Abstract
A recent study suggested that neuroinflammation plays a major role in the pathogenesis of a number of neurodegenerative diseases such as Alzheimer’s disease and Parkinson’s disease. Although the precise mechanism is obscure, dysregulation of the signaling transduction pathway in microglia may enhance inflammation, leading to synaptic dysfunction and ultimately to neuronal cell death. The expression and function of the P2X7 receptor (P2X7R), an ATP-gated ion channel abundantly expressed in microglia in the brain, is significantly up-regulated in the postmortem brain of Alzheimer’s disease patients and various neurodegenerative disease animal models. This supports the role of the P2X7R pathway in the progression of neurodegeneration. Blocking P2X7R using brilliant blue G, a P2X7R antagonist that can cross the blood–brain barrier, has been shown to result in the amelioration of neuropathology in various animal models. Taken together, these results raise the possibility that the P2X7R signaling pathway could be a therapeutic target for treating various neurodegenerative diseases.
Similar content being viewed by others
Introduction
Neurodegenerative diseases are characterized by various histopathological features, including intracellular inclusion bodies, extracellular amyloid deposits, axonal swelling, synaptic loss, and neuronal cell death. Although the precise mechanism leading to the formation of neuronal pathology and ultimately to neuronal death remains incompletely understood, mounting evidence suggests that protein aggregation plays a central role in the pathogenesis of such diseases (Fujita et al. 2006; Hashimoto and Masliah 1999). Due to gene mutations and/or environmental factors, disease-specific amyloidogenic proteins such as amyloid-β (Aβ) and α-synuclein aggregate to form neurotoxic proto-fibrils leading to neurotoxicity.
In addition to the direct toxic effects of these protein aggregates, a recent study showed that inflammation may play a considerable role in neurotoxicity (Sugama et al. 2009). As microglial cell-driven inflammatory responses result in the release of various inflammatory mediators, including an array of neurotoxic cytokines, it is possible that an abnormally up-regulated inflammatory response may exacerbate neurodegeneration. Supporting the role of glial activation in neurodegeneration, epidemiology studies have shown that long-term users of non-steroidal anti-inflammatory drugs, i.e. ibuprofen and indomethacin, have significantly lower frequencies of neurodegenerative disease, including Alzheimer’s disease (AD) and Parkinson’s disease (Sugama et al. 2009). Based on this, extensive studies are in progress to determine whether anti-inflammatory drugs are effective in treating neurodegenerative diseases.
Given the critical role of microglial activation in neurodegeneration, we predict that dysregulation of the signal transduction pathway in microglia may contribute to enhanced neuroinflammation in neurodegenerative disease. In this context, this short review focuses mainly on the role of the P2X7 receptor (P2X7R) in the pathogenesis of neurodegenerative diseases. A recent study showed that increased expression and function of P2X7R is associated with AD (McLarnon et al. 2006). Furthermore, the pharmacological blockade of the P2X7R pathway results in amelioration of neuropathology in animal models of neurodegenerative diseases (Diaz-Hernandez et al. 2009; Ryu and McLarnon 2008). This suggests that P2X7R may be important as a therapeutic target for neurodegenerative diseases.
The P2X7R: Unique Properties Distinct From Other P2X Family Receptors
P2X7R is a purinergic P2 receptor, which are categorized into two major families, P2X ionotropic receptors and P2Y metabotropic receptors. The P2X receptors are ATP-gated ion channels, while the P2Y receptors are G protein-coupled receptors. To date, seven P2X (P2X1-7) and twelve P2Y (P2Y1, P2Y2, P2Y4-6, and P2Y8-14) receptors have been cloned from mammalian and avian species (Abbracchio et al. 2006; North 2002).
P2X7R was initially cloned in 1996 from a rat brain cDNA library and classified as a member of the P2X receptor family due to its amino-acid sequence homology (Surprenant et al. 1996). Similar to other members of the P2X receptor family, P2X7R functions as an ion channel in response to extracellular ATP and is permeable to several small cations such as Ca2+, K+, and Na+ (North 2002). However, distinct from other P2X receptors, P2X7R has a long C-terminal tail that interacts with several proteins and lipids in the cytoplasm (Denlinger et al. 2001; North 2002; Surprenant et al. 1996) and thus ATP can activate multiple intracellular signaling pathways through this receptor. P2X7R possesses some unique properties: (1) much higher concentrations (around the millimolar range) of extracellular ATP are required to activate P2X7R, which is higher than those required for the other P2X receptors (Surprenant et al. 1996), (2) the channel activity of P2X7R induced by ATP is accompanied by slow or no desensitization during application, while rapid desensitization is observed for other P2X receptors (North 2002), (3) prolonged activation of P2X7R using higher concentrations of ATP results in pore formation in the plasma membrane leading to the uptake of molecules as large as 900 Da and cell death (Di Virgilio et al. 1998), and (4) extracellular divalent cations such as Ca2+, Mg2+, Cu2+, and Zn2+ potently inhibit the activation of P2X7R by ATP (Jiang 2009). Based on these properties, it is believed that ATP exerts specific biological actions through P2X7R activation that never occur even when other P2X receptors are activated.
Functional Expression of P2X7R in Microglia and its Role in Brain Inflammation
P2X7R is highly expressed in the cells of monocyte/macrophage lineages and plays important roles in the innate immune system. In the central nervous system (CNS), extensive functional expression of P2X7R was demonstrated in microglia because these cells are the resident macrophages of the brain (Kaur et al. 2001).
Using primary microglial cultures and immortalized microglial cells, we and others have demonstrated that the activation of P2X7R with higher doses of ATP elicits a sustained influx of extracellular Ca2+ as well as intracellular K+ efflux (Ferrari et al. 1996; Takenouchi et al. 2005; Takenouchi et al. 2008). P2X7R activation also leads to the activation of multiple intracellular signaling pathways in microglial cells such as the p44/42 ERK kinase, p38 mitogen-activated protein kinase, c-Jun N-terminal kinase, AMP-activated protein kinase-α, mammalian target of rapamycin/S6 kinase, NF-κB signaling, and nuclear factor of activated T-cell signaling pathways (Ferrari et al. 1997c; Kataoka et al. 2009; Parvathenani et al. 2003; Suzuki et al. 2004; Takenouchi et al. 2007b; Takenouchi et al. 2009a). These P2X7R-mediated signals contribute to the expression of various microglia cellular responses induced by ATP.
Through the activation of P2X7R, ATP induces the secretion of pro-inflammatory cytokines and chemokines such as tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), and CC-chemokine ligand 3 (Ferrari et al. 2006; Kataoka et al. 2009; Suzuki et al. 2004) and also stimulates the production of superoxide and nitric oxide in microglial cells (Gendron et al. 2003; Parvathenani et al. 2003). Among the pro-inflammatory cytokines, recent studies have demonstrated a critical role for P2X7R in the processing and release of IL-1β from microglial cells (Ferrari et al. 1997b; Takenouchi et al. 2009b). IL-1β is initially synthesized as a biologically inactive pro-IL-1β that accumulates in the cytoplasm. The activation of P2X7R by ATP triggers inflammasome activation followed by the processing of pro-IL-1β to mature IL-1β (mIL-1β) and massive release of mIL-1β into the extracellular space. Although priming with the bacterial endotoxin lipopolysaccharide through innate Toll-like receptors is well recognized to induce gene expression and protein synthesis of pro-IL-1β in microglia, this is insufficient to trigger the rapid release of mIL-1β. Since mIL-1β is a key regulator of the brain cytokine network and causes various biological actions related to not only physiological regulation, but also pathological conditions, strict regulatory mechanisms probably exist for the maturation and release of IL-1β. Thus, it is considered that P2X7R activation is an essential second step in the triggering of the release of mIL-1β from microglial cells.
Similar to the case for peripheral macrophages, prolonged activation of P2X7R leads to the formation of membrane pores in microglial cells, which results in the induction of apoptotic/necrotic cell death in microglial cells (Ferrari et al. 1997a). However, modest activation of P2X7R was found to be inversely correlated with the increased proliferation of these cells (Bianco et al. 2006; Monif et al. 2009). Taking these results together, we predict that P2X7R may be fundamentally important for the regulation of both cell death and cell proliferation.
Altered Expression and Function of P2X7R in Neurodegenerative Conditions
It has recently been shown that the expression and function of P2X7R are increased in the AD brain and in various animal models of neurodegenerative diseases. These observations are consistent with the notion that P2X7R plays a critical role in the neuroinflammation observed during the pathogenesis of neurodegenerative disease.
AD is histopathologically characterized by massive neuronal loss, astrocytosis, and microglial activation. The accumulation of aggregated Aβ in senile plaques is a typical hallmark of the AD brain (Selkoe 1996). The up-regulation of P2X7R expression was demonstrated in transgenic mice over-expressing mutant APP (K670N, M671L), and it was determined that P2X7R is up-regulated around amyloid plaques and is regionally localized on activated microglia and astrocytes (Parvathenani et al. 2003). Consistent with this study, enhanced expression of P2X7R was demonstrated in adult microglia derived from postmortem AD brains compared with that in non-demented brains (McLarnon et al. 2006). It was further shown that Aβ triggers increases in intracellular Ca2+, ATP release, IL-1β secretion, and plasma membrane permeabilization in microglia from wild-type but not P2X7R-deleted mice (Sanz et al. 2009). Likewise, intra-hippocampal injection of Aβ caused a large accumulation of IL-1β in wild-type but not P2X7R-deleted mice (Sanz et al. 2009). These results suggest that P2X7R is an obligate participant in microglial activation caused by Aβ. Collectively, it is reasonable to speculate that increased levels of P2X7R may be correlated with the over-activation of the inflammatory response in microglia contributing to the progression of neuronal loss in AD.
The altered expression and function of P2X7R in microglia may be associated with the development of other neurodegenerative diseases, including prion disease and Huntington’s disease (HD). Prion disease is caused by an accumulation of abnormal forms of prion protein (PrPSc) (Prusiner 1991) and is histopathologically associated with brain vacuolation, neuronal cell death, astrocytosis, and microgliosis (Crozet et al. 2008). Using PrPSc-infected mice, we recently demonstrated that the mRNA level of P2X7R gradually increased in the brain during disease progression in these mice (Takenouchi et al. 2007a). Furthermore, PrPSc-infected microglia exhibited hypersensitivity to P2X7R, as demonstrated by the up-regulation of several receptor functions such as Ca2+ influx, membrane pore formation, the induction of microglial cell death, and the release of mIL-1β (Iwamaru et al. 2007; Takenouchi et al. 2007a).
HD is a neurodegenerative disorder caused by a CAG triplet-repeat expansion that codes for a polyglutamine sequence in the N-terminal region of the Huntington protein (The Huntington’s Disease Collaboratine Research Group 1993). Recently, increases in the expression and function of P2X7R in synaptic terminals were demonstrated in the brain of HD model mice, suggesting that ATP-induced synaptic dysregulation and neuronal cell death caused by the altered expression of neuronal P2X7R contributes to HD pathogenesis (Diaz-Hernandez et al. 2009). Notably, in the Caenorhabditis elegans and Drosophila models of HD it was reported that in vivo administration of drugs that impair ATP production, such as rotenone and oligomycin, protected against neuronal death, possibly due to the attenuation of toxic effects elicited by extracellular ATP (Varma et al. 2007).
Taken together, these results suggest that up-regulation of P2X7R is a common mechanism shared by various neurodegenerative diseases.
The Mechanism of the Up-regulation of P2X7R in Neurodegenerative Disease
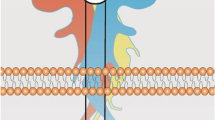
The mechanism of P2X7R up-regulation in neurodegenerative disease is unclear, but it may be closely related to the complicated role of microglia during the progression of such diseases (Fig. 1). It has been well characterized that microglia exert both protective and neurodegenerative roles in neurodegeneration. As macrophages, activated microglia may remove potentially deleterious debris and promote tissue repair, thus contributing to neuroprotection. However, over-activated microglia can release potentially neurotoxic substances, resulting in enhanced inflammation and leading to neurodegeneration (Garden and Moller 2006).
Mechanisms for the involvement of P2X7R in neurodegenerative disease. P2X7R is abundantly expressed in microglia and to a lesser extent in both neurons and astrocytes. Under physiological conditions, microglia may protect neurons through the regulation of synaptic transmission and astrocyte functions (a). Under pathological conditions, the expression levels of P2X7R are increased not only in microglia, but also in neurons and astrocytes. Over-activated microglia may release toxic amounts of cytokines and chemokines, leading to neuronal cell death. Microglia may also stimulate astrocytosis, resulting in synapse dysfunction and exitotoxicity (b)
Accumulating evidence suggests that aging may be a critical factor associated with the switching of microglia from a protective to a neurodegenerative role. Supporting this concept, age-dependent microglial activation has been demonstrated in various animal models of neurodegenerative diseases. For example, microglial activation was investigated in the brains of young (3 months) and older (9–12 months) C57BL/6 mice following treatment with 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP). MPTP is a chemical inducer of parkinsonian symptoms that acts through the killing of doperminergic neurons in the substantia nigra of the brain (Langston et al. 1983). The data demonstrated that robust microglial activation occurs in the substantia nigra in older mice (9–12 months), while less microglial activation was observed in young mice (3 months) (Sugama et al. 2003). In a transgenic mice model of AD, the phenotype of microglia shifts from the non-cytotoxic to the cytotoxic type depending on the age of the mice. At an early age (4–6 months), activated microglia are restricted to amyloid deposits and characterized by the absence of cytotoxic factors (Jimenez et al. 2008). In contrast, in older mice (18 months), activated microglia show a potentially cytotoxic phenotype expressing TNF-α, Fas-L, TRAIL, Cox2, and Nox1 (Jimenez et al. 2008).
Based on the age-dependent switch in the microglial phenotype, we speculate that up-regulation of P2X7R may be pathologically important during the late stages of neurodegeneration (Fig. 1). However, it is also possible that P2X7R is involved in non-cytotoxic physiological functions in the early stages of neurodegeneration. Further investigations are required to test these hypotheses.
Expression of P2X7R at the Pre-synaptic Sites of Neurons and Astrocytes
Although P2X7R is predominantly expressed in microglia, a recent study has shown that this receptor is also expressed in other cell types, including neurons and astrocytes.
While the involvement of the P2X family of receptors except for P2X7R in ATP-related neurotransmission has been well characterized (Norenberg and Illes 2000), the expression of P2X7R in neurons was disputed until recently (Sim et al. 2004). Evidence is accumulating for the functional expression of P2X7R in the central and peripheral pre-synaptic termini of neurons, which may be relevant to the modulation of transmitter release, including that of γ-aminobutyric acid and glutamate (Anderson and Nedergaard 2006). These results indicate that P2X7R plays important roles in the fundamental regulation of synaptic transmission at the pre-synaptic sites of neurons (Duan and Neary 2006).
P2X7R is also expressed in other cell types, including astrocytes and oligodendrocytes. Since astrocytes react with neurotransmitters released from the synapse due to intracellular Ca2+ elevations causing the release of glutamate (Duan et al. 2003), it is possible that ATP also affects synaptic function by modulation of glutamate release from astrocytes. Taken together, it is possible that impairment of P2X7R expression and function in both pre-synapse and astrocytes results in the dysregulation of neural transmission and the induction of excitotoxicity correlated with neurodegenerative diseases (Fig. 1). Future investigations are required to confirm this intriguing possibility.
Therapeutic Effects of P2X7R Antagonists in Animal Models of Neurodegenerative Disease
Since the up-regulation of the P2X7R system may stimulate neurodegenerative diseases, suppression of this receptor could be a therapeutic strategy for ameliorating the neurodegenerative process. Researchers previously found that oxidized ATP, a potent antagonist for P2X7R, could not cross the blood–brain barrier and had adverse effects on the heart. Conversely, a recent study showed that brilliant blue G (BBG) may be promising as an alternative for this purpose because it has similar pharmacological properties to oxidized ATP, can cross the blood–brain barrier, and has low toxicity. BBG is derived from a blue food dye called FD&C blue No. 1, which has been shown to be safe in healthy animals and is approved for use in foodstuffs (Borzelleca et al. 1990; Hess and Fitzhugh 1955).
In Aβ-42-injected rat hippocampi, marked increases in P2X7R expression, gliosis, leakiness of the blood–brain barrier, and hippocampal neuron loss were observed. The P2X7R antagonist BBG reduced the levels of purinergic receptor expression, attenuated gliosis, diminished the leakiness of the blood–brain barrier, and was neuroprotective (Ryu and McLarnon 2008). BBG also demonstrated neuroprotective and antagonistic effects against inflammatory responses induced by the P2X7R agonist 2′,3′-(benzoyl-4-benzoyl)-ATP (Ryu and McLarnon 2008). As with AD, in vivo administration of BBG to HD mice ameliorated the pathogenesis of HD by preventing neuronal apoptosis (Diaz-Hernandez et al. 2009). Similarly, BBG has been shown to exhibit beneficial effects on other animal models of CNS diseases, including spinal cord injury and multiple sclerosis (Matute et al. 2007; Peng et al. 2009).
The success of BBG in various animal studies suggests that P2X7R could be used as a therapeutic target for the treatment of neurodegenerative disease and related disorders. However, considering that relatively high concentrations of BBG (~50 mg/kg) have been used for these animal studies, it is yet to be determined whether non-toxic doses of BBG are effective for human patients suffering from chronic neurodegenerative diseases. Thus, further investigations may find new compounds that antagonize the P2X7R pathway more effectively than BBG. In addition to the pharmacological blockade of P2X7R, other strategies may be considered, such as the delivery of small RNA (e.g. micro RNA and small interfering RNA) into the brain to knock down the expression level of P2X7R. Such a strategy could be combined with treatments involving P2X7R antagonists to effectively suppress the P2X7R signaling pathway.
Concluding Remarks
A recent study suggested that the up-regulation of the P2X7R pathway could play a critical role in the progression of various neurodegenerative diseases. In addition to treatment with P2X7R antagonists, suppression of the P2X7R pathway could become a novel therapeutic approach for ameliorating neurodegenerative processes.
Abbreviations
- AD:
-
Alzheimer’s disease
- P2X7R:
-
P2X7 receptor
- Aβ:
-
Amyloid-β
- CNS:
-
Central nervous system
- IL-1β:
-
Interleukin-1β
- PrPSc :
-
Infectious form of prion protein
- HD:
-
Huntington’s disease
- BBG:
-
Brilliant blue G
References
Abbracchio MP, Burnstock G, Boeynaems JM et al (2006) International Union of Pharmacology LVIII: update on the P2Y G protein-coupled nucleotide receptors: from molecular mechanisms and pathophysiology to therapy. Pharmacol Rev 58:281–341
Anderson CM, Nedergaard M (2006) Emerging challenges of assigning P2X7 receptor function and immunoreactivity in neurons. Trends Neurosci 29:257–262
Bianco F, Ceruti S, Colombo A et al (2006) A role for P2X7 in microglial proliferation. J Neurochem 99:745–758
Borzelleca JF, Depukat K, Hallagan JB (1990) Lifetime toxicity/carcinogenicity studies of FD & C Blue No. 1 (brilliant blue FCF) in rats and mice. Food Chem Toxicol 28:221–234
Crozet C, Beranger F, Lehmann S (2008) Cellular pathogenesis in prion diseases. Vet Res 39:44
Denlinger LC, Fisette PL, Sommer JA et al (2001) Cutting edge: the nucleotide receptor P2X7 contains multiple protein- and lipid-interaction motifs including a potential binding site for bacterial lipopolysaccharide. J Immunol 167:1871–1876
Di Virgilio F, Chiozzi P, Falzoni S et al (1998) Cytolytic P2X purinoceptors. Cell Death Differ 5:191–199
Diaz-Hernandez M, Diez-Zaera M, Sanchez-Nogueiro J et al (2009) Altered P2X7-receptor level and function in mouse models of Huntington’s disease and therapeutic efficacy of antagonist administration. FASEB J 23:1893–1906
Duan S, Neary JT (2006) P2X(7) receptors: properties and relevance to CNS function. Glia 54:738–746
Duan S, Anderson CM, Keung EC et al (2003) P2X7 receptor-mediated release of excitatory amino acids from astrocytes. J Neurosci 23:1320–1328
Ferrari D, Villalba M, Chiozzi P et al (1996) Mouse microglial cells express a plasma membrane pore gated by extracellular ATP. J Immunol 156:1531–1539
Ferrari D, Chiozzi P, Falzoni S et al (1997a) ATP-mediated cytotoxicity in microglial cells. Neuropharmacology 36:1295–1301
Ferrari D, Chiozzi P, Falzoni S et al (1997b) Purinergic modulation of interleukin-1β release from microglial cells stimulated with bacterial endotoxin. J Exp Med 185:579–582
Ferrari D, Wesselborg S, Bauer MK et al (1997c) Extracellular ATP activates transcription factor NF-κB through the P2Z purinoreceptor by selectively targeting NF-κB p65. J Cell Biol 139:1635–1643
Ferrari D, Pizzirani C, Adinolfi E et al (2006) The P2X7 receptor: a key player in IL-1 processing and release. J Immunol 176:3877–3883
Fujita M, Wei J, Nakai M et al (2006) Chaperone and anti-chaperone: two-faced synuclein as stimulator of synaptic evolution. Neuropathology 26:383–392
Garden GA, Moller T (2006) Microglia biology in health and disease. J Neuroimmune Pharmacol 1:127–137
Gendron FP, Chalimoniuk M, Strosznajder J et al (2003) P2X7 nucleotide receptor activation enhances IFNγ-induced type II nitric oxide synthase activity in BV-2 microglial cells. J Neurochem 87:344–352
Hashimoto M, Masliah E (1999) α-synuclein in Lewy body disease and Alzheimer’s disease. Brain Pathol 9:707–720
Hess SM, Fitzhugh OG (1955) Absorption and excretion of certain triphenylmethane colors in rats and dogs. J Pharmacol Exp Ther 114:38–42
Iwamaru Y, Takenouchi T, Ogihara K et al (2007) Microglial cell line established from prion protein-overexpressing mice is susceptible to various murine prion strains. J Virol 81:1524–1527
Jiang LH (2009) Inhibition of P2X(7) receptors by divalent cations: old action and new insight. Eur Biophys J 38:339–346
Jimenez S, Baglietto-Vargas D, Caballero C et al (2008) Inflammatory response in the hippocampus of PS1M146L/APP751SL mouse model of Alzheimer’s disease: age-dependent switch in the microglial phenotype from alternative to classic. J Neurosci 28:11650–11661
Kataoka A, Tozaki-Saitoh H, Koga Y et al (2009) Activation of P2X7 receptors induces CCL3 production in microglial cells through transcription factor NFAT. J Neurochem 108:115–125
Kaur C, Hao AJ, Wu CH et al (2001) Origin of microglia. Microsc Res Tech 54:2–9
Langston JW, Ballard P, Tetrud JW et al (1983) Chronic parkinsonism in humans due to a product of meperidine-analog synthesis. Science 219:979–980
Matute C, Torre I, Perez-Cerda F et al (2007) P2X(7) receptor blockade prevents ATP excitotoxicity in oligodendrocytes and ameliorates experimental autoimmune encephalomyelitis. J Neurosci 27:9525–9533
McLarnon JG, Ryu JK, Walker DG et al (2006) Upregulated expression of purinergic P2X(7) receptor in Alzheimer disease and amyloid-beta peptide-treated microglia and in peptide-injected rat hippocampus. J Neuropathol Exp Neurol 65:1090–1097
Monif M, Reid CA, Powell KL et al (2009) The P2X7 receptor drives microglial activation and proliferation: a trophic role for P2X7R pore. J Neurosci 29:3781–3791
Norenberg W, Illes P (2000) Neuronal P2X receptors: localisation and functional properties. Naunyn Schmiedebergs Arch Pharmacol 362:324–339
North RA (2002) Molecular physiology of P2X receptors. Physiol Rev 82:1013–1067
Parvathenani LK, Tertyshnikova S, Greco CR et al (2003) P2X7 mediates superoxide production in primary microglia and is up-regulated in a transgenic mouse model of Alzheimer’s disease. J Biol Chem 278:13309–13317
Peng W, Cotrina ML, Han X et al (2009) Systemic administration of an antagonist of the ATP-sensitive receptor P2X7 improves recovery after spinal cord injury. Proc Natl Acad Sci USA 106:12489–12493
Prusiner SB (1991) Molecular biology of prion diseases. Science 252:1515–1522
Ryu JK, McLarnon JG (2008) Block of purinergic P2X(7) receptor is neuroprotective in an animal model of Alzheimer’s disease. Neuroreport 19:1715–1719
Sanz JM, Chiozzi P, Ferrari D et al (2009) Activation of microglia by amyloid β requires P2X7 receptor expression. J Immunol 182:4378–4385
Selkoe DJ (1996) Amyloid β-protein and the genetics of Alzheimer’s disease. J Biol Chem 271:18295–18298
Sim JA, Young MT, Sung HY et al (2004) Reanalysis of P2X7 receptor expression in rodent brain. J Neurosci 24:6307–6314
Sugama S, Yang L, Cho BP et al (2003) Age-related microglial activation in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced dopaminergic neurodegeneration in C57BL/6 mice. Brain Res 964:288–294
Sugama S, Takenouchi T, Cho BP et al (2009) Possible roles of microglial cells for neurotoxicity in clinical neurodegenerative diseases and experimental animal models. Inflamm Allergy Drug Targets 8:277–284
Surprenant A, Rassendren F, Kawashima E et al (1996) The cytolytic P2Z receptor for extracellular ATP identified as a P2X receptor (P2X7). Science 272:735–738
Suzuki T, Hide I, Ido K et al (2004) Production and release of neuroprotective tumor necrosis factor by P2X7 receptor-activated microglia. J Neurosci 24:1–7
Takenouchi T, Ogihara K, Sato M et al (2005) Inhibitory effects of U73122 and U73343 on Ca2+ influx and pore formation induced by the activation of P2X7 nucleotide receptors in mouse microglial cell line. Biochim Biophys Acta 1726:177–186
Takenouchi T, Iwamaru Y, Imamura M et al (2007a) Prion infection correlates with hypersensitivity of P2X7 nucleotide receptor in a mouse microglial cell line. FEBS Lett 581:3019–3026
Takenouchi T, Sato M, Kitani H (2007b) Lysophosphatidylcholine potentiates Ca2+ influx, pore formation and p44/42 MAP kinase phosphorylation mediated by P2X7 receptor activation in mouse microglial cells. J Neurochem 102:1518–1532
Takenouchi T, Iwamaru Y, Sugama S et al (2008) Lysophospholipids and ATP mutually suppress maturation and release of IL-1β in mouse microglial cells using a Rho-dependent pathway. J Immunol 180:7827–7839
Takenouchi T, Nakai M, Iwamaru Y et al (2009a) The activation of P2X7 receptor impairs lysosomal functions and stimulates the release of autophagolysosomes in microglial cells. J Immunol 182:2051–2062
Takenouchi T, Sugama S, Iwamaru Y et al (2009b) Modulation of the ATP-induced release and processing of IL-1β in microglial cells. Crit Rev Immunol 29:335–345
The Huntington’s Disease Collaboratine Research Group (1993) A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington’s disease chromosomes. Cell 72:971–983
Varma H, Cheng R, Voisine C et al (2007) Inhibitors of metabolism rescue cell death in Huntington’s disease models. Proc Natl Acad Sci USA 104:14525–14530
Acknowledgments
This work was supported by a grant-in-aid from the Japanese Ministry of Education, Culture, Sports, Science, and Technology. This work was also supported by a research grant from the Takeda Science Foundation.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Takenouchi, T., Sekiyama, K., Sekigawa, A. et al. P2X7 Receptor Signaling Pathway as a Therapeutic Target for Neurodegenerative Diseases. Arch. Immunol. Ther. Exp. 58, 91–96 (2010). https://doi.org/10.1007/s00005-010-0069-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00005-010-0069-y