remains a big challenge. As described here, even though they share similarities in their modes of toxicant action, DOX and MTX seem to differ in the key aspect. DOX is a more redox-interfering drug, while MTX induces energy imbalance. In addition, DOX toxicity can be explained by the Top2 beta and mitochondrial impairment, and increases in ROS generation are the underlying mechanism of DOX toxicity. The mode of action has not yet been fully elucidated for MTX, and this knowledge gap needs to be filled. In this context, PARP is a molecule that unifies the ROS energetic metabolism and DNA repair, among other processes, and should not be overlooked since the oxidative damage and DNA strand breaks generated by Top2 inhibition both require PARP function (Fig. 5).
Role of poly(ADP-ribose) polymerase 1 (PARP1) as a molecule that unifies the reactive oxygen species (ROS) energy metabolism and DNA repair, among other processes, cannot be overlooked since the oxidative damage and DNA strand breaks generated by topoisomerase 2 inhibition are among the processes that require PARP1 function. DOX, doxorubicin; DSB, double-strand break; MTX, mitoxantrone
Abbreviations
- APE:
-
Apurinic/apyrimidinic endonuclease
- BER:
-
Base excision repair
- CAT:
-
Catalase
- DFO:
-
Deferoxamine
- DOX:
-
Doxorubicin
- DSB:
-
Double-strand break
- eNOS:
-
Endothelial nitric oxide synthase
- ETC:
-
Electron transport chain
- HNE:
-
4-Hydroxy-2-nonenal
- HR:
-
Homologous recombination
- MS:
-
Multiple sclerosis
- mtDNA:
-
Mitochondrial DNA
- mtTop:
-
Mitochondrial topoisomerase
- MTX:
-
Mitoxantrone
- MTX-MET:
-
l-Methionine-conjugated MTX
- PAR:
-
Poly(ADP-ribose)
- PARP:
-
Poly(ADP-ribose) polymerase
- RNS:
-
Reactive nitrogen species
- ROS:
-
Reactive oxygen species
- SHR:
-
Spontaneously hypertensive rats
- SNP:
-
Single nucleotide polymorphism
- SOD:
-
Superoxide dismutase
- Top:
-
Topoisomerase
References
Adachi K, Fujiura Y, Mayumi F et al (1993) A deletion of mitochondrial DNA in murine doxorubicin-induced cardiotoxicity. Biochem Biophys Res Commun 195:945–951. doi:10.1006/bbrc.1993.2135
Alderton PM, Gross J, Green MD (1992) Comparative study of doxorubicin, mitoxantrone, and epirubicin in combination with ICRF-187 (ADR-529) in a chronic cardiotoxicity animal model. Cancer Res 52:194–201
Ali M, Kamjoo M, Thomas HD et al (2011) The clinically active PARP inhibitor AG014699 ameliorates cardiotoxicity but does not enhance the efficacy of doxorubicin, despite improving tumor perfusion and radiation response in mice. Mol Cancer Ther 10:2320–2329. doi:10.1158/1535-7163.MCT-11-0356
Annunziata CM, O’Shaughnessy J (2010) Poly (ADP-ribose) polymerase as a novel therapeutic target in cancer. Clin Cancer Res 16:4517–4526. doi:10.1158/1078-0432.CCR-10-0526
Aredia F, Scovassi AI (2014) Poly(ADP-ribose): a signaling molecule in different paradigms of cell death. Biochem Pharmacol. doi:10.1016/j.bcp.2014.06.021
Austin CA, Sng J-H, Patel S, Fisher LM (1993) Novel HeLa topoisomerase II is the IIβ isoform: complete coding sequence and homology with other type II topoisomerases. Biochim Biophys Acta Gene Struct Expr 1172:283–291. doi:10.1016/0167-4781(93)90215-Y
Bachmann E, Weber E, Zbinden G (1987) Effects of mitoxantrone and doxorubicin on energy metabolism of the rat heart. Cancer Treat Rep 71:361–366
Basra J, Wolf CR, Brown JR, Patterson LH (1985) Evidence for human liver mediated free-radical formation by doxorubicin and mitozantrone. Anticancer Drug Des 1:45–52
Bryant HE, Schultz N, Thomas HD et al (2005) Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature 434:913–917. doi:10.1038/nature03443
Bürkle A, Virág L (2013) Poly(ADP-ribose): PARadigms and PARadoxes. Mol Aspects Med 34:1046–1065. doi:10.1016/j.mam.2012.12.010
Caceres RA, Pauli I, Timmers LFSM, de Azevedo WF (2008) Molecular recognition models: a challenge to overcome. Curr Drug Targets 9:1077–1083
Caldecott KW, Aoufouchi S, Johnson P, Shall S (1996) XRCC1 polypeptide interacts with DNA polymerase beta and possibly poly (ADP-ribose) polymerase, and DNA ligase III is a novel molecular “nick-sensor” in vitro. Nucleic Acids Res 24:4387–4394
Capranico G, Zunino F (1992) DNA topoisomerase-trapping antitumour drugs. Eur J Cancer 28A:2055–2060
Carvalho FS, Burgeiro A, Garcia R et al (2014) Doxorubicin-induced cardiotoxicity: from bioenergetic failure and cell death to cardiomyopathy. Med Res Rev 34:106–135. doi:10.1002/med.21280
Cavalcante RP, da Rocha Sandim L, Bogo D et al (2013) Application of Fenton, photo-Fenton, solar photo-Fenton, and UV/H2O2 to degradation of the antineoplastic agent mitoxantrone and toxicological evaluation. Environ Sci Pollut Res Int 20:2352–2361. doi:10.1007/s11356-012-1110-y
Champoux JJ (2001) DNA T < scp > OPOISOMERASES </scp > : structure, function, and mechanism. Annu Rev Biochem 70:369–413. doi:10.1146/annurev.biochem.70.1.369
Cheng CC, Zee-Cheng RK (1983) The design, synthesis and development of a new class of potent antineoplastic anthraquinones. Prog Med Chem 20:83–118
Cini-Neri G, Neri B (1986) Reduction of oxygen uptake in vitro as an index of cardiac toxicity induced by new anthracyclines. Anticancer Res 6:195–197
Costa VM, Carvalho F, Bastos ML et al (2011) Contribution of catecholamine reactive intermediates and oxidative stress to the pathologic features of heart diseases. Curr Med Chem 18:2272–2314
Costa VM, Carvalho F, Duarte JA et al (2013) The heart as a target for xenobiotic toxicity: the cardiac susceptibility to oxidative stress. Chem Res Toxicol 26:1285–1311. doi:10.1021/tx400130v
Cotte S, Von Ahsen N, Kruse N et al (2009) ABC-transporter gene-polymorphisms are potential pharmacogenetic markers for mitoxantrone response in multiple sclerosis. Brain 132:2517–2530. doi:10.1093/brain/awp164
Dantzer F, Santoro R (2013) The expanding role of PARPs in the establishment and maintenance of heterochromatin. FEBS J 280:3508–3518. doi:10.1111/febs.12368
De Isabella P, Palumbo M, Sissi C et al (1995) Topoisomerase II DNA cleavage stimulation, DNA binding activity, cytotoxicity, and physico-chemical properties of 2-aza- and 2-aza-oxide-anthracenedione derivatives. Mol Pharmacol 48:30–38
Di Marco A, Gaetani M, Orezzi P et al (1964) “Daunomycin”, a new antibiotic of the rhodomycin group. Nature 201:706–707
Dores-Sousa JL, Duarte JA, Seabra V et al (2015) The age factor for mitoxantrone’s cardiotoxicity: multiple doses render the adult mouse heart more susceptible to injury. Toxicology 329:106–119. doi:10.1016/j.tox.2015.01.006
Dröse S, Brandt U (2012) Molecular mechanisms of superoxide production by the mitochondrial respiratory chain. Adv Exp Med Biol 748:145–169. doi:10.1007/978-1-4614-3573-0_6
Duthie SJ, Grant MH (1989) The role of reductive and oxidative metabolism in the toxicity of mitoxantrone, adriamycin and menadione in human liver derived Hep G2 hepatoma cells. Br J Cancer 60:566–571
Elihu N, Anandasbapathy S, Frishman WH (1998) Chelation therapy in cardiovascular disease: ethylenediaminetetraacetic acid, deferoxamine, and dexrazoxane. J Clin Pharmacol 38:101–105. doi:10.1002/j.1552-4604.1998.tb04397.x
Farmer H, McCabe N, Lord CJ et al (2005) Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 434:917–921. doi:10.1038/nature03445
Faulds D, Balfour JA, Chrisp P, Langtry HD (1991) Mitoxantrone: a review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential in the chemotherapy of cancer. Drugs 41:400–449
Fenu G, Lorefice L, Frau F et al (2015) Induction and escalation therapies in multiple sclerosis. Antiinflamm Antiallergy Agents Med Chem 14:26–34
Ferreira ALA, Matsubara LS, Matsubara BB (2008) Anthracycline-induced cardiotoxicity. Cardiovasc Hematol Agents Med Chem 6:278–281
Figueira TR, Barros MH, Camargo AA et al (2013) Mitochondria as a source of reactive oxygen and nitrogen species: from molecular mechanisms to human health. Antioxid Redox Signal 18:2029–2074. doi:10.1089/ars.2012.4729
Gagné J-P, Hendzel MJ, Droit A, Poirier GG (2006) The expanding role of poly(ADP-ribose) metabolism: current challenges and new perspectives. Curr Opin Cell Biol 18:145–151. doi:10.1016/j.ceb.2006.02.013
Giulivi C, Boveris A, Cadenas E (1995) Hydroxyl radical generation during mitochondrial electron transfer and the formation of 8-hydroxydesoxyguanosine in mitochondrial DNA. Arch Biochem Biophys 316:909–916. doi:10.1006/abbi.1995.1122
Green PS, Leeuwenburgh C (2002) Mitochondrial dysfunction is an early indicator of doxorubicin-induced apoptosis. Biochim Biophys Acta Mol Basis Dis 1588:94–101. doi:10.1016/S0925-4439(02)00144-8
Gréen H, Falk IJ, Lotfi K et al (2012) Association of ABCB1 polymorphisms with survival and in vitro cytotoxicty in de novo acute myeloid leukemia with normal karyotype. Pharmacogenomics J 12:111–118. doi:10.1038/tpj.2010.79
Hakmé A, Wong H-K, Dantzer F, Schreiber V (2008) The expanding field of poly(ADP-ribosyl)ation reactions. “protein modifications: beyond the usual suspects” review series. EMBO Rep 9:1094–1100. doi:10.1038/embor.2008.191
Halliwell B (2009) The wanderings of a free radical. Free Radic Biol Med 46:531–542. doi:10.1016/j.freeradbiomed.2008.11.008
Halliwell B, Gutteridge JM (1984) Oxygen toxicity, oxygen radicals, transition metals and disease. Biochem J 219:1–14
Hasinoff BB, Patel D, Wu X (2003) The oral iron chelator ICL670A (deferasirox) does not protect myocytes against doxorubicin. Free Radic Biol Med 35:1469–1479. doi:10.1016/j.freeradbiomed.2003.08.005
Heger U, Flechtenmacher C, Ba S et al (2005) Poly (ADP-ribose) polymerase inhibition attenuates biventricular reperfusion injury after orthotopic heart transplantation *. Eur J Cardio-Thoracic Surg 27:226–234. doi:10.1016/j.ejcts.2004.10.055
Herman E (1997) Comparison of the structural changes induced by doxorubicin and mitoxantrone in the heart, kidney and intestine and characterization of the Fe(III)-mitoxantrone complex. J Mol Cell Cardiol 29:2415–2430. doi:10.1006/jmcc.1997.0477
Herman EH, Ferrans VJ, Young RS, Hamlin RL (1988) Effect of pretreatment with ICRF-187 on the total cumulative dose of doxorubicin tolerated by beagle dogs. Cancer Res 48:6918–6925
Herman EH, Zhang J, Hasinoff BB et al (1997) Comparison of the structural changes induced by doxorubicin and mitoxantrone in the heart, kidney and intestine and characterization of the Fe(III)-mitoxantrone complex. J Mol Cell Cardiol 29:2415–2430
Herman EH, Zhang J, Rifai N et al (2001) The use of serum levels of cardiac troponin T to compare the protective activity of dexrazoxane against doxorubicin- and mitoxantrone-induced cardiotoxicity. Cancer Chemother Pharmacol 48:297–304
Hermanson DL, Das SG, Li Y, Xing C (2013) Overexpression of Mcl-1 confers multidrug resistance, whereas topoisomerase IIβ downregulation introduces mitoxantrone-specific drug resistance in acute myeloid leukemia. Mol Pharmacol 84:236–243. doi:10.1124/mol.113.086140
Hixon S (1981) Heart mitochondrial DNA synthesis: preferential inhibition by adriamycin. J Mol Cell Cardiol 13:855–860. doi:10.1016/0022-2828(81)90242-X
Hsiao CJ, Li TK, Chan YL et al (2008) WRC-213, an l-methionine-conjugated mitoxantrone derivative, displays anticancer activity with reduced cardiotoxicity and drug resistance: identification of topoisomerase II inhibition and apoptotic machinery in prostate cancers. Biochem Pharmacol 75:847–856. doi:10.1016/j.bcp.2007.10.012
Huang N-L, Lin J-H (2014) Drug-induced conformational population shifts in topoisomerase-DNA ternary complexes. Molecules 19:7415–7428. doi:10.3390/molecules19067415
Iarussi D, Indolfi P, Casale F et al (2001) Recent advances in the prevention of anthracycline cardiotoxicity in childhood. Curr Med Chem 8:1649–1660
Ichikawa Y, Ghanefar M, Bayeva M et al (2014) Cardiotoxicity of doxorubicin is mediated through mitochondrial iron accumulation. J Clin Invest 124:617–630. doi:10.1172/JCI72931
Ide T, Tsutsui H, Kinugawa S et al (2000) Direct evidence for increased hydroxyl radicals originating from superoxide in the failing myocardium. Circ Res 86:152–157. doi:10.1161/01.RES.86.2.152
Joyce E, Mulroy E, Scott J et al (2013) Subclinical myocardial dysfunction in multiple sclerosis patients remotely treated with mitoxantrone: evidence of persistent diastolic dysfunction. J Card Fail 19:571–576. doi:10.1016/j.cardfail.2013.06.003
Kharasch ED, Novak RF (1983) Bis(alkylamino)anthracenedione antineoplastic agent metabolic activation by NADPH-cytochrome P-450 reductase and NADH dehydrogenase: diminished activity relative to anthracyclines. Arch Biochem Biophys 224:682–694
Khiati S, Dalla Rosa I, Sourbier C et al (2014) Mitochondrial topoisomerase I (top1mt) is a novel limiting factor of doxorubicin cardiotoxicity. Clin Cancer Res 20:4873–4881. doi:10.1158/1078-0432.CCR-13-3373
Kubota Y, Nash RA, Klungland A et al (1996) Reconstitution of DNA base excision-repair with purified human proteins: interaction between DNA polymerase beta and the XRCC1 protein. EMBO J 15:6662–6670
Lebrecht D, Walker UA (2007) Role of mtDNA lesions in anthracycline cardiotoxicity. Cardiovasc Toxicol 7:108–113. doi:10.1007/s12012-007-0009-1
Lee CH, Hsieh MY, Hsin LW et al (2012) Anthracenedione-methionine conjugates are novel topoisomerase II-targeting anticancer agents with favorable drug resistance profiles. Biochem Pharmacol 83:1208–1216. doi:10.1016/j.bcp.2012.01.025
Li SJ, Rodgers EH, Grant MH (1995) The activity of xenobiotic enzymes and the cytotoxicity of mitoxantrone in MCF 7 human breast cancer cells treated with inducing agents. Chem Biol Interact 97:101–118. doi:10.1016/0009-2797(94)03603-6
Lindahl T, Satoh MS, Poirier GG, Klungland A (1995) Post-translational modification of poly(ADP-ribose) polymerase induced by DNA strand breaks. Trends Biochem Sci 20:405–411. doi:10.1016/S0968-0004(00)89089-1
Link G, Tirosh R, Pinson A, Hershko C (1996) Role of iron in the potentiation of anthracycline cardiotoxicity: identification of heart cell mitochondria as a major site of iron-anthracycline interaction. J Lab Clin Med 127:272–278
Magan N, Isaacs RJ, Stowell KM (2012) Treatment with the PARP-inhibitor PJ34 causes enhanced doxorubicin-mediated cell death in HeLa cells. Anticancer Drugs 23:627–637. doi:10.1097/CAD.0b013e328350900f
Masson M, Niedergang C, Schreiber V et al (1998) XRCC1 is specifically associated with poly(ADP-ribose) polymerase and negatively regulates its activity following DNA damage. Mol Cell Biol 18:3563–3571
Mewes K, Blanz J, Ehninger G et al (1993) Cytochrome P-450-induced cytotoxicity of mitoxantrone by formation of electrophilic intermediates. Cancer Res 53:5135–5142
Millefiorini E, Gasperini C, Pozzilli C et al (1997) Randomized placebo-controlled trial of mitoxantrone in relapsing-remitting multiple sclerosis: 24-month clinical and MRI outcome. J Neurol 244:153–159
Mimnaugh EG, Trush M, Ginsburg E, Gram TE (1982) Differential effects of anthracycline drugs on rat heart and liver microsomal reduced nicotinamide adenine dinucleotide phosphate-dependent lipid peroxidation. Cancer Res 42:3574–3582
Miranda CJ, Makui H, Soares RJ et al (2003) Hfe deficiency increases susceptibility to cardiotoxicity and exacerbates changes in iron metabolism induced by doxorubicin. Blood 102:2574–2580. doi:10.1182/blood-2003-03-0869
Morris GM, Huey R, Lindstrom W et al (2009) AutoDock4 and AutoDockTools4: automated docking with selective receptor flexibility. J Comput Chem 30:2785–2791. doi:10.1002/jcc.21256
Murai J, Huang SYN, Das BB et al (2012) Trapping of PARP1 and PARP2 by clinical PARP inhibitors. Cancer Res 72:5588–5599. doi:10.1158/0008-5472.CAN-12-2753
Murphy MP, Holmgren A, Larsson N-G et al (2011) Unraveling the biological roles of reactive oxygen species. Cell Metab 13:361–366. doi:10.1016/j.cmet.2011.03.010
Neilan TG, Blake SL, Ichinose F et al (2007) Disruption of nitric oxide synthase 3 protects against the cardiac injury, dysfunction, and mortality induced by doxorubicin. Circulation 116:506–514. doi:10.1161/CIRCULATIONAHA.106.652339
Ning Y, Shen Q, Herrick K et al (2012) Abstract LB-339: cause of death in cancer survivors. Cancer Res 72:LB-339. doi:10.1158/1538-7445.AM2012-LB-339
Nishida K, Otsu K (2008) Cell death in heart failure. Circ J 72 Suppl A:A17–A21
Octavia Y, Tocchetti CG, Gabrielson KL et al (2012) Doxorubicin-induced cardiomyopathy: from molecular mechanisms to therapeutic strategies. J Mol Cell Cardiol 52:1213–1225. doi:10.1016/j.yjmcc.2012.03.006
Pacher P, Szabó C (2007) Role of poly(ADP-ribose) polymerase 1 (PARP-1) in cardiovascular diseases: the therapeutic potential of PARP inhibitors. Cardiovasc Drug Rev 25:235–260. doi:10.1111/j.1527-3466.2007.00018.x
Panjrath GS, Patel V, Valdiviezo CI et al (2007) Potentiation of Doxorubicin cardiotoxicity by iron loading in a rodent model. J Am Coll Cardiol 49:2457–2464. doi:10.1016/j.jacc.2007.02.060
Panousis C, Kettle AJ, Phillips DR (1994) Oxidative metabolism of mitoxantrone by the human neutrophil enzyme myeloperoxidase. Biochem Pharmacol 48:2223–2230. doi:10.1016/0006-2952(94)00429-3
Papa S (1996) Mitochondrial oxidative phosphorylation changes in the life span. Molecular aspects and physiopathological implications. Biochim Biophys Acta 1276:87–105
Park E-J, Chan DW, Park J-H et al (2003) DNA-PK is activated by nucleosomes and phosphorylates H2AX within the nucleosomes in an acetylation-dependent manner. Nucleic Acids Res 31:6819–6827
Pillai JB, Isbatan A, Imai SI, Gupta MP (2005) Poly(ADP-ribose) polymerase-1-dependent cardiac myocyte cell death during heart failure is mediated by NAD + depletion and reduced Sir2α deacetylase activity. J Biol Chem 280:43121–43130. doi:10.1074/jbc.M506162200
Pommier Y (2013) Drugging topoisomerases: lessons and Challenges. ACS Chem Biol 8:82–95. doi:10.1021/cb300648v
Pommier Y, Leo E, Zhang H, Marchand C (2010) DNA topoisomerases and their poisoning by anticancer and antibacterial drugs. Chem Biol 17:421–433. doi:10.1016/j.chembiol.2010.04.012
Prasad R, Dyrkheeva N, Williams J, Wilson SH (2015) Mammalian base excision repair: functional partnership between PARP-1 and APE1 in AP-site repair. PLoS ONE 10:e0124269. doi:10.1371/journal.pone.0124269
Rao VA, Zhang J, Klein SR et al (2011) The iron chelator Dp44mT inhibits the proliferation of cancer cells but fails to protect from doxorubicin-induced cardiotoxicity in spontaneously hypertensive rats. Cancer Chemother Pharmacol 68:1125–1134. doi:10.1007/s00280-011-1587-y
Richardson DR, Ponka P (1997) The molecular mechanisms of the metabolism and transport of iron in normal and neoplastic cells. Biochim Biophys Acta 1331:1–40
Roca J, Wang JC (1994) DNA transport by a type II DNA topoisomerase: evidence in favor of a two-gate mechanism. Cell 77:609–616
Rogakou EP, Pilch DR, Orr AH et al (1998) DNA double-stranded breaks induce histone H2AX phosphorylation on serine 139. J Biol Chem 273:5858–5868. doi:10.1074/jbc.273.10.5858
Rossato LG, Costa VM, De Pinho PG et al (2013a) The metabolic profile of mitoxantrone and its relation with mitoxantrone-induced cardiotoxicity. Arch Toxicol 87:1809–1820. doi:10.1007/s00204-013-1040-6
Rossato LG, Costa VM, Vilas-Boas V et al (2013b) Therapeutic concentrations of mitoxantrone elicit energetic imbalance in H9c2 cells as an earlier event. Cardiovasc Toxicol 13:413–425. doi:10.1007/s12012-013-9224-0
Rossato LG, Costa VM, Dallegrave E et al (2014) Mitochondrial cumulative damage induced by mitoxantrone: late onset cardiac energetic impairment. Cardiovasc Toxicol 14:30–40. doi:10.1007/s12012-013-9230-2
Saffi J, Agnoletto MH, Guecheva TN et al (2010) Effect of the anti-neoplastic drug doxorubicin on XPD-mutated DNA repair-deficient human cells. DNA Repair (Amst) 9:40–47. doi:10.1016/j.dnarep.2009.10.003
Sant M, Allemani C, Santaquilani M et al (2009) EUROCARE-4. Survival of cancer patients diagnosed in 1995–1999. Results and commentary. Eur J Cancer 45:931–991. doi:10.1016/j.ejca.2008.11.018
Satoh MS, Lindahl T (1992) Role of poly(ADP-ribose) formation in DNA repair. Nature 356:356–358. doi:10.1038/356356a0
Senkus E, Jassem J (2011) Cardiovascular effects of systemic cancer treatment. Cancer Treat Rev 37:300–311. doi:10.1016/j.ctrv.2010.11.001
Serrano J, Palmeira CM, Kuehl DW, Wallace KB (1999) Cardioselective and cumulative oxidation of mitochondrial DNA following subchronic doxorubicin administration. Biochim Biophys Acta Bioenerg 1411:201–205. doi:10.1016/S0005-2728(99)00011-0
Shipp NG, Dorr RT, Alberts DS et al (1993a) Characterization of experimental mitoxantrone cardiotoxicity and its partial inhibition by ICRF-187 in cultured neonatal rat heart cells. Cancer Res 53:550–556
Shipp NG, Dorr RT, Alberts DS et al (1993b) Characterization of experimental mitoxantrone cardiotoxicity and its partial inhibition by ICRF-187 in cultured neonatal rat heart cells. Cancer Res 53:550–556
Sies H (1997) Oxidative stress: oxidants and antioxidants. Exp Physiol 82:291–295
Šimůnek T, Štěrba M, Popelová O et al (2009) Anthracycline-induced cardiotoxicity: overview of studies examining the roles of oxidative stress and free cellular iron. Pharmacol Rep 61:154–171
Stěrba M, Popelová O, Lenčo J et al (2011) Proteomic insights into chronic anthracycline cardiotoxicity. J Mol Cell Cardiol 50:849–862. doi:10.1016/j.yjmcc.2011.01.018
Stěrba M, Popelová O, Vávrová A et al (2013) Oxidative stress, redox signaling, and metal chelation in anthracycline cardiotoxicity and pharmacological cardioprotection. Antioxid Redox Signal 18:899–929. doi:10.1089/ars.2012.4795
Tan C, Tasaka H, Yu KP et al (1967) Daunomycin, an antitumor antibiotic, in the treatment of neoplastic disease. Clinical evaluation with special reference to childhood leukemia. Cancer 20:333–353
Tsutsui H, Kinugawa S, Matsushima S (2008) Oxidative stress and mitochondrial DNA damage in heart failure. Circ J 72:A31–A37. doi:10.1253/circj.CJ-08-0014
Vásquez-Vivar J, Kalyanaraman B, Martásek P et al (1998) Superoxide generation by endothelial nitric oxide synthase: the influence of cofactors. Proc Natl Acad Sci USA 95:9220–9225
Vejpongsa P, Yeh ETH (2013) Topoisomerase 2β: a promising molecular target for primary prevention of anthracycline-induced cardiotoxicity. Clin Pharmacol Ther 95:45–52. doi:10.1038/clpt.2013.201
Vejpongsa P, Yeh ETH (2014a) Topoisomerase 2β: a promising molecular target for primary prevention of anthracycline-induced cardiotoxicity. Clin Pharmacol Ther 95:45–52. doi:10.1038/clpt.2013.201
Vejpongsa P, Yeh ETH (2014b) Prevention of anthracycline-induced cardiotoxicity. J Am Coll Cardiol 64:938–945. doi:10.1016/j.jacc.2014.06.1167
Von Hoff DD, Rozencweig M, Layard M et al (1977) Daunomycin-induced cardiotoxicity in children and adults. A review of 110 cases. Am J Med 62:200–208. doi:10.1016/0002-9343(77)90331-X
Wallace KB (2003) Doxorubicin-induced cardiac mitochondrionopathy. Pharmacol Toxicol 93:105–115
Wallace AC, Laskowski RA, Thornton JM (1995) LIGPLOT: a program to generate schematic diagrams of protein-ligand interactions. Protein Eng 8:127–134
Wang M, Hu B, Zhang Y-L et al (2014) Effects of 3-aminobenzamide on ventricular function in infarct heart assessed by quantitative tissue velocity imaging. J Cardiovasc Med (Hagerstown). doi:10.2459/JCM.0000000000000061
Weilbach FX, Chan A, Toyka KV, Gold R (2004) The cardioprotector dexrazoxane augments therapeutic efficacy of mitoxantrone in experimental autoimmune encephalomyelitis. Clin Exp Immunol 135:49–55. doi:10.1111/j.1365-2249.2004.02344.x
Wojnowski L, Kulle B, Schirmer M et al (2005) NAD(P)H oxidase and multidrug resistance protein genetic polymorphisms are associated with doxorubicin-induced cardiotoxicity. Circulation 112:3754–3762. doi:10.1161/CIRCULATIONAHA.105.576850
Wosniak J, Santos CXC, Kowaltowski AJ, Laurindo FRM (2009) Cross-talk between mitochondria and NADPH oxidase: effects of mild mitochondrial dysfunction on angiotensin II-mediated increase in Nox isoform expression and activity in vascular smooth muscle cells. Antioxid Redox Signal 11:1265–1278. doi:10.1089/ars.2009.2392
Wu C-C, Li Y-C, Wang Y-R et al (2013) On the structural basis and design guidelines for type II topoisomerase-targeting anticancer drugs. Nucleic Acids Res 41:10630–10640. doi:10.1093/nar/gkt828
Yi LL, Kerrigan JE, Lin CP et al (2007) Topoisomerase IIβ-mediated DNA double-strand breaks: implications in doxorubicin cardiotoxicity and prevention by dexrazoxane. Cancer Res 67:8839–8846. doi:10.1158/0008-5472.CAN-07-1649
Zhang YW, Shi J, Li YJ, Wei L (2009) Cardiomyocyte death in doxorubicin-induced cardiotoxicity. Arch Immunol Ther Exp (Warsz) 57:435–445. doi:10.1007/s00005-009-0051-8
Zhang S, Liu X, Bawa-Khalfe T, Lu L-S, Lyu YL, Liu LF, Yeh ETH (2012) Identification of the molecular basis of doxorubicin-induced cardiotoxicity. Nat Med 18(11):1639–1642. doi:10.1038/nm.2919
Zhao Y, Miriyala S, Miao L et al (2014) Redox proteomic identification of HNE-bound mitochondrial proteins in cardiac tissues reveals a systemic effect on energy metabolism after doxorubicin treatment. Free Radic Biol Med 72:55–65. doi:10.1016/j.freeradbiomed.2014.03.001
Acknowledgments
The authors would like to thank the CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico, Brasília, Brazil—Grant No. 479564/2013-2) and PRONEX–FAPERGS/CNPq (Grant No. 10/0044-3) for grant support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Damiani, R.M., Moura, D.J., Viau, C.M. et al. Pathways of cardiac toxicity: comparison between chemotherapeutic drugs doxorubicin and mitoxantrone. Arch Toxicol 90, 2063–2076 (2016). https://doi.org/10.1007/s00204-016-1759-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-016-1759-y